Key Points
A relevant xenograft chemotherapy model was developed by using standard AML induction therapy drugs and primary human AML patient samples.
Human AML cells show significantly increased sensitivity to in vivo chemotherapy treatment compared with murine LSK and total bone marrow cells.
Abstract
As acute myeloid leukemia (AML) xenograft models improve, the potential for using them to evaluate novel therapeutic strategies becomes more appealing. Currently, there is little information on using standard chemotherapy regimens in AML xenografts. Here we have characterized the immunodeficient mouse response to combined Ara-C (cytarabine) and doxorubicin treatment. We observed significant toxicity associated with doxorubicin that required optimization of the route of injection as well as the maximum-tolerated dose for immunodeficient strains. Mice treated with an optimized 5-day induction protocol showed transient weight loss, short-term reduction of peripheral blood cell and platelet counts, and slight anemia. Considerable cytotoxicity was observed in the bone marrow (BM), with primitive LSK cells having a significant survival advantage relative to more mature cells, consistent with the idea of chemotherapy targeting actively growing cells. Treated leukemic mice demonstrated reduced disease burden and increased survival, demonstrating efficacy. AML cells showed significantly increased sensitivity to doxorubicin-containing therapy compared with murine BM cells. Although early treatment could result in some cures, mice with significant leukemia grafts were not cured by using induction therapy alone. Overall, the data show that this model system is useful for the evaluation of novel chemotherapies in combination with standard induction therapy.
Introduction
Although significant progress has been made in the treatment of leukemia, relapse continues to be a significant problem, particularly in acute myeloid leukemia (AML).1 The prognosis for relapsed leukemia is poor, indicating a dire need for improvements at all stages of chemotherapy treatment. Research and development aimed at identification of novel targeted anti-leukemic compounds is of particular interest.
AML patients of all World Health Organization (WHO) subtypes other than t(15;17) received 7+3 induction therapy that combines Ara-C (cytarabine; 7 days, continuous intravenous) with an anthracycline such as daunorubicin or doxorubicin (Adriamycin; 3 days, intravenous push).2 Consolidation therapy followed in a cytogenetically directed manner, with the preferred treatment being either further intensive chemotherapy for good-prognosis cases, such as Core Binding Factor rearrangements, allogenic stem-cell transplantation for poor-prognosis cases such as those with complex cytogenetics, or a less clearly defined set of options for intermediate-prognosis cases, including normal cytogenetic AML. Maintenance therapy for AML is not current standard of care because of lack of efficacy.3-5 Patients in relapse have limited treatment options, and outcome is uniformly poor.6,7
Most patients respond to induction therapy and enter remission with undetectable levels of leukemic blasts in the bone marrow (BM). However, without further treatment, relapse is inevitable for the vast majority of patients. Additional therapeutics, in particular those that target known oncogenic signals in individual AML (personalized therapy), could potentially delay or prevent relapse.8,9 New treatment regimens are needed for relapse cases, especially in cases in which the leukemia has developed resistance to chemotherapy. In addition, even in those patients with relapsed leukemia who remain sensitive to standard chemotherapy, treatment may be complicated by toxicities associated with exceeding safe cumulative doses of individual compounds, especially anthracyclines.10 This further highlights the need for novel agents.
Many compounds that show significant anticancer effects in vitro and in preclinical models fail to show efficacy in clinical trials.11 Frequently, these compounds have been injected into mice soon after receiving fatal doses of AML cell lines. In addition, many of these experiments compare the activity of a candidate compound against carrier alone. Occasionally, a second study arm compares the effect of a single proven chemotherapeutic agent, typically cytarabine, alone and in combination with the candidate compound.12
An alternative in vivo preclinical test might compare the candidate regimen or compound(s) to standard-of-care therapies. Indeed, large-scale, multicenter clinical trials generally compare test regimens to the accepted 7+3 standard. To date, a standardized treatment regimen using combined cytarabine and anthracycline administration has not been optimized for AML xenografts. Such a model would allow more in-depth preclinical evaluation of novel candidate compounds.
Our laboratory has developed a unique model of human AML based upon retroviral expression of an MLL-AF9 (MA9) complementary DNA in human umbilical cord blood CD34+ cells.13 The transduced cells form highly clonogenic, cytokine-dependent immortal cell lines that indefinitely retain the ability to engraft immunodeficient mouse strains and induce lethal AML. We have also shown that strains of nonobese diabetic/severe combined immunodeficiency (NOD/SCID or NS) and NOD/SCID interleukin 2 receptor gamma (NOD/SCID IL2RG−/− or NSG) mice that express the human cytokines somatic cell-derived growth factor, granulocyte macrophage colony-stimulating factor, and interleukin-3 promote a faster, more predictable lethal AML that develops within a tight window.14,15 Additionally, subsequent introduction of activated NRasG12D complementary DNA into MA9 AML cells leads to cytokine-independent growth in vitro and a significantly decreased latency in vivo. Importantly, these MA9-NRas cells induce fatal AML in a very reliable manner, even in nonconditioned hosts.15 With the benefits of these unique tools in hand, we sought to develop a model system to evaluate the efficacy of chemotherapeutic agents on human AML cells in vivo.
Materials and methods
NS (NOD/SCID, Jackson Laboratories), NSG (NOD/SCID IL2RG−/−, Jackson Laboratories), NS-SGM3,14 and NSGS15 mice were bred and maintained at Cincinnati Children’s Hospital under standard conditions. Mice were placed on doxycycline chow (TestDiet; Modified Prolab RMH-1500 with 0.0625% doxycycline) prior to, during, and for several weeks after chemotherapy treatment or irradiation. All mouse experiments were conducted under the guidance of an approved protocol.
Cytarabine (Bedford Laboratories) and doxorubicin (Bedford Laboratories) were reconstituted with phosphate-buffered saline (PBS), filtered, and stored in aliquots at −20°C. Drugs were delivered by tail vein and intraperitoneal injection. Weights were taken daily during treatment, and doses were recalculated to ensure that the mice received a consistent dose of 50 mg/kg cytarabine and 1.5 mg/kg doxorubicin every treatment.
Complete blood count (CBC) analysis was obtained from tail bleed samples by using a HemaVet 9500 (Drew Scientific). Total white blood cell (WBC) counts were used to calculate total cell numbers present in BM samples, and these values were confirmed by trypan blue exclusion performed on a subset of samples.
For cell line experiments, roughly 0.25 million cultured cells were resuspended in 300 μL PBS for tail vein injection into nonirradiated mice. Patient samples were acquired following informed consent in accordance with the Declaration of Helsinki and under the direction of protocols approved by the institutional review board. Grafts were monitored by tail bleeds, and BM aspirations were monitored by using standard procedures.
Flow cytometry to detect human AML cells or to measure lin−sca+kit+ (LSK) mouse cells was performed on FACSCanto Instruments (BD) with commercially available antibodies (BD). For LSK analysis, antibodies used were Sca-1 PE, Kit APC, and Lin FITC. The Lin cocktail included antibodies against Mac-1, Gr-1, CD3, CD4, CD8a, B220, and TER119. For the cell cycle experiment, 100 μL of a 10-mg/mL bromodeoxyuridine (BrDu) solution (BD) was injected intraperitoneally on day 8 following treatment initiation and 1 hour before the BM was harvested.
Results
Lowered doses of chemotherapy must be used with NOD/SCID-derived mice
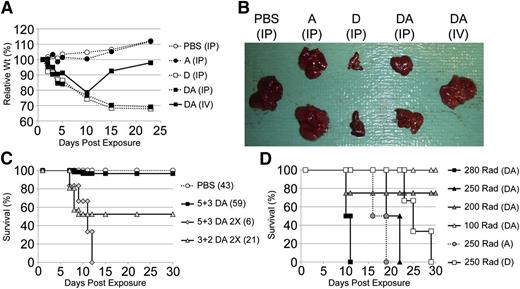
As a first step toward developing a xenograft chemotherapy model, we determined the maximum-tolerated dose (MTD) of combined cytarabine and doxorubicin for use with immunodeficient mice. A previous report used a schedule consisting of 5 consecutive daily intraperitoneal doses of 100 mg/kg cytarabine along with 3 mg/kg doxorubicin for experiments involving sublethally irradiated immune-competent C57Bl/6 mice.12 We tested these doses and several combinations that maintained the cytarabine:doxorubicin ratio. With 4-week survival as an end point for these initial studies, we found an MTD of 50 mg/kg cytarabine and 1.5 mg/kg doxorubicin. This dose was consistent for all immunodeficient strains tested, namely NS, NOD/SCID-SGM3 (NSS), NSG, and NOD/SCID-IL2RG-SGM3 (NSGS). Mice receiving this dose by intraperitoneal delivery were noticeably ill and lost significant body weight (Figure 1A). Although most of these mice survived the initial study period, this cohort remained sickly and showed increased mortality when observed for longer time periods. Necropsy revealed severe liver damage, frequently with an accumulation of peritoneal fluid as well as gross intestinal abnormalities (Figure 1B) (data not shown). These complications were specifically associated with intraperitoneal delivery of doxorubicin because we did not observe them in mice treated with PBS or cytarabine alone or when doxorubicin was administered intravenously (Figure 1A-B). Additionally, combination chemotherapy apparently lessened the effect, as evidenced by the slightly less necrotic livers observed in mice treated with doxorubicin-cytarabine (DA). Therefore, to avoid toxicity, we used intravenous codelivery (in the same syringe) of both cytarabine and doxorubicin on days 1 to 3 followed by intraperitoneal injection of cytarabine alone on days 4 and 5. Although mice on this schedule also showed signs of illness, drug-related morbidity was nearly eliminated, and necropsy revealed grossly normal liver, kidney, and intestines (Figure 1B-C) (data not shown). Furthermore, both the weight loss and observed illness were temporary, and mice appeared to make full recoveries within 2 to 3 weeks of exposure (Figure 1A). By using this improved delivery method, we attempted to increase the chemotherapy dose. However, this resulted in excessive fatalities, indicating that we had identified the MTD (Figure 1C). This 5+3 DA dosing protocol was chosen for further studies.
Optimization of chemotherapy delivery for immunodeficient mice. (A) Weights of representative mice exposed to chemotherapy (A, cytarabine; D, doxorubicin; DA, combined cytarabine and doxorubicin; IP, intraperitoneal delivery; IV, intravenous delivery). Cytarabine was given on days 1 to 5 and doxorubicin on days 1 to 3 only. (B) Whole livers were isolated from mice 28 days after initiation of drug injections. (C) Survival of mice was monitored for 30 days after exposure to different doses of cytarabine and doxorubicin. DA indicates 1.5 mg/kg doxorubicin and 50 mg/kg cytarabine. DA 2× is 3.0 mg/kg doxorubicin and 100 mg/kg cytarabine. The first number of 5+3 or 3+2 is the number of daily doses of cytarabine, and the second indicates the same for doxorubicin. A consistent volume was injected at each dose (10 microliters per gram of body weight) by preparing appropriate stock solutions. (D) Survival of mice receiving the optimized maximum-tolerated doses of D+A chemotherapy following the indicated sublethal doses of whole-body irradiation.
Optimization of chemotherapy delivery for immunodeficient mice. (A) Weights of representative mice exposed to chemotherapy (A, cytarabine; D, doxorubicin; DA, combined cytarabine and doxorubicin; IP, intraperitoneal delivery; IV, intravenous delivery). Cytarabine was given on days 1 to 5 and doxorubicin on days 1 to 3 only. (B) Whole livers were isolated from mice 28 days after initiation of drug injections. (C) Survival of mice was monitored for 30 days after exposure to different doses of cytarabine and doxorubicin. DA indicates 1.5 mg/kg doxorubicin and 50 mg/kg cytarabine. DA 2× is 3.0 mg/kg doxorubicin and 100 mg/kg cytarabine. The first number of 5+3 or 3+2 is the number of daily doses of cytarabine, and the second indicates the same for doxorubicin. A consistent volume was injected at each dose (10 microliters per gram of body weight) by preparing appropriate stock solutions. (D) Survival of mice receiving the optimized maximum-tolerated doses of D+A chemotherapy following the indicated sublethal doses of whole-body irradiation.
We next set out to test this protocol by using mice previously exposed to sublethal irradiation, the conditioning protocol used for engraftment of most leukemia cells in NOD/SCID models. We observed nearly complete mortality upon administration of the optimized 5+3 DA treatment to previously irradiated mice (Figure 1D). This result was observed even when the mice were allowed 10 weeks or more of recovery and when each compound was administered individually (data not shown). Chemotherapy was tolerated when suboptimal doses of irradiation were used; however, these radiation doses were also associated with suboptimal or no engraftment of human cells (Figure 1D) (data not shown).
Murine hematopoiesis is profoundly affected by chemotherapy
With MTD determined, we next aimed to evaluate the effects of single-agent and combination chemotherapy on endogenous murine hematopoiesis. Chemotherapy exposure induced multiple signs of illness, including lethargy, hunched posture, rough coat, and weight loss. Measurable weight loss occurred immediately after treatment initiation and correlated with dosage. A nadir was reached between days 8 and 10, with a gradual recovery to near starting levels within 2 to 3 weeks (Figure 2A). This effect was associated with doxorubicin exposure, since we did not observe a significant weight loss upon exposure to cytarabine alone. Additionally, serial CBC analysis was performed on a cohort of control and chemotherapy-injected mice (Figure 2B-G). DA-treated mice exhibited a rapid transient decline in WBC and neutrophil counts, with delayed decreases in red blood cell (RBC) and platelet numbers, all of which quickly rebounded to control levels or higher. Cytarabine alone induced a drop in WBC counts by day 8 (after initiation of exposure), although doxorubicin treatment actually increased these counts. Interestingly, the DA combination lowered WBC count further, implying a cooperative cytoreductive effect. Since doxorubicin was administered during the first 3 days of treatment, it was possible that the higher WBC counts in doxorubicin-only mice on day 8 were due to the fact that this group had been chemotherapy free for an additional 2 days compared with the cytarabine groups. Each drug independently reduced platelet counts, with counts reduced to an even greater extent when drugs were combined. RBC, hemoglobin, and hematocrit measures indicated a transient anemia that rapidly appeared following cytarabine exposure and was reproducibly delayed and muted by combination with doxorubicin. It is worth noting that, overall, these changes generally mimic changes observed in patients undergoing standard induction chemotherapy.
Chemotherapy induces a physiologically relevant response. (A) Weights of mice were monitored for 4 weeks after initial exposure to single-agent or combined chemotherapy. Weights were normalized to the weight of each mouse on day 1 of the experiment. (B-G) CBC analysis was performed before the initial exposure to chemotherapy and serially each week for 4 weeks. (B) White blood cell (WBC) count, (C) neutrophil (NE) count, (D) red blood cell (RBC) count, (E) hemoglobin (Hb), (F) hematocrit (HCT), and (G) platelet counts were monitored. (H) Total BM cellularity of an individual femur was calculated on day 8 following initial exposure to chemotherapy. The average cell number for the PBS cohort of each experiment was normalized to 1.0. LSK flow was performed on these samples to determine (I) lin− BM cell percentage, (J) LSK frequency in the BM, and (K) total LSK per femur for the control and DA groups. (L) Cell cycle analysis of PBS- and DA-exposed BM cells gated on LSK (top row) or total BM cells (bottom row). *P < .05 as determined by the Student t test. NS, not significant.
Chemotherapy induces a physiologically relevant response. (A) Weights of mice were monitored for 4 weeks after initial exposure to single-agent or combined chemotherapy. Weights were normalized to the weight of each mouse on day 1 of the experiment. (B-G) CBC analysis was performed before the initial exposure to chemotherapy and serially each week for 4 weeks. (B) White blood cell (WBC) count, (C) neutrophil (NE) count, (D) red blood cell (RBC) count, (E) hemoglobin (Hb), (F) hematocrit (HCT), and (G) platelet counts were monitored. (H) Total BM cellularity of an individual femur was calculated on day 8 following initial exposure to chemotherapy. The average cell number for the PBS cohort of each experiment was normalized to 1.0. LSK flow was performed on these samples to determine (I) lin− BM cell percentage, (J) LSK frequency in the BM, and (K) total LSK per femur for the control and DA groups. (L) Cell cycle analysis of PBS- and DA-exposed BM cells gated on LSK (top row) or total BM cells (bottom row). *P < .05 as determined by the Student t test. NS, not significant.
We next assessed the effects of chemotherapy exposure on immunodeficient mouse BM cellularity and composition. These assays were performed on several NOD/SCID-based substrains with no significant differences between the strains (data not shown). Cellularity was significantly reduced in femurs from exposed mice at day 8, demonstrating efficient targeting and general cytotoxicity in the BM, particularly upon exposure to combined DA (Figure 2H). BM counts of previously irradiated mice at day 5 were found to be 35% lower than those of nonirradiated mice at day 5, indicating that the lethality observed in conditioned mice may be at least partially related to excessive BM damage (data not shown). Consistent with the CBC data above, doxorubicin appeared to induce relatively minor effects at day 8. We euthanized additional doxorubicin-only exposed mice on day 6 to account for the earlier cessation of chemotherapy in this group. BM cellularity was significantly decreased at day 6, but this drop was still less than that observed in the cytarabine-only group.
To determine the effects of chemotherapy on the different BM cell types, we used flow cytometry to analyze the isolated BM from DA mice. As might be expected, DA mice showed a significant increase in percentage of lineage-negative cells relative to mice treated with PBS, indicating a greater toxicity to mature cell types (Figure 2I). Furthermore, the frequency of (LSK) progenitor cells was increased, although the total LSK numbers were only slightly decreased in dosed mice (Figure 2J-K), consistent with a lesser effect of chemotherapy on quiescent cell types. Fatal doses of chemotherapy induced even greater cytotoxicity in the BM without affording protection to the LSK population (data not shown). It appears that the more primitive noncycling cells were largely protected from nonfatal doses of chemotherapy, although we cannot rule out a rapid expansion of this compartment during the 5 intervening days between dosing cessation and harvest of the femurs. However, we did analyze BrDu incorporation in some mice on day 8 and found increased cycling in the BM of DA mice that was not observed in the immature Lin- or LSK populations (Figure 2L). This would imply either that expansion of the LSK population was limited to a window before day 8 or that LSK mice were undergoing asymmetric self-renewal divisions in response to chemotherapy and that lineage-positive progenitors were repopulating the BM. Overall, these results correlate well with trends observed in patients treated with these drugs, indicating that immunodeficient mice can tolerate this dosing schema and that it is producing physiologically relevant results.
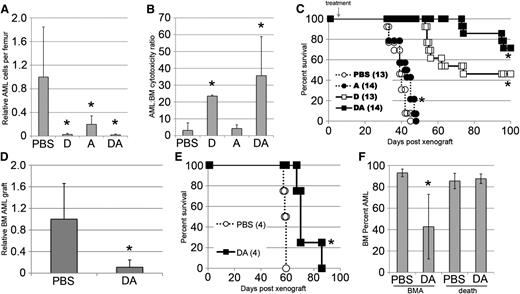
Chemotherapy shows efficacy in a human xenograft model
It has been proposed that AML is a stem-cell disease, with individual leukemia cases containing a variable population of leukemic-initiating cells (LICs).16,17 The ability to target these rare cells is critical to improving treatment of AML.18 We have previously shown that MA9 cultures have a high frequency of LICs.19 MA9 cells expressing activated N-Ras retain this high LIC frequency, are easily detectable in homing assays, and can readily engraft nonirradiated mice,15 making them ideal for testing the efficacy of the DA chemotherapy protocol. We began with an early treatment approach, treating mice 4 to 5 days after transplantation of leukemia cells followed by measurement of total AML cells per femur on day 8. With such an approach, we hoped to more specifically measure effects on LICs because they are likely overrepresented in the subset of cells with the ability to engraft mice. Mice treated with PBS harbored easily detectable AML cells at day 8 in the range of 2000 to 4000 cells per femur (Figure 3A). We observed a clear reduction of AML cells in the doxorubicin-, cytarabine-, and DA-treated cohorts. In fact, these cells were nearly undetectable in many doxorubicin and DA mice. These data were combined with the data on total BM cellularity to arrive at a ratio for AML-specific cytotoxicity (Figure 3B). Although cytarabine demonstrated a reduction in AML cells, this reduction was similar to the overall cytotoxic effect on murine BM cells, indicating only a minor degree of selectivity of cytarabine for AML cells. In contrast, doxorubicin was 20-fold more selective against early-engrafted AML cells than it was against whole murine BM (Figure 3B). The combination of both drugs further improved the selectivity against MA9-NRas AML to approximately 35-fold. Importantly, these measures of efficacy correlated with the survival of mice that were identically treated and monitored for development of AML (Figure 3C). Although all groups produced significant latency shifts, the cytarabine effect was quite minor. Doxorubicin treatment alone greatly improved survival with nearly half the mice surviving leukemia free for the 100-day experimental period. Combined DA treatment further improved on both latency and survival, again demonstrating synergy. AML was undetectable in BM samples taken from surviving mice at the end of these experiments.
Chemotherapy shows efficacy against human AML in vivo. (A) Human MA9-NRas AML cells remaining in the femurs of mice treated with chemotherapy were quantified on day 8 by cell counts and flow cytometry. The average AML cell number for the PBS group (1000 to 4000 cells per femur) was set to 1.0 in each experiment. (B) By using these data and data from Figure 2H, a ratio of AML to normal BM toxicity was calculated. (C) Mice engrafted and treated as in (A) were followed for survival. (D) Mice were injected with an AML patient sample (AMLCC2) and treated with chemotherapy. BM grafts were determined 6 to 8 weeks later. The average PBS grafts (15% to 40% AML) were set to 1.0 for each experiment for normalization. (E) Mice engrafted with a second AML patient sample (AMLCC1) were followed for survival. (F) BM grafts of AMLCC1-engrafted mice were determined at day 45 and again at time of death for each mouse. *(A, B, D, F) indicates P < .05 by the Student t test. *(C, E) indicates P < .05 by the log-rank test.
Chemotherapy shows efficacy against human AML in vivo. (A) Human MA9-NRas AML cells remaining in the femurs of mice treated with chemotherapy were quantified on day 8 by cell counts and flow cytometry. The average AML cell number for the PBS group (1000 to 4000 cells per femur) was set to 1.0 in each experiment. (B) By using these data and data from Figure 2H, a ratio of AML to normal BM toxicity was calculated. (C) Mice engrafted and treated as in (A) were followed for survival. (D) Mice were injected with an AML patient sample (AMLCC2) and treated with chemotherapy. BM grafts were determined 6 to 8 weeks later. The average PBS grafts (15% to 40% AML) were set to 1.0 for each experiment for normalization. (E) Mice engrafted with a second AML patient sample (AMLCC1) were followed for survival. (F) BM grafts of AMLCC1-engrafted mice were determined at day 45 and again at time of death for each mouse. *(A, B, D, F) indicates P < .05 by the Student t test. *(C, E) indicates P < .05 by the log-rank test.
We sought to repeat this finding with 2 separate AML patient samples that we determined were able to engraft mice without irradiation preconditioning. BM aspirates taken at intermediate time points showed significant reduction of AML graft in DA-treated mice, and mouse survival was increased by chemotherapy treatment (Figure 3D-F). At death, BM grafts of treated mice were similar in percentage to those of nontreated mice (Figure 3F). Together, these data suggest that the leukemia was merely delayed, and normal growth resumed after therapy was stopped. Although responsive to DA treatment, these 2 patient samples were notably more resistant to therapy than were the MA9-NRas cells under identical conditions, consistent with the heterogeneous nature of AML response to induction therapy.
In an effort to more realistically model AML response to therapy, we allowed mice to develop measurable grafts before the initiation of treatment. Treatment began at day 25 posttransplantation, just before AML fatalities are typically observed in this model, ensuring that a majority of the mice would have an easily detectable tumor burden. We observed increased latency with doxorubicin and DA treatment, although cytarabine treatment showed no significant effect on survival (Figure 4A). We performed this experiment with another MA9 clone carrying an activated Flt3-ITD mutation (instead of activated NRas) and found a similar delay in latency upon DA treatment (Figure 4B). Tumor burden was determined before treatment in this experiment and correlated well with the survival of individual mice (Figure 4C-D). Although the data indicate that treatment prolongs life when comparing mice of roughly equivalent grafts, the difference is most significant in mice with low tumor burden but is fairly minor in mice with high AML levels. DA therapy did not result in any cures, implying that treatment was significantly more difficult once the leukemia was allowed to progress.
Differential effects of chemotherapy against overt leukemia are observed in vivo. (A) Survival of mice treated with chemotherapy 25 days after engraftment with MA9-NRas AML cells. (B) Survival of mice treated with chemotherapy 35 days after engraftment with MA9-ITD AML cells. (C) The BM grafts of mice in (B) were determined before therapy and show that treatment delays death in mice with roughly equivalent grafts. (D) Individual data points from (C) plotted to show correlation of survival with measured AML graft in mice treated with PBS and DA. (E) Flow cytometry plots demonstrating a reduction of AML burden in a mouse with a significant human AML patient sample graft following combined DA chemotherapy. (F) Summary of additional experiments performed with other AML patient samples and cell lines showing variable response in vivo. *P < .05 by the log-rank test. ARAC, Ara-C (cytarabine); DOXO, doxorubicin.
Differential effects of chemotherapy against overt leukemia are observed in vivo. (A) Survival of mice treated with chemotherapy 25 days after engraftment with MA9-NRas AML cells. (B) Survival of mice treated with chemotherapy 35 days after engraftment with MA9-ITD AML cells. (C) The BM grafts of mice in (B) were determined before therapy and show that treatment delays death in mice with roughly equivalent grafts. (D) Individual data points from (C) plotted to show correlation of survival with measured AML graft in mice treated with PBS and DA. (E) Flow cytometry plots demonstrating a reduction of AML burden in a mouse with a significant human AML patient sample graft following combined DA chemotherapy. (F) Summary of additional experiments performed with other AML patient samples and cell lines showing variable response in vivo. *P < .05 by the log-rank test. ARAC, Ara-C (cytarabine); DOXO, doxorubicin.
Additional experiments were performed by using mice with measurable AML patient sample grafts. BM engraftment was measured just prior to initiation of chemotherapy and again on day 8. One of five samples responded well to chemotherapy, as evidenced by a significant reduction of AML detected by flow cytometry (Figure 4E). Notably, this sample contained a CD34+CD38− population that, although it was diminished, it was not entirely eliminated by DA treatment, but it also did not appear to be differentially resistant relative to the other phenotypic populations. Other samples were refractory to treatment or showed only minor responses (Figure 4F). For example, although mice engrafted with AML1 contained either higher, lower, or equal frequencies of total human cells before and after treatment, the CD34+ component was consistently higher in these mice, indicating that this sample may contain primitive cells that are resistant to standard chemotherapy. A summary of all tested samples is shown in Figure 4F. Although most of the patient samples we analyzed appeared to be resistant to chemotherapy, one of our known pretreatment samples, AML5, was fairly responsive, with significant reductions in AML burden similar to that observed with several MLL-AF9 cell lines.
Discussion
We have optimized a chemotherapy protocol for induction therapy in the most commonly used immunodeficient mouse strain, NSG. Our data highlight the importance of the route of delivery, especially regarding the anthracycline doxorubicin, in contrast to the published data in immunocompetent mouse models.12 This unique problem for NOD/SCID-based immunodeficient mice likely centers around the SCID (PRKDC) mutation, which affects a key DNA damage repair pathway.20 These strains are well known to be significantly more radiosensitive than typical laboratory mice, including other immunodeficient strains, such as the NOD/RAG/IL2RG (NRG) mouse, which relies on a defective recombination-activated gene (RAG) for impaired lymphocyte differentiation.21,22 Although the RAG mutation is hematopoietic-specific, the SCID mutation affects most tissues of the body. This may partially explain the sensitivity of NSG mice to intraperitoneal injection of doxorubicin and to combined irradiation-chemotherapy protocols (Figure 1). Nevertheless, since doxorubicin is known to cause severe tissue necrosis clinically, we might expect to observe some organ toxicity, even in immunocompetent mice injected via the intraperitoneal route. This may also have contributed to the toxicity issues encountered by using daunorubicin in the immunocompetent mouse model of AML.12
Our data showing that preconditioning of mice with radiation precludes the subsequent use of chemotherapy implies that only the most aggressive samples can be used for AML xenograft chemotherapy studies. Although these aggressive samples are known to be the most likely to relapse,23 it is still critical that we devise approaches to expand these chemotherapy models to AML samples needing preconditioning of mice for efficient engraftment, since they represent the majority of samples. It will be important to determine whether NRG mice respond more favorably to chemotherapy and to allow for expanded treatment schedules. In addition, these approaches will reflect the clinical situation more accurately if we are able to build in a second round of chemotherapy to mimic consolidation. We have been unable to use this approach in NOD/SCID-based mice (data not shown). However, recent success using consolidation therapy with a liposomal formulation of cytarabine and daunorubicin in RAG2 immunodeficient mice indicates that this approach is feasible, either by modifying the host or the formulation of the chemotherapy.24
Ideally, an in vivo xenograft chemotherapy model will show physiologically relevant responses to the drugs that parallel what is seen in the clinic. We felt this was an important point to evaluate, especially considering the aspects of chemotherapy treatment that we cannot readily mimic in the mouse. For example, although the dose of doxorubicin closely estimates equivalent human doses based on weight, the cytarabine dose is approximately 20-fold higher than what is administered to patients receiving standard 7+3 induction therapy (60 mg/m2 daunorubicin and 100 mg/m2 cytarabine). Converted to milligrams per kilogram, these values roughly equate to 1.5 mg/kg daunorubicin and 2.5 mg/kg cytarabine. This increase in cytarabine is necessary to reach adequate plasma levels with a bolus injection compared with the continuous intravenous infusion used in clinical care. Importantly, we observed many changes in the peripheral blood (PB) counts and BM composition that fit with the clinical experience quite well (Figure 2). The rapid weight loss, neutropenia, and low WBC counts, followed by a delayed RBC and platelet effect, are reminiscent of the effects seen during induction chemotherapy in humans. We also observed profound changes in BM cellularity, with specific effects on mature cells relative to the more primitive quiescent cells, indicating that this treatment regimen is effectively targeting BM. This is important since the BM is the prime reservoir for AML cells. Of interest was the differential sensitivity of the AML cells to doxorubicin treatment relative to the effects on the mouse BM cells (Figure 3B). This was not evident for cytarabine, which had a profound cytotoxic effect on the mouse BM cells (to a greater degree than doxorubicin treatment) but did not affect the AML cells to the same extent as doxorubicin. To the best of our knowledge, this has not been previously reported. These types of questions can now be pursued at a more mechanistic level in vivo to determine whether these effects are intrinsic to the AML cells in this study or whether they apply more broadly to transformed cells in general. Although the MA9-NRas cells we used here have a higher clonogenicity than most AML samples, it will be possible to replicate these findings by using primary patient samples to quickly assess the ability of particular chemotherapy drugs to target these critical cells. Our preliminary data indicate that some patient AML samples do respond to chemotherapy in this xenograft model (Figures 3D-E and 4E). Importantly, these results correlated with survival in follow-up experiments that used both MA9-NRas and patient AML samples, possibly signifying a reduction in total numbers of LICs in response to chemotherapy (Figure 3C,E).
Our initial studies with AML xenografts used treatment at a very early time point, only 4 to 5 days after engraftment (Figure 3). This approach offers an opportunity to assay for the effects of chemotherapy on only those few cells that successfully engraft, a key property that may reflect the LICs. There is some evidence in the literature that LICs may have a differential response to chemotherapy compared with bulk leukemia cells.25 Although the CD34+CD38− phenotype is not a definitive marker of AML stemness,26-28 recent evidence indicates that the majority of patient AML samples are enriched for LIC activity in the CD34+CD38− compartment.28-30 From our limited experience in this study, we did not observe a survival advantage for the CD34+CD38− cells in the responsive patient AML sample we used (Figure 4E). More work is needed to determine whether a cell surface marker or cellular functional measure (eg, side population, aldehyde dehydrogenase [ALDH] expression) correlates with chemoresistance in vivo.
Although modeling chemotherapy in freshly engrafted mice is convenient and can answer many biological questions, it is not an ideal model for mimicking induction treatment of overt AML. With this in mind, we allowed mice to become fully engrafted before initiating treatment to assess the efficacy of our chemotherapy protocol on a mouse with high tumor burden. Induction chemotherapy in leukemic mice was notably less effective at extending the survival of mice engrafted with MA9 leukemia cells, leaving significant room for improvement by using additional therapies and/or consolidation therapy (Figure 4A-B). By flow cytometry, we were able to easily detect and quantify residual disease in mice engrafted with patient samples. This aspect makes the xenograft model ideal for evaluating therapies that might specifically target the few remaining primitive AML cells. Some patient samples were found to be refractory to treatment, recapitulating a key clinical problem. Other samples responded to treatment, but the few remaining AML cells did not phenotypically resemble the LICs as defined in other xenograft AML models.25 Intriguingly, the best responding patient sample (Figure 4E) was a sample taken before any therapy. We tested a number of relapse samples in this same assay (Figure 4F), none of which responded to chemotherapy. It will be interesting to determine whether this trend holds up in larger cohorts of samples and whether we can correlate therapeutic response in our model to clinical outcome of the patients. These samples will be especially good tools that can be used in screens of candidate therapies that could be useful in combating refractory or relapse AML.
In summary, we have developed a model system to evaluate the efficacy of chemotherapeutic agents on human AML cells in vivo. This model permits a detailed analysis of tumor response to the standard best-of-care treatment regimen in use in the clinic and should allow a careful examination of the critical few cancer stem cells that remain after induction therapy with the goal of identifying novel compounds capable of targeting these cells.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the Comprehensive Mouse and Cancer Core of the Children’s Hospital Research Foundation for help with cell and chemotherapy injections, the Cincinnati Children’s Hospital Medical Center Research Flow Cytometry Core for flow cytometry help, Janet Schibler for technical support, and Dr Ashish Kumar (Cincinnati Children’s Hospital), Dr Martin Carroll (University of Pennsylvania), and Guido Marcucci (Ohio State University) for patient AML samples.
This work was supported by Department of Defense grant PR081404 (Y.S. and J.C.M.), an Institutional Clinical and Translational Science Award, National Institutes of Health/National Center for Research Resources grant 1UL1RR026314-01, and a Center of Excellence in Molecular Hematology P30 award (DK090971). J.C.M. is a Leukemia and Lymphoma Scholar.
Authorship
Contribution: M.W. designed and performed experiments, analyzed and interpreted data, and wrote the paper. B.M. designed experiments and interpreted data. F.-S.C., C.S., and M.S. performed experiments. Y.S. contributed essential reagents. J.C.M. designed experiments, interpreted data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: James C. Mulloy, Division of Experimental Hematology and Cancer Biology, Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, 3333 Burnet Ave, MLC 7013, Cincinnati, OH; e-mail: james.mulloy@cchmc.org.