To the editor:
An earlier report by Bucher et al1 indicated a better stem cell transplant (SCT) outcome with younger sibling donors (YSD). Transmaternal cell flow during pregnancy2 might explain this observation. Notably, cord blood comprises minor H antigen experienced T cells that are not only directed against maternal foreign minor H antigens.3,4 This observation prompted us to investigate the role of minor H antigens in the birth order effect in HLA identical SCT.
Hereto, we made use of a large database of 10/10 HLA allele-matched and minor H antigen–typed SCT donor/recipient pairs (Spierings et al, submitted), collected under the auspices of the International Histocompatibility and Immunogenetics Workshop and Conference. Additional relevant family information was included for 311 10/10 HLA allele–matched sibling donor/recipient pairs.
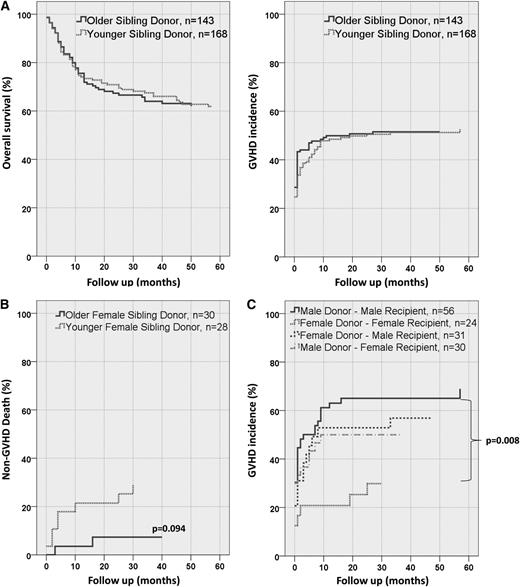
In the whole cohort of 311 pairs, overall survival, graft versus host disease (GVHD) incidence, GVHD-related mortality, and GVHD-free survival were not statistically significantly different in SCT with older sibling donors (OSD, n = 143) compared with SCT with YSD (n = 168; Figure 1A).
Influence of birth order on overall survival and GVHD incidence. (A) Overall survival and GVHD incidence in recipients with a YSD (n = 168) compared with recipients with an OSD (n = 143) are not statistically significantly different. (B) Female donors with female recipients have a higher non-GVHD death incidence (ie, relapse) in YSD compared with OSD (hazard ratio = 3.76, P = .094). (C) Adult YSD are subdivided by gender. Female donors in female recipients have a significantly (P = .008) reduced GVHD incidence compared with M→M.
Influence of birth order on overall survival and GVHD incidence. (A) Overall survival and GVHD incidence in recipients with a YSD (n = 168) compared with recipients with an OSD (n = 143) are not statistically significantly different. (B) Female donors with female recipients have a higher non-GVHD death incidence (ie, relapse) in YSD compared with OSD (hazard ratio = 3.76, P = .094). (C) Adult YSD are subdivided by gender. Female donors in female recipients have a significantly (P = .008) reduced GVHD incidence compared with M→M.
The sample size of 311 appeared too small to analyze the effect of either single or multiple autosomally or of single Y chromosome–encoded minor H antigen(s). However, the effect of gender mismatch5 on the birth order effect appeared feasible to investigate. Interaction analyses of birth order and gender mismatch showed a statistically significant interaction for non-GVHD, which is merely relapse-related, death (P < .05; data not shown). Subsequent analysis in female recipients of female donors (F→F; Figure 1B) showed lower, nonsignificant non–GVHD-related death in the YSD group (hazard ratio = 3.76, P = .094).
The study cohort comprised pediatric and adult SCT pairs. The number of pediatric pairs (n = 40) was too small to analyze separately. Analysis of the adult SCT pairs revealed a significant reduced GVHD incidence in the YSD group as opposed to the OSD group by comparing F→F transplantation with male donors to male recipients (M→M) transplantation (hazard ratio = 0.337, P = .008; Figure 1C). Furthermore, GVHD-free survival was significantly better in F→F compared with M→M SCT (hazard ratio = 0.547, P = .043; data not shown).
In summary, we support the existence of a birth order effect as reported before.1,6 Additionally, we show that gender might be one of the causal factors. Interestingly, the birth order effect was significant in the adult female donor/female recipient SCT pairs. Our current plausible explanation is the intrauterine exposure to sibling antigens occurring during pregnancy, leading to minor H antigen experienced T-cell responses in women.4 These responses might lead to immune regulation.7 Subsequent (re-)exposure to fetal antigens during pregnancy of the donor herself explains the favorable younger female SCT donor in combination with the female recipient.
To get a clearer picture of the influence of minor H antigens on the birth order effect, we suggest a much larger cohort of HLA-identical sibling SCT with detailed information regarding family and obstetric history of both patient and donor.
Authorship
Contribution: M.D., E.S., and E.G. designed the research and drafted the manuscript; A.C., H.D., J.-F.E., J.E., T.G., B.K., D.L., P.L., and R.S. provided data; M.D., E.S., and M.H. collected data; and M.D., E.S., R.B., and E.G. analyzed results and prepared figures.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Eric Spierings, Laboratory for Translational Immunology, University Medical Center Utrecht, F03.821, Postbox 85500, 3508 GA, Utrecht, Netherlands; e-mail: e.spierings@umcutrecht.nl.