Abstract
Outcome of patients with Ph-positive acute lymphoblastic leukemia (Ph+ ALL) improved markedly with the introduction of tyrosine kinase inhibitors (TKIs) used in combination with chemotherapy. However, despite very high rate of complete remissions the possibility of cure with conventional-dose treatment remains questionable. Hence, allogeneic hematopoietic stem cell transplantation (HSCT) is still considered a standard of care. Patients lacking appropriate donor are usually treated with TKI-based maintenance. Autologous HSCT could be an alternative approach, however, due to “negative” results of a series of prospective studies run in XX. century its use has been limited. The goal of the current analysis was to retrospectively analyze if results of autoHSCT for Ph+ ALL changed over time.
Results of 171 autologous transplantations performed in the first complete remission between 1996–2010 and reported to the EBMT registry have been analyzed. Median patient age was 48.3 (19–65) years. Conditioning regimen was based on either TBI (63%) or chemotherapy (37%). Peripheral blood was used as a source of stem cells in 84% cases.
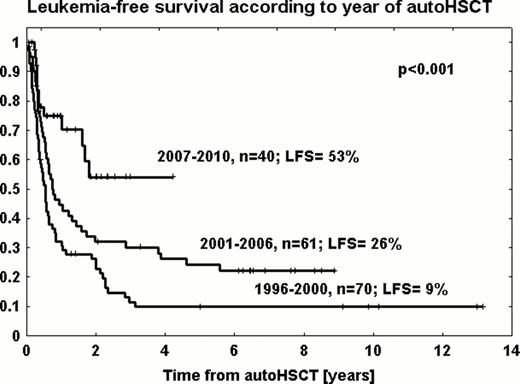
With the median follow-up of 2 years, in the whole study group, the probability of the overall survival (OS) at 2 years was 45% (+/−4%) and leukemia-free survival (LFS) was 32% (+/−4%). The cumulative incidence of relapse (RI) and non-relapse mortality (NRM) was 54% (+/−4%) and 13% (+/−3%), respectively. LFS rates were comparable for TBI and chemotherapy-based conditioning (34% vs. 29%, p=0.53). As well, the source of stem cells had no impact on LFS (32% for PB vs. 33% for BM, p=0.91). The 2 year probability of LFS increased from 22% for transplants performed between 1996–2000 (n=70) to 32% between 2001–2006 (n=61) and 54% between 2007–2010 (n=40), p<0.001 (Fig). In respective periods the RI decreased from 65% to 47% and 46% (p=0.01), while NRM was 11%, 21% and 0% (p=0.03). In a multivariate analysis the year of transplantation (<2007 vs. 2007–2010) was the only factor independently influencing the risk of treatment failure (HR=2.98, 95%CI, 1.54–5.79; p=0.001).
We conclude that results of autologous HSCT for Ph+ ALL improved markedly in recent period with more than half of patients being alive and leukemia-free at 2 years. Therefore, it appears than in the era of TKIs autologous HSCT may be considered potentially curative option. The advantage is probably associated with more profound responses achieved with TKIs, which, however requires confirmation in a separate analysis. As well, the role of post-transplant maintenance remains to be determined.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.