Abstract
Abstract 881
T-cell acute lymphoblastic leukemia (T-ALL) represents a heterogeneous group of acute leukemias, which account for 25% of adult ALL. The GRAALL group recently reported a significant improvement in the outcome of BCR-ABL negative adult ALL using an intensified treatment protocol and a significantly better outcome in T-ALL harbouring NOTCH1 and/or FBXW7 (N/F) mutations compared to unmutated cases. Despite this, a third of N/F mutated T-ALL patients relapse and the identification of a T-ALL subgroup with very favorable outcome remains desirable.
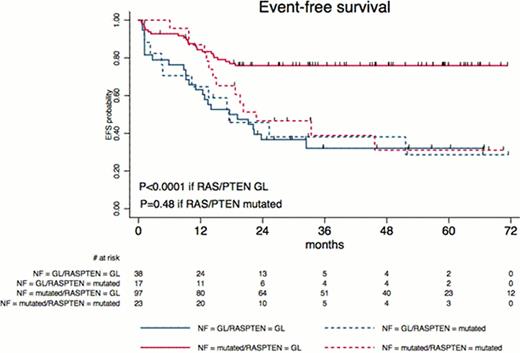
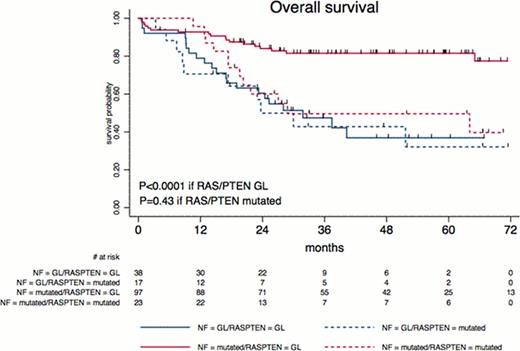
In a series of 212 adult T-ALLs included in the multicenter randomized GRAALL-2003 and 2005 trials, we searched for N/K-RAS (exon 1) mutations and PTEN (exon 7 mutations and gene deletion by CGH-array SNP-6 Affymetrix®) defects, which are considered as “type B3” mutations involved in pre-TCR signalling. Overall survival (OS) and event-free survival (EFS) were estimated by the Kaplan-Meier method, and then compared by the log-rank test.
NOTCH1 and/or FBXW7 mutations were identified in 143 (67%) of the 212 patients and lack of N/F mutation was associated with a poor prognostic. N-RAS, K-RAS and PTEN mutations were identified in 3/191 (1.6%), 17/191 (8.9%) and 17/175 (9.7%) patients, respectively. PTEN genomic deletions/mutations and N/K-RAS activating mutations were virtually mutually exclusive. N/K-RAS mutations were more frequent in TCR negative phenotype and CNS positive T-ALLs, but did not correlate with other classical parameters, EGIL phenotype, N/F status, or cortico- or chemo-sensitivity. PTEN alterations were more frequent in mature TCR expressing, SIL-TAL+, N/F unmutated cases with high leukemic bulk tumors, but did not significantly differed with respect to age, gender, CNS involvement, cortico- or chemo-sensitivity. When analyzed separately, N/K-RAS mutations or PTEN genomic abnormalities demonstrated trends to a worse outcome.
We then analyzed the effect of N/K-RAS mutations and/or PTEN genomic abnormalities on the good prognosis associated with N/F mutations by a multivariate Cox model for EFS and OS, entering the two N/F and RAS/PTEN covariates, as well as an interaction term. The prognostic significance of N/F mutations was still observed (HR, 0.26 [95% CI, 0.15–0.46] and 0.26 [95% CI, 0.14–0.49] with P<0.0001 for EFS and OS, respectively), with a significant interaction between N/F and RAS/PTEN mutations (P=0.03 and 0.05 for EFS and OS, respectively. In other terms, the favorable impact of N/F mutation was still observed in, and was restricted to patients without RAS/PTEN abnormalities. These observations led us to propose a new T-ALL oncogenetic classifier defining low-risk patients as those with N/F mutation but no RAS/PTEN mutation (97 out of 189 [51%] patients in the present cohort) and all other patients (49%, including 13% N/F and RAS/PTEN mutated cases) as high-risk patients (Figures 1A and 1B). Comparing this refined oncogenetic classifier to the simple N/F classification, hazard ratios for high-risk patients increased from 2.6 (95% CI, 1.7–4.0) to 3.25 (95% CI, 2.0–5.3) for EFS and from 2.5 (95% CI, 1.5–4.0) to 3.3 (95% CI, 1.9–5.8) for OS. When adjusting the effect of the new N/F-RAS-PTEN classifier to age (using the 35-year cutoff) and WBC (using the 100.109/L cut-off), the oncogenetic classifier remained the only significant prognostic covariate (HR= 3.2 (95% CI, 1.9–5.15) and 3.2 (95% CI, 1.9–5.6); P<0.0001 and <0.0001, for EFS and OS, respectively). The prognostic impact was maintained when GRAALL-2003 and GRAALL-2005 patients were analysed separately.
Taken together, these data demonstrate that detection of RAS and PTEN mutations add significant prognostic value to assessment of N/F status, allowing identification of nearly 50% very good prognosis T-ALL adults.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.