Abstract
Abstract 4158
Allogeneic hematopoietic stem cell transplantation (HSCT) remains the only curative procedure for patients of high-risk acute myeloid leukaemia (AML) and Myelodysplastic syndromes (MDS). The development of reduced intensity protocols (RIC) has expanded this treatment modality to older patients and to those with comorbidities. The development of the HCT-CI has been an important advance in attempting to more effectively assess patient′s fitness and likely non-relapse mortality (NRM); however its prognosis significance in a population of elderly patients remains uncertain. We evaluated the impact of HCT-CI and other factors that may enhance risk stratification in patients of advanced age receiving a RIC HSCT with alemtuzumab T-cell depletion.
85 consecutive patients aged >60 years who received a RIC HSCT for MDS and AML between January 2002 and December 2010 were retrospectively analysed, All patients received an FBC conditioning regimen (fludarabine 150mg/m2 iv, busulphan 8mg/kg oral or 6.4 mg/kg iv, alemtuzumab 100mg iv) followed by HSCT from an HLA identical sibling (n=19) or volunteer unrelated donors (n=66). Median age was 64 years (range 60–72), with 57/28 male/female. Diagnoses included AML with trilineage dysplasia (AML-TLD n=47), RAEB I/II (n=17), CMML (n=8) and RCMD (n=13),cytogenetics (high risk n= 22), IPSS risk divided patients in Low/Intermediate 1 risk (n=13), Intermediate 2 (n=11), High risk (n=6), AML (n=47). A survival analysis for NRM, overall survival (OS), disease free survival (DFS) was performed including pre-transplant HCT-CI (HCT-CI 0 n=20, HCT-CI 1–2 n=21 and HCT-CI >=3 n=43), ferritin level (<1500 mg n=43, >1500 n=42), number of courses of high dose chemotherapy (=<2 courses n=49, > 2 courses n=33), disease status pre-transplant (CR n=75, no CR n=10), CRP level (<10 n=34, >10 n=25), age >= 65 (<65 n=53, >65 n= 32), albumin median (albumin median = 42g/L), median Inmunoglobulin G (IgG, median = 9,85g/L) and median Inmunoglobulin M (IgM, median = 0,79g/L).
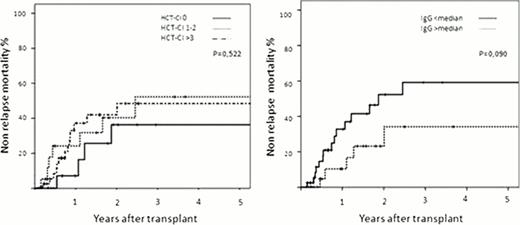
At last follow up 60/85 patient had died (NRM, n=25, relapse n=35; median follow-up, 3.5 years, range 0.3–9.5). HCT-CI score showed no statistically significant impact on 2-year NRM (27 %, 40% and 42% in patients having an HCI-CI score of 0, 1–2 and > =3 respectively, p=0.522, Figure) and 3-year NRM (27%, 52% and 49% respectively) or on 2-year OS (40 %, 39% and 29% in patients having an HCI-CI score of 0, 1–2 and > =3 respectively, p=0.577). Ferritin level, number of courses of high dose chemotherapy, CRP level, age >= 65, albumin level and IgM had not statistically significant impact on NRM or OS, while there was a trend of better outcome for patients with higher IgG level (2 and 3-year NRM 26% and 35% vs 53% and 61%, p=0,090, Figure 1). Of note -and as expected- patients in CR at the time of transplant had a better outcome (2 year OS of 38% vs 0%, p=0,008), and high risk cytogenetics was associated with poorer 2-year OS (41% vs 15% (p=0,006).
In summary HCT-CI does not best identify patients at higher risk of NRM in patients older than 60 years receiving an alemtuzumab T-cell depleted RIC allo HSCT for AML or MDS while there is a trend toward worse NRM in patients with lower IgG level; this suggests that poorer humoral immunity before transplant might reflect higher risk of NRM although the underlying mechanism remains to be further investigated.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.