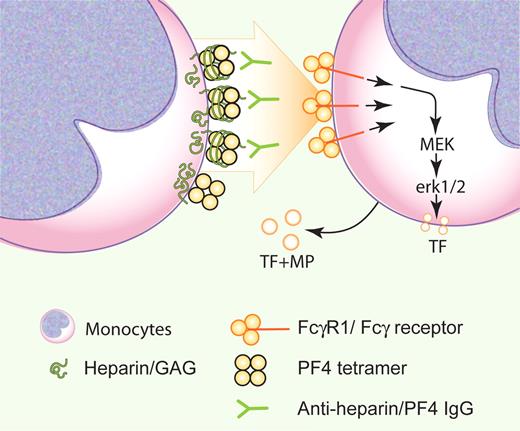
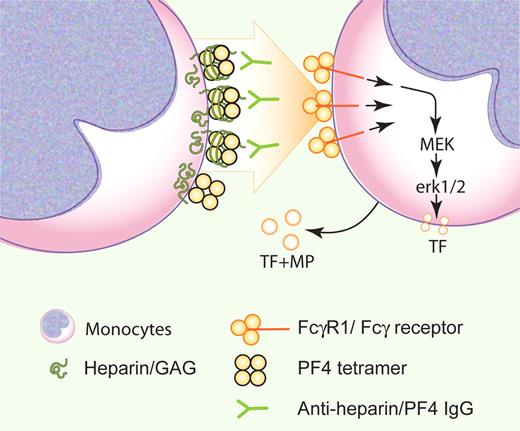
Heparin-induced thrombocytopenia (HIT) is a paradoxical disorder. Patients with HIT develop thrombocytopenia while on heparin, yet the clinical manifestations are dominated by venous, arterial, and/or microvascular thrombosis.2,3 These thrombi are platelet- and fibrin-rich. However, the initiators of thrombosis have been poorly understood because clots develop in the presence of physically intact endothelium, that is, without exposure of blood to the subendothelial matrix. Initial progress in understanding fibringeneration in HIT came from studies by Pouplard et al and Arepally et al, indicating that monocytes express tissue factor (TF) when stimulated by the HIT immune complex, consisting of macromolecular heparin/PF4 in combination with anti-heparin/PF4 IgG antibodies.4,5 Now Kasthuri et al confirm and extend these findings, discovering that monocytes express TF and release TF+ microparticles (MPs) on stimulation by HIT immune complexes.
The authors are to be commended for validating that both human HIT IgG and the HIT-like monoclonal antibody KKO act the same. As per the figure, they nicely demonstrate that the CD64 FcγRI receptor on monocytes, and not FcγRIIA (CD32a), transduces the signal to TF generation. Furthermore, they demonstrate that MEK and erk1/2 are involved. One more interesting note from these careful studies: their data are consistent with the localization of the stimulatory HIT immune complex on the neighboring cell surface, in keeping with the observations by Rauova and colleagues.6
Monocytes contribute to thrombosis in heparin-induced thrombocytopenia (HIT) by cell surface HIT immune complexes triggering the FcγRI receptor via erk1/2 to produce a TF+ surface and TF+ microparticles. Professional illustration by Paulette Dennis.
Monocytes contribute to thrombosis in heparin-induced thrombocytopenia (HIT) by cell surface HIT immune complexes triggering the FcγRI receptor via erk1/2 to produce a TF+ surface and TF+ microparticles. Professional illustration by Paulette Dennis.
The generation of TF and TF+ MPs by monocytes likely plays a substantial role in the thrombosis of HIT. We can hope that this new knowledge of the effectors in this process enables targeted approaches that minimize hemorrhagic side effects in treating HIT.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■