Abstract
Allogeneic hematopoietic stem cell transplantation (alloHSCT) remains the only curative option for multiple myeloma (MM). Unfortunately, relapses remain frequent and randomized controlled trials have yielded equivocal conclusions. Before these trials were published, selected patients were treated with alloHSCT, but factors affecting long-term success have not been clearly defined. We have analyzed our single-center cohort of MM patients receiving a myeloablative alloHSCT in the 1990's in order to evaluate the impact of several factors on outcomes.
We performed a retrospective data collection on all patients treated with myeloablative alloHSCT from a sibling donor at our institution. Probabilities of overall (OS) and progression-free survival (PFS), as well as relapse, nonrelapse mortality (NRM) and graft-versus-host disease (GVHD) incidences were estimated taking competing risks into account when appropriate. Regression analysis using Cox and Fine & Gray models were used to determine factors influencing outcomes. Severity of chronic GVHD was assessed by the proportion of survivors on systemic immunosuppressive therapy.
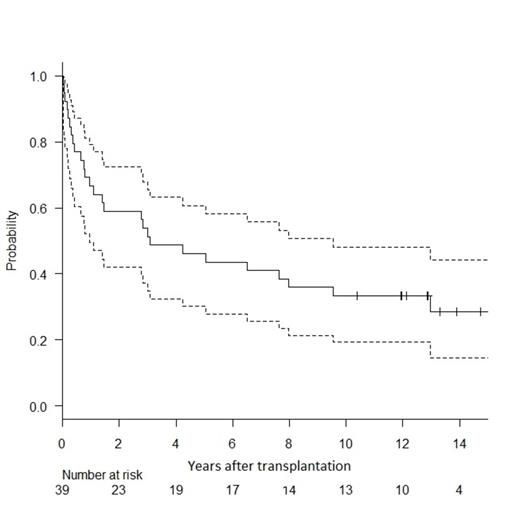
Between 1990 and 2001, 39 patients received a myeloablative alloHSCT. Median age was 46 years (range 24-53) and 68% had Durie-Salmon stage III disease. Twenty patients had received more than 4 cycles of prior chemotherapy and 4 patients had been treated with an autologous HSCT. Complete remission (CR) was achieved before allogeneic transplant in 31% patients. All but one donor were 6/6 HLA matches. AlloHSCT was performed within the first year of diagnosis in 69% of patients. Irradiation-based conditioning was used in 77%; stem cell source was bone marrow in 54% and peripheral blood (PB) in 46% of patients. With a median follow-up of 13 years, cumulative incidences of progression and NRM were 43% (95%CI: 26-59; Fig. 1) and 38% (22-54), respectively. Cumulative incidences of grade II-IV acute and extensive chronic GVHD were 29% (16-44) and 40% (24-55). Probabilities of 10-year OS and PFS were 33% (95%CI: 19-48; Fig. 2) and 29% (95%CI: 16-44) In multivariate analysis, the most significant protective factor against relapse was the use of PB as cell source (HR 0.34, CI: 0.14-0.82). The only protective factor for PFS was CR status before transplantation (HR 0.28, CI: 0.09-0.89). Nevertheless, the effect of these variables on overall survival was inconclusive (respectively: HR 0.51, CI 0.22-1.17, and HR 0.39, CI: 0.13-1.19). The time-dependent effect of chronic GVHD on PFS was also statistically non-significant (HR 0.47, CI: 0.14-1.59). The probability of being on systemic immunosuppressive treatment for GVHD in alive patients was 31% (CI: 13-58) at 10 years.
(left) shows cumulative incidence of progression with death in remission as competing risk (light grey).
(left) shows cumulative incidence of progression with death in remission as competing risk (light grey).
(right) shows the probability of overall survival with 95% confidence interval.
Myeloablative alloHSCT performed for MM in the 1990's in selected patients allowed a high probability of disease control but with major toxicity as shown by the high NRM risk. A third of patients are alive 10 years after transplantation. Achievement of CR before alloHSCT and the use of PB stem cells were protective against transplant failure. However, small sample size does not allow us to draw conclusions on the effect of other pre-transplant characteristics and GVHD on OS. The risk of relapse in our cohort being comparable to published results in frontline reduced-intensity alloHSCT, superiority of myeloablative HSCT for advanced disease can be hypothesized. Prohibitive NRM risk should encourage efforts to reduce early and late toxicity through better patient and donor selection, conditioning regimen and GVHD prophylaxis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.