Abstract
Hepcidin is an antimicrobial peptide that controls systemic iron homeostasis. Hepcidin binding to its receptor ferroportin reduces iron availability, thus controlling microbial growth. In parallel it triggers an anti-inflammatory response in macrophages. Hepcidin is transcriptionally regulated by iron, through the bone morphogenetic protein–son of mothers against decapentaplegic (BMP-SMAD) pathway and by inflammation, through IL6-mediated STAT3 signaling. To investigate the mechanisms linking iron and inflammation, we treated C57BL/6 iron-deficient mice with a sublethal dose of lipopolysaccharide (LPS) and analyzed their inflammatory response in comparison with controls. We show that iron-deprived mice have a proinflammatory condition, exacerbated by LPS treatment leading to increased IL6 and TNFα mRNA in liver and spleen macrophages, and increased serum IL6 (482.29 ± 205.59 pg/mL) versus controls (69.01 ± 17.52 pg/mL; P < .05). Hepcidin was undetectable in iron-deficient mice but pretreatment with hepcidin normalized their response to LPS. Tmprss6−/− mice, characterized by iron deficiency and high hepcidin, show a blunted inflammatory response when challenged with LPS. Our data support a model in which the lack of hepcidin is responsible of the high inflammatory response to LPS in iron deficiency. The proinflammatory status associated with chronic iron deficiency could explain the resistance to infection seen in this condition.
Introduction
The peptide hepcidin is the central regulator of body iron homeostasis. Hepcidin binding to the iron exporter ferroportin causes its internalization and degradation, reducing iron release from macrophages, duodenal cells, and hepatocytes.1 Hepcidin synthesis is regulated by changes in body iron stores, erythropoietic needs, and inflammation. The bone morphogenetic protein–son of mothers against decapentaplegic ((BMP-SMAD) pathway up-regulates hepcidin transcription in response to increased body iron. Binding of BMP6 to its receptors (BMPRs) in the presence of the coreceptor hemojuvelin (HJV) activates SMAD signaling. Phosphorylated SMAD1/5/8 form a heterodimeric complex with SMAD4 in the cytoplasm that translocates to the nucleus to activate target genes including hepcidin.2,3 Inactivation of genes that directly (HJV, BMP6) or indirectly (HFE, TfR2) regulate BMP-SMAD signaling, impairs hepcidin production, and causes iron overload in humans4 and mice.5-9
Hepcidin is also an antimicrobial peptide,10 and its expression is induced by infection/inflammation. Although hepcidin has direct antimicrobial activity in vitro,10 the antimicrobial effect of hepcidin in vivo is usually ascribed to its ability to decrease the availability of circulating iron which is a growth factor for invading pathogens. Lipopolysaccharide (LPS) and the central cytokine of inflammation IL6 increase hepcidin mRNA through phosphorylation of STAT3.11,12 Sustained up-regulation of IL6 in chronic inflammation and the consequent increase of hepcidin are responsible for the anemia of chronic diseases,13,14 which is because of iron-restricted erythropoiesis. The hepcidin promoter has a STAT3–responsive site (STAT3-RS) at position −72/−64 in close proximity of a BMP–responsive element (BMP-RE1) at position −87/−79.15 Although STAT3-RS inactivation does not alter the BMP-mediated response of hepcidin, mutations of BMP-RE1 strongly down-regulate IL6-mediated hepcidin activation, suggesting that the integrity of the BMP-SMAD pathway is required to activate hepcidin.15 This is confirmed by the lack of an increase in hepcidin in response to IL6 in liver-specific conditional Smad4-deficient mice.7 However, the cross-talk between the 2 (iron and cytokine-dependent) pathways of hepcidin up-regulation remains incompletely understood.
It is well accepted that iron deficiency confers resistance to a variety of microbes.16 The molecular basis of the iron-dependent response to infection is not completely defined. In conditions of iron deficiency, the production of hepcidin is suppressed. Besides controlling iron availability to microbes, hepcidin is a candidate regulator of the cross-talk between iron intake and inflammation because it activates in macrophages a JAK2-mediated intracellular signaling pathways that curbs the production of inflammatory cytokines triggered by LPS.17
Here we show that persistent iron deficiency in mice induces a proinflammatory state and a stronger inflammatory response to LPS compared with mice with normal iron stores. The LPS-induced inflammation of iron-deficient mice can be suppressed by pretreatment with exogenous hepcidin. The effect is independent of hepcidin's function on iron metabolism becauseTmprss6−/− mice which are characterized by iron-deficiency anemia and a paradoxically high production of hepcidin, and have a blunted inflammatory response compared with mice rendered iron deficient (ID) through exposure to an ID diet. The data imply that lack of hepcidin in iron deficiency is responsible for enhanced systemic inflammation.
Methods
Animals, diet, and tissue collections
C57BL/6 male mice, obtained from Charles River, and Tmprss6−/− mice, on a mixed 129/Ola × C57BL/6 background,18 were maintained in the animal facility of the San Raffaele Scientific Institute in accordance with the European Union guidelines. The study was approved by the institutional animal care and use committee of our institution. Four-week-old male mice were fed an iron-balanced diet (carbonile iron 200 mg/kg; SAFE) or an iron-deficient diet, with virtually no iron content (< 3 mg iron/kg; SAFE) for 3 weeks, as previously described.19 When indicated, 100 μg of hepcidin or sterile PBS, were IP-injected in mice, 2 hours before LPS treatment. Inflammation was induced by IP injection of LPS (from Escherichia coli O26:B6; 0.1 mg/kg, IP; Sigma-Aldrich). Control mice were injected with sterile saline solution. Mice were killed 6 hours later. Livers and spleen were either snap-frozen for Western blot analyses and isolation of RNA or were processed immediately for isolation of tissue macrophages and for tissue iron measurements (see “Isolation of resident macrophages”).
Hematologic and iron parameters
Blood (0.2 mL) was extracted by a single caudal puncture from anesthetized mice. Blood cell counts and erythrocyte parameters were determined using the Sysmex KX-21 automated blood cell analyzer (Sysmex America). Transferrin saturation (TS) was calculated as a ratio of serum iron and total iron binding capacity levels (Randox Laboratories Ltd).
To measure iron concentration, tissue samples were dried at 110°C overnight, and 20 mg were digested in 1 mL of acid solution (3M HCl, 0.6M TCA) for 20 hours at 65°C. The cleared acid extract was added to 1 mL of working chromogen reagent (1 volume of 0.1% bathophenanthroline sulfate and 1% thioglycolic acid solution, 5 volumes of water, and 5 volumes of saturated sodium acetate). The solutions were then incubated for 30 minutes at room temperature until color development and the absorbance was measured at 535 nm. A standard curve was plotted using the acid solution containing increasing amounts of iron diluted from a stock solution of Titrisol iron standard (Merck).
Western blot analysis
Livers were homogenized and lysed in lysis buffer (200mM Tris-HCl [pH 8]; 1mM EDTA; 100mM NaCl; 10% glycerol; 0.5% NP-40). Proteins were quantified using the Bio-Rad Protein Assay (Bio-Rad) according to the manufacturer's instructions. Protein extracts (50 μg) were diluted in Laemmli buffer, incubated 5 minutes at 95°C, and subjected to 10% SDS-PAGE and then transferred to Hybond C membrane (Amersham Bioscience Europe GmbH) by standard Western blot technique. Blots were blocked with 5% nonfat milk in TBS (0.5M Tris-HCl [pH 7.4] and 0.15M NaCl) containing 0.1% Tween 20 (TBST), incubated overnight with anti-phospho-SMAD1/5/8 (1:1000; Cell Signaling; Millipore), anti-SMAD5 (1:1000; Cell Signaling), anti-phospho-STAT3 (1:1000; Cell Signaling), anti-STAT3 (1:2000; Cell Signaling), anti-TfR1 (1:1000; Zymed), anti-tubulin (1:1000; Santa Cruz Biotechnology) in TBST containing 5% BSA. After washing with TBST, blots were incubated 1 hour with relevant HRP-conjugated antisera in TBST with 5% nonfat milk and developed using a chemoluminescence detection kit (ECL; Amersham Biosciences).
Isolation of resident macrophages
Splenic macrophages were isolated from treated and untreated animals from whole spleen using MACS CD11b MicroBeads (Miltenyi Biotec GmbH) according to the manufacturer's instructions.
Liver macrophages were isolated as described.20 Briefly, mice were killed and livers were perfused in situ through the inferior vena cava with a 0.03% collagenase type IV (Sigma-Aldrich)–HBSS solution (Life Technologies) after transection of the portal vein. After perfusion, livers were removed and gently teased with forceps. Cell suspensions were filtered through a nylon gauze and then centrifuge at 25g for 3 minutes. The resulting pellets were washed 3 times, supernatants were collected and centrifuged at 650g for 7 minutes. Pellets, containing mainly nonparenchymal (macrophages and stellate) cells, were resuspended in HBSS (Life Technologies) and layered onto a 50%-25% 2-step Percoll gradient and then centrifuged 15 minutes at 1500g. Middle layers were collected, cells were separated by centrifugation, and macrophages were isolated using MACS CD11b MicroBeads (Miltenyi Biotec).
Spleen- and liver-isolated macrophages from each group (4 mice per group) were pooled and then analyzed by quantitative RT-PCR (qRT-PCR) and flow cytometry (see next section).
qRT-PCR
Tissue samples were stored in RNALater (QIAGEN), and total RNA was extracted with TRIzol reagent (Invitrogen). Two micrograms of total RNA were retro-transcribed with the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems), using random hexamers and RNase inhibitor. Gene expression levels were measured by quantitative real-time PCR in a ABI7900 Real-Time PCR System (Applied Biosystems) using TaqMan Gene Expression Master Mix (Applied Biosystems) or SybrGreen PCR Master Mix (Applied Biosystems). Primers used for qRT-PCR are indicated in supplemental Tables 1 and 2 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Tissue digestion and flow cytometry
Carefully minced livers, resuspended in 0.5 mg/mL collagenase type IV (Sigma-Aldrich) and 60 U/mL DNAse I (Roche) in 1× PBS+ (Life Technologies), underwent 4 cycles of enzymatic digestion at 37°C for 10 minutes. After digestion, samples were passed through 40-μm filters and the single-cell suspension was processed for flow cytometry. Spleens were harvested and total splenocytes were processed for flow cytometry. Briefly, cells were resuspended in 1× cold PBS− containing 2mM EDTA, then incubated with APC-conjugated anti-CD11b mAb (clone M1/70; BD Biosciences), PerCP-conjugated anti-CD45 mAb (clone 30-F11; BD Pharmingen), and PE-conjugated anti-F4/80 mAb (clone MCA497EL; AbD Serotec) to select macrophage populations. Staining with a rabbit anti–mouse CD163 mAb (clone M-96; Santa Cruz Biotechnology), followed by secondary staining with polyclonal APC-conjugated goat anti–rabbit Ab (Southern Biotechnology Associates), FITC-conjugated anti–mouse CD86 (clone GLI; BD Biosciences), PE-conjugated anti–mouse CD206 mAb (clone MR5D3; Serotec), and FITC-conjugated anti–mouse I-Ab (clone C3H.SW; BD Biosciences) was performed to evaluate macrophages polarization. All Abs were diluted in PBS 10% FBS. After washing, cells were analyzed on a FACSCanto (BD Pharmingen). Analyses were performed with the FlowJo software (Treestar Inc).
Serum IL6 levels
Serum was obtained by centrifugation of blood, kept 2 hours at room temperature after caudal puncture. Serum IL6 was analyzed using Mouse IL6 ELISA Ready-Set-Go! (eBioscience) according to the manufacturer's instructions.
Statistical analyses
The unpaired 2-tailed Student t test was used to analyze significant changes in the described parameters (GraphPad Prism Version 5.0a). P values < .05 were considered statistically significant.
Results
Hematologic and iron parameters of ID mice
Four-week-old male mice were fed an ID diet for 3 weeks and then treated with a single sublethal dose (0.1 mg/kg IP) of LPS. Mice were killed 6 hours later. Mice developed moderate iron deficiency as shown by the parameters listed in Table 1. Injection of LPS has little effect on the hematologic parameters of ID mice. TS declined after LPS challenge in iron-replete (IR) controls but was unchanged from the low basal levels in ID mice. A significant increase of liver non-heme iron (LIC) was observed in IR mice treated with LPS (Table 1) as expected because of the autocrine effects of high hepcidin on degradation of hepatic ferroportin (Fpn).21 No differences in the low basal non-heme iron levels were detected in ID mice. As expected, liver transferrin receptor 1 (TfR1) was up-regulated, both at mRNA (supplemental Figure1A) and protein (supplemental Figure1B) levels, and Fpn mRNA was down-regulated (supplemental Figure1C) in ID mice. LPS strongly inhibited Fpn mRNA expression, as previously reported,22 but did not affect liver TfR1 levels in ID mice or in IR controls.
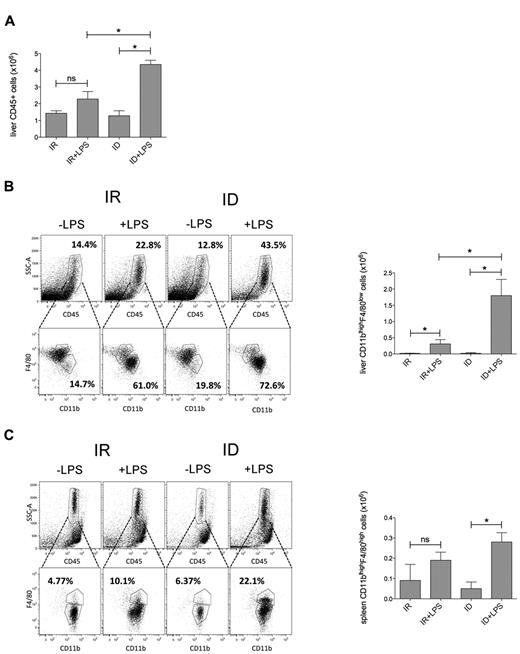
Iron deficiency modulates LPS-induced recruitment of spleen and liver macrophages and the induction of inflammatory cytokines
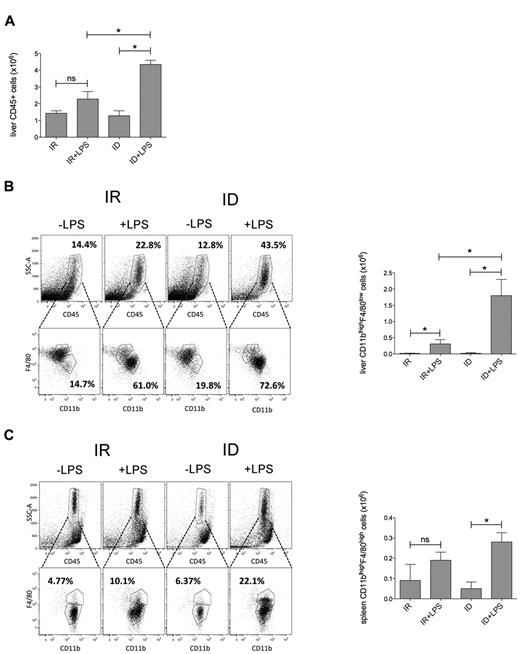
Under basal conditions ID mice had higher white blood cell (WBC) count than control mice (Table 1). LPS treatment caused a marked WBC decrease in both animal groups (Table 1) because of WBC peripheral recruitment as previously reported.23,24 To investigate whether iron deficiency modulates leukocyte recruitment, the total number of CD45+ (WBC) cells and CD45+CD11b+/F4/80+ macrophages retrieved from the liver and spleen of control and ID mice were evaluated by flow cytometry. LPS administration increased CD45+ (Figure 1A) and CD45+CD11b+/F4/80+ cell frequency in livers (Figure 1B) and spleens (Figure 1C) of both ID mice and IR controls, although the recruitment in the liver was more prominent in ID than in IR mice. As shown in Table 2, the expression of CD163 (the hemoglobin/haptoglobin scavenger receptor) was higher in ID mice (compatible with the condition of iron deficiency)25 and was not affected by treatment with LPS. The expression of the mannose scavenger receptor CD206 was equivalent in all conditions. LPS led to an up regulation of markers of macrophage activation (MHC class II molecules and the costimulatory molecule CD86) whose expression was consistently higher in ID mice (Table 2).
Increased macrophage recruitment in LPS-treated ID mice. (A) Absolute number of leukocytes (CD45+) analyzed in total liver of IR and ID mice under basal condition or after LPS injection (4 mice for each group). Frequency (left panel) and absolute number (right panel) of inflammatory macrophages (CD45+CD11b+F480+), isolated as described in “Tissue digestion and flow cytometry,” were analyzed in liver (B) and spleen (C) of IR and ID mice treated with or without LPS (4 mice for each group) 6 hours before sacrifice. Error bars indicate SE; *P < .05.
Increased macrophage recruitment in LPS-treated ID mice. (A) Absolute number of leukocytes (CD45+) analyzed in total liver of IR and ID mice under basal condition or after LPS injection (4 mice for each group). Frequency (left panel) and absolute number (right panel) of inflammatory macrophages (CD45+CD11b+F480+), isolated as described in “Tissue digestion and flow cytometry,” were analyzed in liver (B) and spleen (C) of IR and ID mice treated with or without LPS (4 mice for each group) 6 hours before sacrifice. Error bars indicate SE; *P < .05.
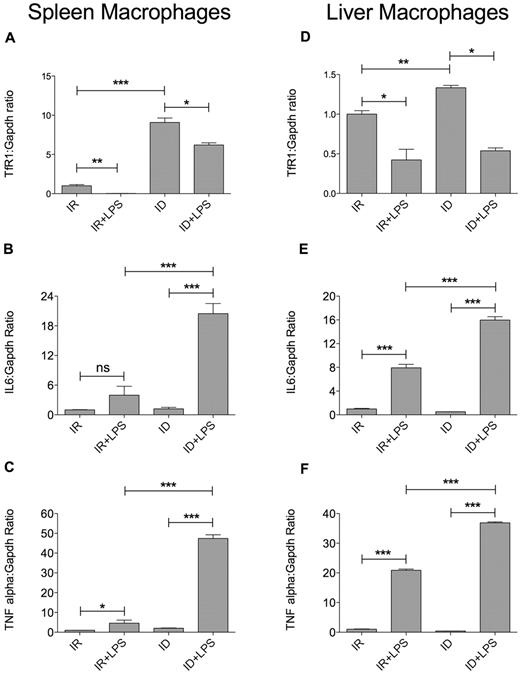
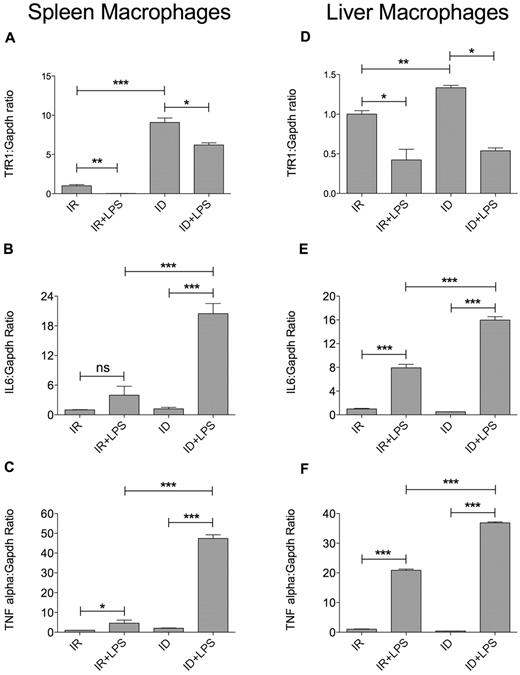
Spleen and liver macrophages were also analyzed for the expression of TfR1 and inflammatory cytokines. TfR1 mRNA, measured by qRT-PCR, was high in ID mice as expected and down-regulated on LPS stimulation both in IR and ID mice (Figure 2A,D). IL6 (Figure 2B), TNFα (Figure 2C), and IL1β (supplemental Figure 2A) mRNA were strongly induced by LPS in spleen macrophages isolated from ID mice, compared with IR controls. Similar results were obtained in liver-derived macrophages: there was a strong up-regulation of IL6 (Figure 2E), TNFα (Figure 2F) and IL1β (supplemental Figure2B) in ID mice treated with LPS.
Increased inflammatory response in splenic and hepatic macrophages from LPS-treated ID mice. Splenic and liver macrophages were isolated from IR and ID mice treated or not with LPS (4 mice for each group), as described in “Isolation of resident macrophages.” TfR1 (A,D), IL6 (B,E), and TNFα (C,F) mRNA expression was quantified by SybrGreen qRT-PCR. Gapdh was used as the housekeeping gene. mRNA expression ratio was normalized to an IR mean value of 1. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
Increased inflammatory response in splenic and hepatic macrophages from LPS-treated ID mice. Splenic and liver macrophages were isolated from IR and ID mice treated or not with LPS (4 mice for each group), as described in “Isolation of resident macrophages.” TfR1 (A,D), IL6 (B,E), and TNFα (C,F) mRNA expression was quantified by SybrGreen qRT-PCR. Gapdh was used as the housekeeping gene. mRNA expression ratio was normalized to an IR mean value of 1. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
In further support to the proinflammatory status of ID mice, the serum levels of IL6 were significantly higher (P < .05) in LPS-treated ID mice (482.29 ± 205.59 pg/mL) compared with LPS-treated IR mice (69.01 ± 17.52 pg/mL).
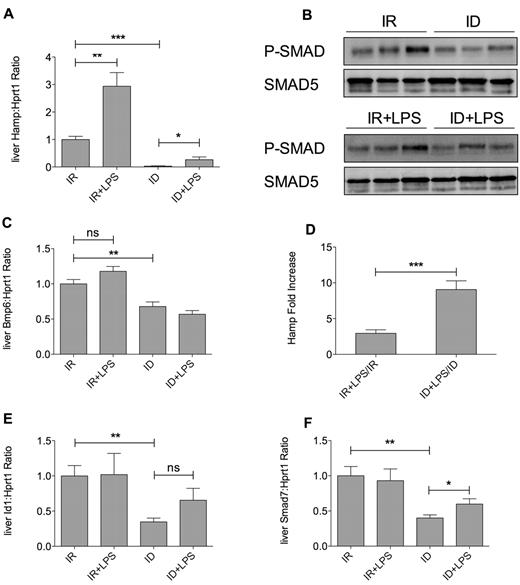
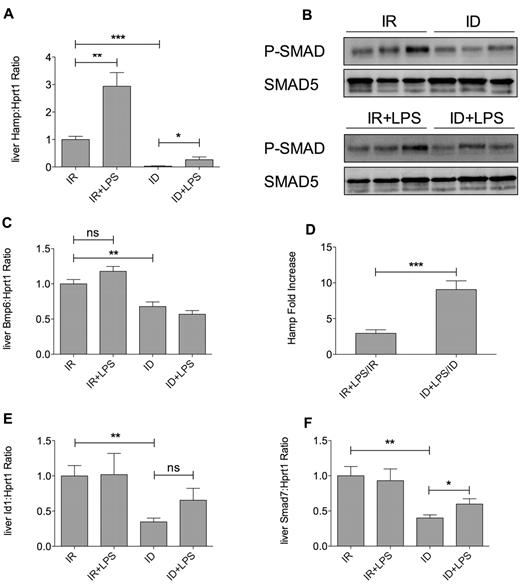
Down-regulation of the BMP-SMAD signaling in iron deficiency impairs the LPS-mediated hepcidin activation
Because hepcidin may represent a link between iron metabolism and inflammation, we measured hepcidin production in both ID and IR mice. As expected, hepcidin mRNA levels were strongly down-regulated in ID (Figure 3A) because of inactivation of the BMP-SMAD pathway (Figure 3B, supplemental Figure 2C), likely as a consequence of Bmp6 mRNA reduction (Figure 3C). LPS increased hepcidin mRNA in both ID and IR controls (Figure 3A). Interestingly, the fold increase of LPS-mediated hepcidin transcription was significantly higher in ID mice (Figure 3D), although the expression levels were below those observed in control mice. The BMP-SMAD signaling pathway was only slightly affected by inflammatory stimuli: indeed mRNA levels of the BMP-SMAD downstream gene, inhibitor of DNA binding 1 (Id1; Figure 3E) was unchanged and the level of hepatic phosphorylated SMAD1/5/8 were comparable between untreated and LPS-treated mice (Figure 3B, supplemental Figure 2C). The BMP coreceptor hemojuvelin (Hjv) was down-regulated after LPS treatment (supplemental Figure 2D), as reported.5 However, SMAD7, which has been related to the inflammatory pathway,26 was slightly increased in ID mice after LPS injection (Figure 3F).
LPS does not modify the BMP-SMAD pathway in ID and control mice. (A) Liver expression of hepcidin (Hamp) mRNA measured by TaqMan–qRT-PCR in 7-week-old mice (10 mice for each group). (B) Analysis of liver SMAD protein activation. Livers were dissociated as described in “Western blot analysis”; extracts were subjected to SDS-PAGE and Western blotted for phospho-SMAD1/5/8 and SMAD5 to normalize gel loading. A representative Western blot is shown. (C) Liver bone morphogenetic protein 6 (Bmp6) expression measured as in panel A. (D) Hamp fold-increase activation by LPS calculated as a ratio between the value of LPS-treated and untreated animals both in IR and ID mice. Liver inhibitor of DNA binding 1 (Id1; E) and Smad7 (F) mRNA expression measured by TaqMan qRT-PCR (10 mice for each group). Hypoxanthine phosphoribosyltransferase 1 (Hprt1) was used as the housekeeping gene to normalize gene expression. mRNA expression ratio was normalized to an IR mean value of 1. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
LPS does not modify the BMP-SMAD pathway in ID and control mice. (A) Liver expression of hepcidin (Hamp) mRNA measured by TaqMan–qRT-PCR in 7-week-old mice (10 mice for each group). (B) Analysis of liver SMAD protein activation. Livers were dissociated as described in “Western blot analysis”; extracts were subjected to SDS-PAGE and Western blotted for phospho-SMAD1/5/8 and SMAD5 to normalize gel loading. A representative Western blot is shown. (C) Liver bone morphogenetic protein 6 (Bmp6) expression measured as in panel A. (D) Hamp fold-increase activation by LPS calculated as a ratio between the value of LPS-treated and untreated animals both in IR and ID mice. Liver inhibitor of DNA binding 1 (Id1; E) and Smad7 (F) mRNA expression measured by TaqMan qRT-PCR (10 mice for each group). Hypoxanthine phosphoribosyltransferase 1 (Hprt1) was used as the housekeeping gene to normalize gene expression. mRNA expression ratio was normalized to an IR mean value of 1. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
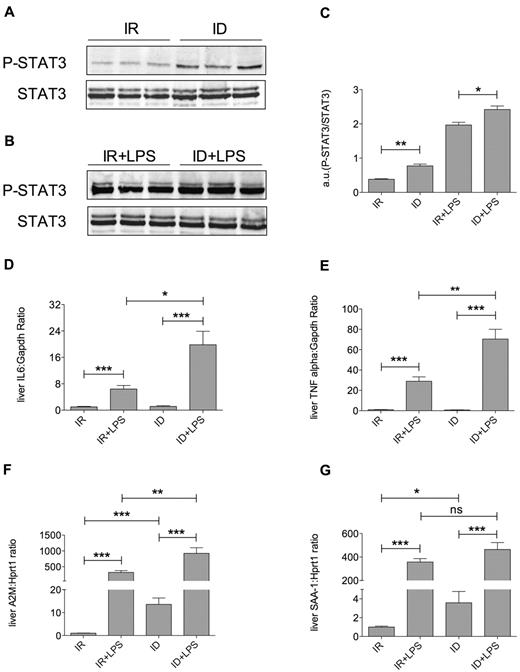
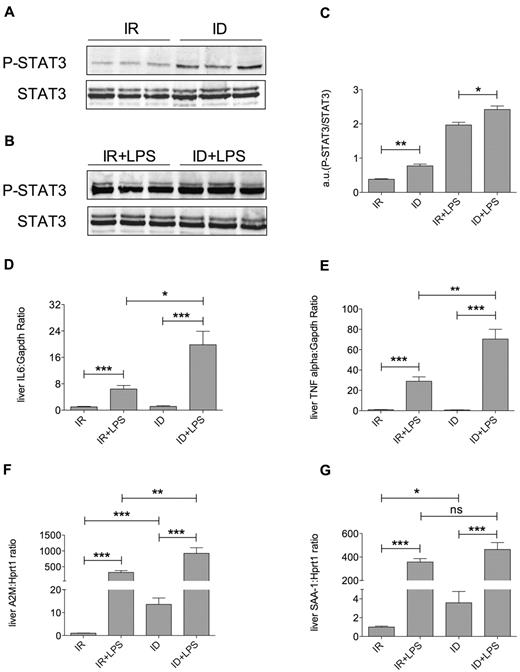
Increased liver STAT3 and acute-phase proteins in ID mice
The fold change of hepcidin increase observed on LPS treatment in ID mice (Figure 3D) is in agreement with the increased recruitment of inflammatory macrophages in liver and spleen (Figure 1). Accordingly, liver STAT3, an effector of the inflammatory pathway, was in the active form in untreated ID mice (Figure 4A,C) and was further phosphorylated on LPS challenge (Figure 4B-C). STAT3 was barely detected in untreated controls and strongly increased after LPS treatment. In addition, IL6 (Figure 4D), TNFα (Figure 4E), and IL1β (supplemental Figure 2E) mRNA were strongly induced in ID mice treated with LPS and, accordingly, liver acute-phase markers such as alpha-2 macroglobulin (A2M; Figure 4F) and serum amyloid A1 (SAA-1; Figure 4G) were significantly up-regulated in ID and further increased on LPS challenge.
Iron deficiency induces a proinflammatory condition. (A-B) Analysis of liver STAT3 activation. Livers were dissociated as described and protein extracts were subjected to SDS-PAGE and Western blotted for phospho-STAT3 and STAT3 to normalize gel loading. A representative Western blot is shown. (C) The level of STAT3 phosphorylation was quantified by densitometric analysis of phospho-STAT3 normalized to STAT3. Hepatic expression of the inflammatory cytokines IL6 (D) and TNFα (E), measured by SybrGreen qRT-PCR, and of acute-phase proteins A2M (F) and serum amyloid A-1 (SAA-1; G), measured by TaqMan qRT-PCR (10 mice each group). Gapdh (SybrGreen qRT-PCR) or Hprt1 (TaqMan qRT-PCR) were used as housekeeping genes to normalize gene expression. mRNA expression ratio was normalized to an IR mean value of 1. a.u. indicates arbitrary unit. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
Iron deficiency induces a proinflammatory condition. (A-B) Analysis of liver STAT3 activation. Livers were dissociated as described and protein extracts were subjected to SDS-PAGE and Western blotted for phospho-STAT3 and STAT3 to normalize gel loading. A representative Western blot is shown. (C) The level of STAT3 phosphorylation was quantified by densitometric analysis of phospho-STAT3 normalized to STAT3. Hepatic expression of the inflammatory cytokines IL6 (D) and TNFα (E), measured by SybrGreen qRT-PCR, and of acute-phase proteins A2M (F) and serum amyloid A-1 (SAA-1; G), measured by TaqMan qRT-PCR (10 mice each group). Gapdh (SybrGreen qRT-PCR) or Hprt1 (TaqMan qRT-PCR) were used as housekeeping genes to normalize gene expression. mRNA expression ratio was normalized to an IR mean value of 1. a.u. indicates arbitrary unit. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
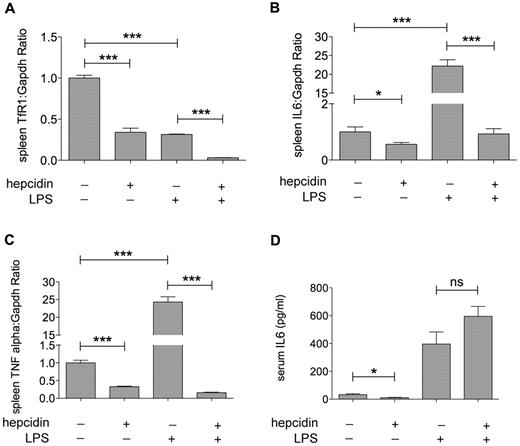
Hepcidin injection attenuates the LPS-mediated increase of inflammatory cytokines in ID mice
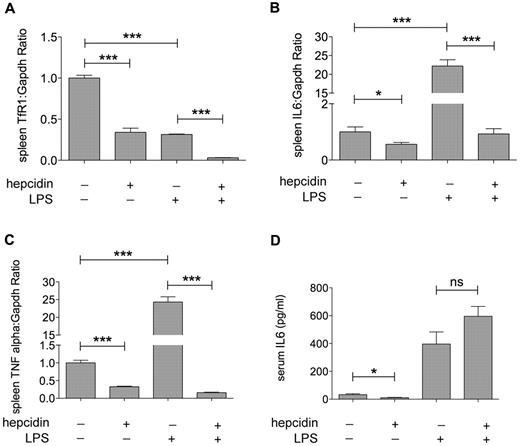
Recently, hepcidin has been shown to exert an anti-inflammatory role in macrophages after binding surface ferroportin.17 We hypothesized that the proinflammatory condition observed in ID mice was because of the lack of this hepcidin effect. To demonstrate this possibility, mice fed an ID diet were pretreated with 100 μg of endotoxin-free hepcidin17 and 2 hours later were injected with LPS. Six hours later, animals were killed and inflammatory cytokines were measured by qRT-PCR in splenic macrophages and in total liver. Hepcidin pretreatment reduced Tfr1 mRNA levels (Figure 5A) in spleen-derived macrophages, indirectly confirming the increased intracellular iron content after hepcidin-mediated ferroportin degradation. Pretreatment with hepcidin down-regulated IL6 (Figure 5B) and TNFα (Figure 5C) mRNA in ID mice. Hepcidin injection significantly decreased the LPS induction of cytokines (Figure 5B-C) in spleen-derived macrophages, but the protocol followed did not detect a decrease in serum IL6 (Figure 5D), suggesting that 6 hours is not a sufficient time to observe a change of the amount of the secreted protein.27 We observed only a mild decrease of the 2 inflammatory cytokines in mice preinjected with hepcidin and challenged with LPS (supplemental Figure 3A-B). However, the reduction did not reach statistical significance probably because of a dilution effect because the 2 cytokines were measured in total liver and not in isolated macrophages.
Hepcidin pretreatment blunts the LPS-mediated inflammatory response. TfR1 (A), IL6 (B), and TNFα (C) mRNA were analyzed by SybrGreen qRT-PCR in spleen macrophages isolated from ID mice pretreated with hepcidin (100 μg) or PBS before LPS injection (4 mice for each group). Gapdh was used as housekeeping gene to normalize gene expression. mRNA expression ratio was normalized to an ID (-hepcidin, -LPS) mean value of 1. (D) Serum IL6 levels were measured as described in “Serum IL6 levels” (4 mice for each group). Error bars indicate SE; *P < .05; and ***P < .0001.
Hepcidin pretreatment blunts the LPS-mediated inflammatory response. TfR1 (A), IL6 (B), and TNFα (C) mRNA were analyzed by SybrGreen qRT-PCR in spleen macrophages isolated from ID mice pretreated with hepcidin (100 μg) or PBS before LPS injection (4 mice for each group). Gapdh was used as housekeeping gene to normalize gene expression. mRNA expression ratio was normalized to an ID (-hepcidin, -LPS) mean value of 1. (D) Serum IL6 levels were measured as described in “Serum IL6 levels” (4 mice for each group). Error bars indicate SE; *P < .05; and ***P < .0001.
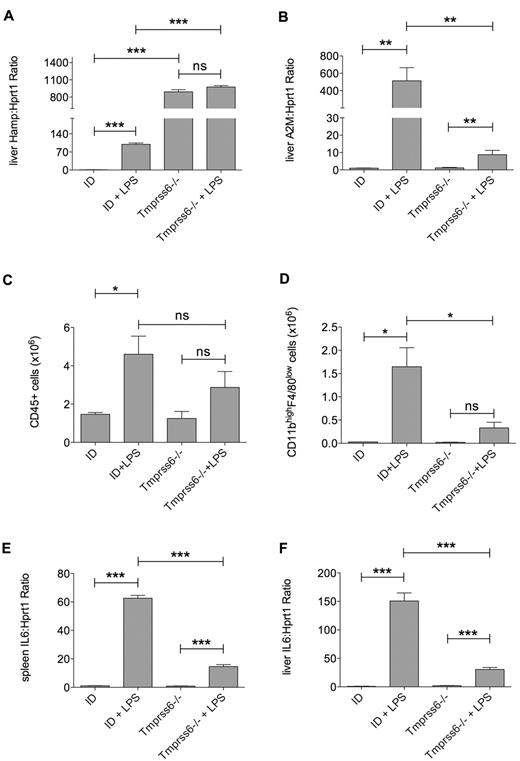
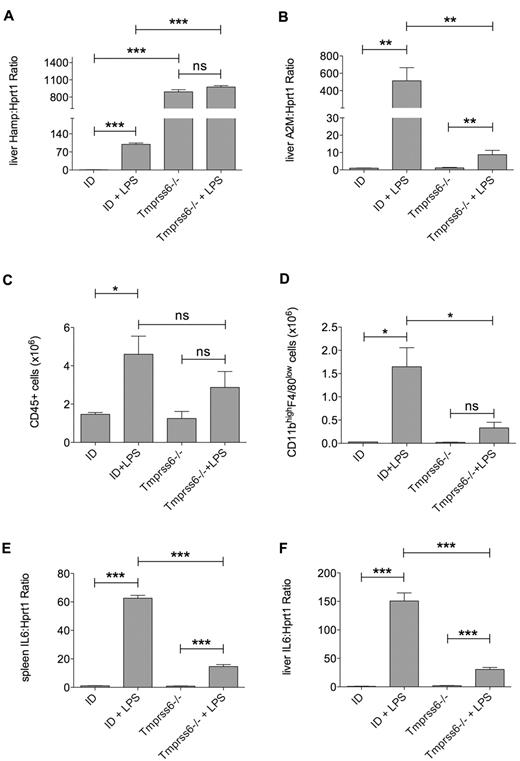
Blunted inflammatory response of Tmprss6−/− mice
To unequivocally discriminate between the contribution of iron deficiency and that of lack of hepcidin to the inflammatory state observed in ID, we took advantage of the Tmprss6−/− mouse,18,28 as in these animals severe iron deficiency coexists with inappropriately high hepcidin levels.18,29 Tmprss6−/− mice fed a normal diet were compared with age-matched littermates fed an iron-poor diet for 3 weeks. Tmprss6−/− mice had more severe iron deficiency than wild-type ID littermates, as shown by lower hemoglobin (Hgb), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH; Table 3). As expected, liver hepcidin mRNA was almost undetectable in ID mice and strongly up-regulated by LPS. In contrast, hepcidin was highly expressed in Tmprss6−/− mice and was LPS insensitive (Figure 6A). Liver acute-phase protein A2M mRNA levels (Figure 6B) and SAA-1 (not shown) were less induced by LPS in mutant Tmprss6−/− compared with ID mice.
Decreased inflammatory response in Tmprss6−/− mice.Tmprss6−/− mice, maintained at a regular diet, and control littermates, fed an ID diet, were injected with LPS and then killed 6 hours later (3 mice for each group). Hepatic expression of hepcidin (Hamp; A) and A2M (B) analyzed by TaqMan qRT-PCR. Analysis of leukocytes recruitment (CD45+; C) and infiltrating macrophages (CD11b+/F4/80+; D) in liver of Tmrpss6−/− and control mice. Liver (E) and spleen (F) IL6 mRNA expression were analyzed by TaqMan qRT-PCR. Hprt1 was used as the housekeeping gene to normalize gene expression. mRNA expression ratio was normalized to an ID mean value of 1. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
Decreased inflammatory response in Tmprss6−/− mice.Tmprss6−/− mice, maintained at a regular diet, and control littermates, fed an ID diet, were injected with LPS and then killed 6 hours later (3 mice for each group). Hepatic expression of hepcidin (Hamp; A) and A2M (B) analyzed by TaqMan qRT-PCR. Analysis of leukocytes recruitment (CD45+; C) and infiltrating macrophages (CD11b+/F4/80+; D) in liver of Tmrpss6−/− and control mice. Liver (E) and spleen (F) IL6 mRNA expression were analyzed by TaqMan qRT-PCR. Hprt1 was used as the housekeeping gene to normalize gene expression. mRNA expression ratio was normalized to an ID mean value of 1. Error bars indicate SE; ns, not significant; *P < .05; **P < .005; and ***P < .0001.
Under basal conditions Tmprss6−/− mice had similar levels of CD45+ cells (Figure 6C) and macrophages (CD45+CD11b+/F4/80+ cells) in the liver (Figure 6D) as ID wild-type littermates. Inflammatory cell recruitment, strongly increased by LPS injection in the liver of ID mice was significantly less prominent in Tmprss6−/− mice (Figure 6C-D), which had lower levels of IL6 mRNA in spleen-derived macrophages (Figure 6E) and in total liver (Figure 6F). In agreement with the more severe iron deficiency of mutant mice, TfR1 mRNA was higher in spleen-derived macrophages compared with ID control littermates (supplemental Figure3C). In support of the anti-inflammatory role of hepcidin, serum IL6 was significantly lower in LPS-treated Tmprss6−/− mice (68.56 ± 11.81 pg/mL) compared with LPS-treated ID littermates (232.66 ± 64.15 pg/mL; P < .01).
Together these results demonstrate that high hepcidin levels in Tmprss6−/− mice are protective against the LPS-mediated inflammatory effects and support the conclusion that reduced hepcidin levels and not simply iron deficiency are the cause of the proinflammatory condition observed in iron deficiency.
Discussion
Hepcidin levels in iron deficiency are reduced because the BMP pathway is down-regulated.19 When BMP signaling is inactivated by treatment with the BMP receptor inhibitor dorsomorphin,30 IL6-mediated hepcidin activation is compromised, suggesting a cross-talk between these 2 pathways of hepcidin activation. Here we explored the complex interplay between these pathways. We demonstrated that iron deficiency in mice causes a proinflammatory state, characterized by high WBC count, increased transcription of liver acute-phase proteins and liver recruitment of inflammatory cells, and made more pronounced by LPS. The observation of an inhibitory effect of iron on the proinflammatory immune response with consequent decreased of inflammatory cytokines (TNFα, IL6) reported by several studies31-35 is in line with our results. However, in theory, both iron deficiency and lack of hepcidin17 might be responsible of this effect. To discriminate between the role of iron and that of hepcidin we used 2 approaches: (1) we pretreated ID mice with a short course of exogenous hepcidin before LPS challenge; and (2) we analyzed the LPS response in Tmprss6−/− mice, which, despite severe iron deficiency, have elevated hepcidin levels. Pretreatment with hepcidin rescued the inflammatory phenotype of spleen macrophages in ID mice, which supports the proposed anti-inflammatory function of hepcidin.17 Consistent with our results, mouse models of hemochromatosis asHfe−/−,36 Bmp6−/−,6 and liver conditional Smad4 deficient mice,7 characterized by iron overload but low hepcidin, and hepcidin−/− mice,17 respond to LPS more actively that IR controls. We were, however, unable to detect a down-regulation of serum IL6 in ID mice pretreated with hepcidin. The discrepancy between the strong down-regulation of mRNA and the normal serum protein levels may be accounted for by their different kinetics, as observed,17 serum IL6 having a longer half-life compared with IL6 mRNA.27 Dissociation between transcription and serum release of IL6 in response to LPS was also reported in Hfe−/− mice.36
Hepcidin pretreatment reduces inflammatory response but, as expected, causes macrophage iron sequestration. It has been shown that iron alone does not modulate macrophage cytokine transcription.17 To further support this conclusion, we analyzed Tmprss6−/− mice, characterized by high hepcidin levels and severe tissue and spleen iron deficiency.
Although more severely ID than their littermates maintained on an iron-poor diet, Tmprss6−/− mice show a blunted response to LPS, reduced inflammatory cell recruitment in the liver, reduced acute-phase proteins and serum IL6. Together, these findings suggest that low hepcidin, not low iron levels controls inflammation in vivo.
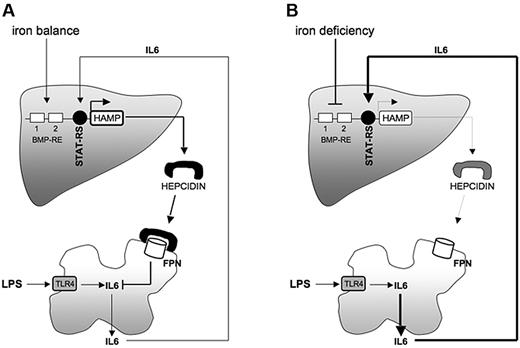
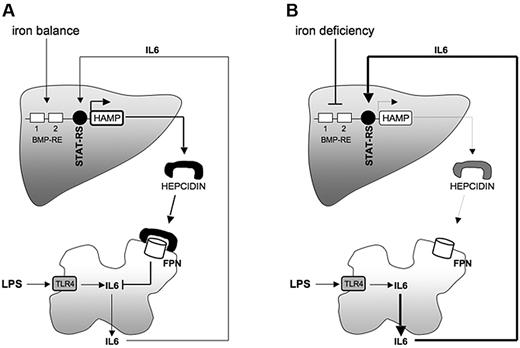
The model we propose is shown in Figure 7. Under IR conditions (Figure 7A), LPS stimulates macrophage production of inflammatory cytokines (IL6). IL6 up-regulates hepcidin transcription through STAT3 phosphorylation. Hepcidin binds to macrophage ferroportin resulting in 2 negative feedback effects: the reduction of circulating iron (not shown) and the impairment of inflammatory cytokine (IL6). In iron deficiency (Figure 7B), LPS activates IL6. However, the macrophage inflammatory response is exaggerated as a consequence of low hepcidin production. Despite high IL6, hepcidin, because of the block of the SMAD pathway, cannot be up-regulated.
Iron deficiency controls the inflammatory response through modulation of hepcidin. Schematic representation of the proposed model. In normal conditions (iron balance; A), LPS, on binding TLR4, stimulates macrophages to produce inflammatory cytokines (IL6); hepcidin is up-regulated by STAT3 and released into the blood stream to control both iron recycling (not shown) and IL6 transcription in macrophages. In iron deficiency (B), hepcidin transcription is severely reduced. LPS injection activates macrophages to produce IL6. The IL6 production is exaggerated because of the lack of the hepcidin-mediated anti-inflammatory response. BMR-RE indicates bone morphogenetic protein–responsive element; STAT-RS, STAT3–responsive site; HAMP, hepcidin; FPN, Ferroportin; and TLR4, Toll-like Receptor 4.
Iron deficiency controls the inflammatory response through modulation of hepcidin. Schematic representation of the proposed model. In normal conditions (iron balance; A), LPS, on binding TLR4, stimulates macrophages to produce inflammatory cytokines (IL6); hepcidin is up-regulated by STAT3 and released into the blood stream to control both iron recycling (not shown) and IL6 transcription in macrophages. In iron deficiency (B), hepcidin transcription is severely reduced. LPS injection activates macrophages to produce IL6. The IL6 production is exaggerated because of the lack of the hepcidin-mediated anti-inflammatory response. BMR-RE indicates bone morphogenetic protein–responsive element; STAT-RS, STAT3–responsive site; HAMP, hepcidin; FPN, Ferroportin; and TLR4, Toll-like Receptor 4.
Implications of our results are the following:
The 2 anti-inflammatory properties of hepcidin, iron sequestration, and modulation of the cytokine response, are complementary and both are based on negative feedback loops. When iron is sufficient, high hepcidin blocks cellular iron export and impairs growth of pathogens. At the same time, however, hepcidin reduces IL6 and limits potential damage because of an excessive inflammatory response. In condition of iron deficiency, increased inflammation provides only a second line of defense against invading microorganisms.
Whether this mechanism pertains to other conditions characterized by low hepcidin remains to be demonstrated. Both acute and chronic hypoxia are associated with strong hepcidin suppression.37,38 Recently, hematologic and iron parameters, serum hepcidin, and IL6 were measured in normal volunteers after acute and chronic exposure to high-altitude hypoxia.38 Hepcidin reduction after acute hypoxia exposure was paralleled by an early and stable increase of serum IL6, in the absence of any infection/inflammatory condition. Both IL6 and hepcidin reverted to normal with the return of the volunteers to the sea level.38 This finding supports our view of the effect of hepcidin on IL6.
Although our results have been obtained in an acute model of inflammation, we suggest that the anti-inflammatory properties of hepcidin should be taken into account when planning to antagonize the hepcidin effect with the aim of improving the anemia of chronic diseases.39 Manipulating the hepcidin pathway should be undertaken with great caution because it might have the negative effect of leaving the inflammatory response uncontrolled with subsequent potential damage to the organism.
Iron deficiency is extremely common worldwide, not only in underdeveloped areas because of inadequate dietary intake, but also in children and in pregnant women in socio-economically well developed countries.40 It appears that no strong selection has evolved against the inhibitory control of iron absorption. We speculate that this might be related to the strong effect of hepcidin as a modulator of inflammation that could render ID subjects more resistant to infection.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are indebted to Carlos Lopez-Otin for giving us the Tmprss6−/− mice. They warmly thank Jerry Kaplan for critical reading of the manuscript and Ivana De Domenico for the kind gift of hepcidin.
This work was partly supported by Association Francaise contre les Myopathies (AFM 14137; L.S. and P.R.-Q.); FIRB/IDEAS (P.R.-Q.); Cariplo Foundation (project 2009-2483), Regione Lombardia (SAL-11, ID17389), and Telethon Grant GGP08089 (C.C.).
Authorship
Contribution: A.P. and A.N. performed experiments; G.C. and L.B. contributed to the isolation of macrophages and performed FACS analysis; P.R.-Q. contributed to experimental design and to the writing of the manuscript; C.C. designed the research and contributed to the writing of the manuscript; and L.S. designed the research, analyzed the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Clara Camaschella, Vita-Salute San Raffaele University, Via Olgettina, 60, 20132 Milan-Italy; e-mail: camaschella.clara@hsr.it.
References
Author notes
A.P. and A.N. contributed equally to the work.