Key Points
Endothelial Smad4 is a physiological suppressor that functions specifically during the transition to hematopoietic progenitors.
Endothelial Smad4 lies upstream of the subaortic microenvironment to control the hematopoietic fate of aortic endothelium.
Abstract
In mouse mid-gestational embryos, definitive hematopoietic stem progenitor cells are derived directly from a very small proportion of the arterial endothelium. However, the physiological mechanisms restraining excessive endothelial-hematopoietic transition remain elusive. We show here that genetic deletion of Smad4 from the endothelium stage (using Tie2-Cre), but not from embryonic hematopoietic cells (using Vav-Cre), leads to a strikingly augmented emergence of intra-arterial hematopoietic clusters and an enhanced in vitro generation of hematopoietic progenitors, with no increase in the proliferation and survival of hematopoietic cluster cells. This finding indicates a temporally restricted negative effect of Smad4 on the endothelial to hematopoietic progenitor transition. Furthermore, the absence of endothelial Smad4 causes an increased expression of subaortic bone morphogenetic protein 4 and an activation of aortic extracellular signal-regulated kinase, thereby resulting in the excessive generation of blood cells. Collectively, our data for the first time identify a physiological suppressor that functions specifically during the transition of endothelial cells to hematopoietic progenitors and further suggest that endothelial Smad4 is a crucial modulator of the subaortic microenvironment that controls the hematopoietic fate of the aortic endothelium.
Introduction
In mouse embryos, definitive hematopoiesis can be classified into 2 waves: the initial generation of multipotent hematopoietic progenitors, beginning at embryonic day (E) 8/8.5, and the later adult-repopulating hematopoietic stem cells (HSCs), starting from E10.5.1-3 Accumulating evidence from multiple research strategies has pinpointed that definitive hematopoietic progenitors and HSCs are directly formed from hemogenic endothelium, a unique type of structural endothelium with transient hematopoietic potential.4-8 This process is, therefore, acknowledged as the endothelial-hematopoietic transition, manifested intra-embryonically as the appearance of vascular hematopoietic clusters in the aorta, vitelline, and umbilical arteries.4,7,9 It is proposed that definitive hematopoietic progenitors and HSCs are generated from distinct types of hemogenic endothelium, implying that distinct molecular programming is involved; these mechanisms are as yet poorly defined.1-3,10 Of note, only a very small proportion of aortic endothelium has blood-forming capacity. In theory, physiological mechanisms restraining excessive endothelial-hematopoietic transition must exist, but remain largely unknown.
The transforming growth factor β (TGF-β) superfamily contains a large group of structurally related polypeptide growth factors, including TGF-βs, bone morphogenetic proteins (BMPs), activins, and others. Members of the TGF-β family signal through specific type I and type II transmembrane serine/threonine kinase receptors that activate intracellular mediator Smads. Smad2 and Smad3 are activated by the type I receptors of TGF-β and activin, whereas Smad1, Smad5, and Smad8 are phosphorylated in response to BMPs. Receptor-activated Smads then interact with Smad4 to form heteromeric complexes that are translocated into the nucleus. Activated TGF-β receptors can also transduce the signals through alternative Smad-independent pathways, such as mitogen-activated protein kinase, ras homolog family member A, and c-Jun N-terminal kinase.11
BMP4 has long been acknowledged to be pivotal in mesoderm induction and hematopoietic commitment, as revealed by studies in different species.12,13 Furthermore, BMP4 has been identified as a positive modulator of mouse HSC development in the context of an aorta‐gonad‐mesonephros (AGM) explant culture and transplantation assay.14 Nevertheless, a previous study using a fetal liver kinase 1 (Flk1)-Cre-mediated BMPRIA/ALK3 conditional knockout mouse model revealed a dispensable role for BMP receptor signaling in the generation of hematopoietic progenitors from Flk1+ mesoderm in vivo.15 To date, the physiological roles of certain TGF-β family members involved in the mammalian endothelial-hematopoietic transition remain largely unknown.
Currently, endothelial cell-specific combined with hematopoietic cell-specific gene knockout mouse models are used to explore candidate regulatory mechanisms implicated in hemogenic endothelium development.7,16,17 Using both Tie2-Cre and Vav-Cre transgenic mouse models, we show here that the deletion of Smad4 from the endothelium stage, but not from embryonic hematopoietic cells, caused an increased generation of hematopoietic clusters and progenitor cells. Furthermore, the absence of endothelial Smad4 caused an upregulation of subaortic BMP4 and an activation of aortic extracellular signal-regulated kinase (ERK), resulting in the excessive transition of endothelial cells to hematopoietic progenitors. In summary, we reveal a novel physiological inhibitor implicated specifically in the endothelial cell to hematopoietic progenitor transition in mouse embryos.
Methods
Animals
Mice carrying conditional Smad4 alleles (Smad4fl/fl),18 Tie2-Cre transgenic mice19 and ROSA-LacZ reporter mice20 have been reported elsewhere. Vav-Cre transgenic mice (strain name: B6.Cg-Tg(Vav1-cre)A2Kio/J)21 and ROSA-EYFP reporter mice (strain name: B6.129X1-Gt(ROSA)26Sortm1(EYFP)Cos/J)22 were purchased from The Jackson Laboratory. Animal care and embryo dissection are detailed in the supplemental Methods on the Blood Web site. Mice involved in the study were approved by the Animal Care and Use Committee and handled in accordance with institutional guidelines for laboratory animals.
Flow cytometric analysis
Cells were incubated with different antibodies for 30 minutes. The 7-amino-actinomycin D (7-AAD; eBioscience) was used to exclude dead cells. Stained cells were analyzed by fluorescence-activated cell sorting (FACS) with a FACSCalibur flow cytometer or sorted with an FACS Aria 2 flow cytometer (BD Biosciences). For cell cycle analysis, 5-bromo-2′-deoxyuridine (BrdU; BD Pharmingen) or Ki67 (BD Pharmingen) staining was performed. The 7-AAD was used to measure DNA content in the intracellular Ki67 staining. For apoptotic analysis, Annexin V (BD Pharmingen) staining was performed. Antibodies and procedures are detailed in the supplemental Methods. FACS data were analyzed with FlowJo software (Tree Star).
Hematopoietic assays
AGM culture from the caudal half of E9.0-E9.5 embryos was performed as described.23 After incubation for 5 to 10 days, the colonies generated in the culture were calculated and the cells were recovered by trypsinase digestion for flow cytometric analysis. Alternatively, the cultures were fixed for LacZ staining or immunostaining. For OP9/OP9-DL1 coculture, sorted Tie2+ cells from the caudal half were plated on an OP9/OP9-DL1 stromal layer in the presence of 50 ng/mL stem cell factor ([SCF]; PeproTech) and 10 ng/mL IL-3 (PeproTech), or a cytokine cocktail as previously described.24 After being cultured for 5 to 10 days, cells were harvested by mechanical pipetting for further analysis. Explant culture was carried out with the caudal half of E9.5 embryos as previously described.25 After 1-3 days at 37°C, explants were dissociated in collagenase for flow cytometry analysis. Hematopoietic assays are detailed in the supplemental Methods.
Histological analysis
Whole-mount immunostaining and confocal microscopy were performed as previously described.9 The primary antibodies used were anti-c-Kit (2B8, BD Biosciences) and biotinylated anti-CD31 (MEC13.3, BD Biosciences). LacZ staining and other immunostaining procedures are detailed in the supplemental Methods.
Statistical analysis
Data were evaluated using Student two-tail t test. P < .05 was considered to be statistically significant.
Results
Enhanced hemogenic activity of Smad4-deficient endothelium in vivo and in vitro
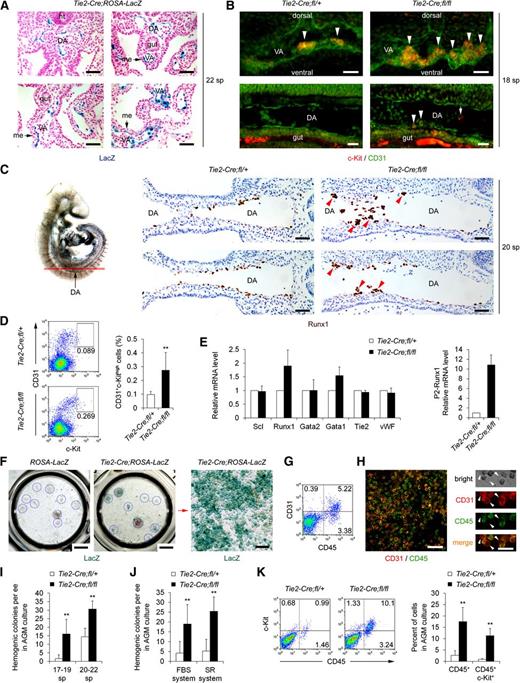
Tie2-Cre-mediated ablation of Smad4 leads to embryonic lethality at E10.5 due to cardiovascular defects.19 In the present study, E9.0 to early E9.5 (13-25 somite pairs [sp]) embryos were used, avoiding the influences secondary to the vascular defects. Unlike a previous study showing the Tie2-Cre-mediated excision in the mesenchymal cells surrounding the vitelline artery,26 the ablation activity of the Tie2-Cre transgene used here was restricted to the endothelial layer and blood cells inside the dorsal aorta and vitelline arteries at early E9.5 (Figure 1A). We found that at approximately 18 sp, CD31+c-Kit+ hematopoietic clusters were occasionally observed within the vitelline artery of the control embryos (Figure 1B), in accordance with a previous report.9 In contrast, the clearly increased numbers of hematopoietic clusters were detected in the vitelline arteries of Tie2-Cre;Smad4fl/fl embryos (Figure 1B and supplemental Figure 1). Moreover, CD31+c-Kit+ cells closely associated with the endothelial layer emerged in the mutant dorsal aorta, whereas such cluster cells were not detectable in the littermate controls (Figure 1B and supplemental Figure 1). Consistently, Runx1+ intra-aortic clusters with more than 5 cells were exclusively visualized within the dorsal aorta of Smad4 mutants, but not the littermate controls at 20 sp (Figure 1C). By flow cytometric analysis, we further quantified the hematopoietic cluster cells proven to be enriched in the CD31+c-Kithigh population9 and observed a significant 2.8-fold increase in the Smad4 mutants (Figure 1D).
Enhanced hemogenic activity of Smad4-deficient endothelium in vivo and in vitro. (A) Sections of β-D-galactosidase (LacZ)-stained Tie2-Cre;ROSA-LacZ double transgenic embryos at 22 sp. Scale bars: 50 μm. (B) Whole mount immunostaining of c-Kit (red) and CD31 (green) at 18 sp. Confocal images of the embryonic vitelline arteries (VA, upper, three-dimensional reconstructions with totally 15 μm thickness) and dorsal aortas (DA) (lower, representative single images) are shown. c-Kit+CD31+ clusters (upper, arrowheads) or cluster cells (lower, arrowheads) attached to the ventral side of CD31+ endothelial layer are shown. The arrow indicates a c-Kit+CD31− circulating cell in the aorta. Scale bars: 20 μm. (C) Immunohistochemistry staining of Runx1 in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos at 20 sp. Continuous sections for each genotype are shown. Arrowheads indicate the Runx1+ intra-aortic clusters with more than 5 cells exclusively in the Tie2-Cre;Smad4fl/fl embryos. The diagram on the left illustrates the location analyzed. Scale bars: 50 μm. (D) Representative FACS analysis of caudal half cells for c-Kit and CD31 expression (left). The graph to the right shows percentages of the gated populations (n = 8). (E) Real-time PCR analysis of RNA extracts from E9.5 caudal half. Relative expression fold to that of control embryos is shown (n = 4). (F) LacZ stained AGM cultures derived from E9.5 ROSA-LacZ transgenic embryos without (left) or with (middle and right) Tie2-Cre transgene. Blue cycles indicate individual colonies. Magnification (right) of the red boxed region in the macroscopic view (middle) is shown. Scale bars: left and middle, 200 mm; right, 100 μm. (G) Representative FACS analysis of the cells recovered from the E9.5 AGM culture. (H) CD31 (red) and CD45 (green) double immunostaining of an E9.5 AGM culture. Arrowheads denote the “budding” cells co-expressed CD31 and CD45 with the CD45 signals enriched in the detaching parts. Scale bars: left, 100 μm; right, 50 μm. (I-J) Graphs showing the numbers of colonies generated in the AGM cultures from Tie2-Cre;Smad4fl/fl and control embryos (n = 4). (K) Representative FACS analysis of cells derived from the AGM cultures (left). The graph to the right shows the percentages of different subpopulations (n = 3). Data are mean ± standard deviation. DA, dorsal aorta; ee, embryo equivalent; me, mesenchymal cells surrounding the vitelline artery; nt, neural tube; SR, serum replacement; VA, vitelline artery. **P < .01, compared with control embryos.
Enhanced hemogenic activity of Smad4-deficient endothelium in vivo and in vitro. (A) Sections of β-D-galactosidase (LacZ)-stained Tie2-Cre;ROSA-LacZ double transgenic embryos at 22 sp. Scale bars: 50 μm. (B) Whole mount immunostaining of c-Kit (red) and CD31 (green) at 18 sp. Confocal images of the embryonic vitelline arteries (VA, upper, three-dimensional reconstructions with totally 15 μm thickness) and dorsal aortas (DA) (lower, representative single images) are shown. c-Kit+CD31+ clusters (upper, arrowheads) or cluster cells (lower, arrowheads) attached to the ventral side of CD31+ endothelial layer are shown. The arrow indicates a c-Kit+CD31− circulating cell in the aorta. Scale bars: 20 μm. (C) Immunohistochemistry staining of Runx1 in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos at 20 sp. Continuous sections for each genotype are shown. Arrowheads indicate the Runx1+ intra-aortic clusters with more than 5 cells exclusively in the Tie2-Cre;Smad4fl/fl embryos. The diagram on the left illustrates the location analyzed. Scale bars: 50 μm. (D) Representative FACS analysis of caudal half cells for c-Kit and CD31 expression (left). The graph to the right shows percentages of the gated populations (n = 8). (E) Real-time PCR analysis of RNA extracts from E9.5 caudal half. Relative expression fold to that of control embryos is shown (n = 4). (F) LacZ stained AGM cultures derived from E9.5 ROSA-LacZ transgenic embryos without (left) or with (middle and right) Tie2-Cre transgene. Blue cycles indicate individual colonies. Magnification (right) of the red boxed region in the macroscopic view (middle) is shown. Scale bars: left and middle, 200 mm; right, 100 μm. (G) Representative FACS analysis of the cells recovered from the E9.5 AGM culture. (H) CD31 (red) and CD45 (green) double immunostaining of an E9.5 AGM culture. Arrowheads denote the “budding” cells co-expressed CD31 and CD45 with the CD45 signals enriched in the detaching parts. Scale bars: left, 100 μm; right, 50 μm. (I-J) Graphs showing the numbers of colonies generated in the AGM cultures from Tie2-Cre;Smad4fl/fl and control embryos (n = 4). (K) Representative FACS analysis of cells derived from the AGM cultures (left). The graph to the right shows the percentages of different subpopulations (n = 3). Data are mean ± standard deviation. DA, dorsal aorta; ee, embryo equivalent; me, mesenchymal cells surrounding the vitelline artery; nt, neural tube; SR, serum replacement; VA, vitelline artery. **P < .01, compared with control embryos.
In accordance with the in situ results, real-time polymerase chain reaction (PCR) revealed a 1.9-fold increase in Runx1 expression in the caudal half of Tie2-Cre;Smad4fl/fl embryos (Figure 1E). The proximal P2 promoter-driven Runx1 isoform (P2-Runx1) marks a hemogenic endothelium population.27,28 A striking 10.8-fold increased expression of P2-Runx1 in the caudal half of Smad4 mutant embryos was observed, which was highly suggestive of an augmented hemogenic activity by Smad4-deficient endothelium (Figure 1E).
We analyzed hemogenic potential in vitro with a modified AGM culture system.23 The Tie2-Cre-mediated ablation occurred in the colonies generated in the E9.5 AGM cultures (Figure 1F). FACS and immunofluorescence analysis documented a specific cell population coexpressing CD31 and CD45 (Figure 1G-H). Interestingly, we witnessed some “budding” cells with both CD31+CD45+ detaching part and CD31+CD45− adherent part (Figure 1H, right). This phenomenon highly suggested the occurrence of endothelial-hematopoietic transition in the culture system derived from E9.5 embryos. The hemogenic colonies were detectable starting at late E9.0 (17-18 sp), approaching the time-point that intraembryonic hematopoietic clusters are first detected in vivo,9 and the number of colonies increased in slightly older (20-22 sp) embryos (Figure 1I). Notably, Tie2-Cre;Smad4fl/fl embryos showed a remarkably increased number of colonies in the AGM culture (Figure 1I). The result in a serum-free culture system resembled that in cultures with serum (Figure 1J). Flow cytometric analysis demonstrated a significant increase in the frequencies of both CD45+ and CD45+c-Kit+ cells in the recovered cells derived from Smad4 mutant AGM cultures (Figure 1K). These data suggested an enhanced hemogenic potential from the Tie2-Cre;Smad4fl/fl embryos.
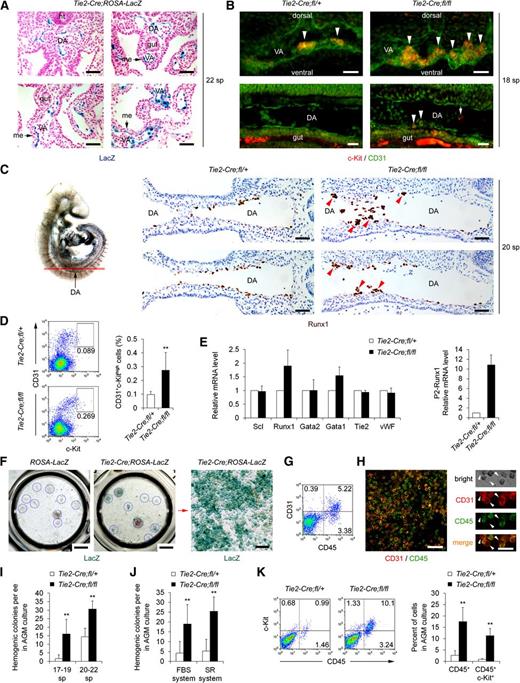
Increased hemogenesis in Tie2-Cre;Smad4fl/fl embryos is not due to abnormal hematopoietic proliferation, survival, or differentiation
We next investigated whether the increased generation of hematopoietic clusters in the Smad4 mutants was caused by enhanced cell proliferation or survival. The cellularity of the total cells, the putative endothelium (CD31+CD41−CD45−), and committed hematopoietic cells (CD41+/CD45+) in the caudal half did not change between the control and Smad4 conditional knockouts (Figure 2A and supplemental Figure 2A-B). Then the cell cycle status and apoptosis in CD31+ (predominantly endothelium), c-Kit+ (including hematopoietic progenitors), and CD31+c-Kithigh (intravascular cluster cells) subpopulations of the caudal half were analyzed (Figure 2B-D). In all of the subpopulations, the proportion of BrdU+ cells was comparable between cells derived from the control and Smad4 mutants (Figure 2B). Ki67 staining further showed that in the CD31+c-Kithigh population, the percentage of cycling cells (G1 + S/G2/M) was even slightly decreased in the Smad4 mutants (Figure 2C and supplemental Figure 2C). Furthermore, Smad4 deficiency did not alter the percentage of healthy (PI-Annexin V−) or apoptotic cells (Annexin V+) in all of the subpopulations assessed (Figure 2D and supplemental Figure 2D).
Increased hemogenesis in Tie2-Cre;Smad4fl/fl embryos is not due to abnormal hematopoietic proliferation, survival, or differentiation. (A) Graphs showing the absolute numbers of total cells (left) and CD31+CD41−CD45− endothelial cells (right) in the caudal half of Tie2-Cre;Smad4fl/fl and control embryos (n = 3). (B) Graph showing the percentage of BrdU+ cells within different subpopulations of the caudal half determined by FACS analysis (n = 3). No increase was detected in the Smad4 mutants as compared with the control embryos. (C) Representative FACS analysis of Ki67/7-AAD fluorescence in the CD31+ or c-Kit+ populations of the caudal half of Tie2-Cre;Smad4fl/fl and control embryos (upper). Graphs to the lower showing the cell cycle status within different subpopulations of the caudal half determined by FACS analysis of Ki67/7-AAD fluorescence (n = 4). (D) Graphs showing the apoptotic status within different subpopulations of the caudal half determined by FACS analysis of Annexin V/PI fluorescence (n = 5). No difference was detected in the Smad4 mutants as compared with the control embryos in all the groups. (E) Tie2+ cells from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos were cultured on OP9 for 7 to 9 days. Representative FACS analysis of cells generated in the cultures is shown. (F) Morphologic analysis of the sorted populations generated from Tie2+ caudal half cells in the OP9-DL1 coculture. Cytospin preparations are stained with May-Grunwald/Giemsa. Scale bar: 40 μm. (G) Graph to the left showing the frequencies of CFU-Cs in the individual sorted populations generated from Tie2+ caudal half cells in the OP9-DL1 coculture. Graph to the right showing the total number of CFU-Cs recovered from the OP9-DL1 coculture (n = 4). Data are mean ± standard deviation. NS, not significant. **P < .01.
Increased hemogenesis in Tie2-Cre;Smad4fl/fl embryos is not due to abnormal hematopoietic proliferation, survival, or differentiation. (A) Graphs showing the absolute numbers of total cells (left) and CD31+CD41−CD45− endothelial cells (right) in the caudal half of Tie2-Cre;Smad4fl/fl and control embryos (n = 3). (B) Graph showing the percentage of BrdU+ cells within different subpopulations of the caudal half determined by FACS analysis (n = 3). No increase was detected in the Smad4 mutants as compared with the control embryos. (C) Representative FACS analysis of Ki67/7-AAD fluorescence in the CD31+ or c-Kit+ populations of the caudal half of Tie2-Cre;Smad4fl/fl and control embryos (upper). Graphs to the lower showing the cell cycle status within different subpopulations of the caudal half determined by FACS analysis of Ki67/7-AAD fluorescence (n = 4). (D) Graphs showing the apoptotic status within different subpopulations of the caudal half determined by FACS analysis of Annexin V/PI fluorescence (n = 5). No difference was detected in the Smad4 mutants as compared with the control embryos in all the groups. (E) Tie2+ cells from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos were cultured on OP9 for 7 to 9 days. Representative FACS analysis of cells generated in the cultures is shown. (F) Morphologic analysis of the sorted populations generated from Tie2+ caudal half cells in the OP9-DL1 coculture. Cytospin preparations are stained with May-Grunwald/Giemsa. Scale bar: 40 μm. (G) Graph to the left showing the frequencies of CFU-Cs in the individual sorted populations generated from Tie2+ caudal half cells in the OP9-DL1 coculture. Graph to the right showing the total number of CFU-Cs recovered from the OP9-DL1 coculture (n = 4). Data are mean ± standard deviation. NS, not significant. **P < .01.
In the presence of SCF and IL-3, the coculture of E9.5 Tie2+ cells with OP9 or OP9-DL1 stromal cells for 7 to 9 days generates 3 populations, namely CD45+c-Kithigh, CD45+c-Kitlow, and CD45+c-Kit− cells (Figure 2E). Most of the CD45+c-Kithigh cells were CD34+, and the percentage of this population declined when cultured in the medium with a cytokine cocktail favoring hematopoietic differentiation, suggestive of their more immature nature compared with CD45+c-Kitlow cells (Figure 2E). The CD45+c-Kithigh cells appeared to be morphologically immature with a large and round nucleus based on May-Grunwald/Giemsa staining (Figure 2F), and had a higher frequency of colony-forming unit in culture (CFU-C) compared with the other 2 populations (Figure 2G). Of note, the Smad4 mutant cocultures demonstrated a remarkable 3.0- to 3.5-fold increase in the percentage of CD45+CD34+c-Kithigh cells (Figure 2E). Notably, neither cellular morphology nor the CFU-C frequency of the individually sorted populations showed an apparent difference between cells derived from Smad4 mutants and controls, although the total colony number recovered from OP9/OP9-DL1 coculture was considerably increased in Tie2-Cre;Smad4fl/fl embryos (Figure 2F-G). The results suggested that the deletion of Smad4 in Tie2-derived cells led to the enhanced generation of hematopoietic progenitors, but did not affect subsequent hematopoietic differentiation. Supportively, Karlsson et al29 have reported that the clonogenicity and proliferation of hematopoietic progenitors in vitro are not perturbed by the absence of Smad4.
Deletion of Smad4 by Vav-Cre has no influence on hematopoietic progenitor generation and homeostasis
To further exclude the possibility that Smad4 continues to play a role in hematopoietic cells once the endothelial-hematopoietic transition is complete, we used the Vav-Cre transgene, the expression of which is reported to be restricted to hematopoietic cells.7 We first evaluated the excision of the ROSA-EYFP allele by Vav-Cre in certain populations along the endothelial-hematopoietic transition process in the caudal half of E10.5 embryos. In contrast to the high ablation efficacy of the Tie2-Cre transgene, the Vav-Cre-mediated ablation occurred in 28.6% of the CD31+c-Kithigh intravascular cluster cells and nearly 50% of the hematopoietic cells, but only in a very small proportion of the CD41−CD45-Ter119−CD31+ putative endothelial cells (Figure 3A). The deletion of Smad4 via Vav-Cre did not affect fetal or adult viability, as previously reported.30 No difference in the number of intravascular hematopoietic clusters could be detected between the Vav-Cre;Smad4fl/fl and control embryos at E10.5 by whole-mount immunostaining or flow cytometry (Figure 3B-C). The result was further confirmed at E11.5 when the efficiency of the Vav-Cre-mediated excision was much higher, which was 61% in the CD31+c-Kithigh intravascular cluster cells and nearly 70% in the hematopoietic progenitors (Figure 3D-E and supplemental Figure 3A). From the data, it was suggested that Smad4 was dispensable after hematopoietic clusters were generated.
Deletion of Smad4 by Vav-Cre has no influence on hematopoietic progenitor generation and homeostasis. (A) Representative FACS analysis of EYFP fluorescence in the gated subpopulations (blue boxes) of E10.5 Tie2-Cre;ROSA-EYFP (upper) and E10.5 Vav-Cre;ROSA-EYFP (lower) AGM regions, respectively. The ROSA-EYFP littermate without the Cre transgene serves as the negative controls (red lines). (B) Whole mount immunostaining of c-Kit (red) and CD31 (green) at E10.5. Confocal images of the aorta region of Vav-Cre;Smad4fl/fl and control embryos are shown (three-dimensional reconstructions with totally 120 μm thickness). Higher magnification images of representative clusters are shown to the right, respectively. Scale bars: 40 μm. (C) Representative FACS analysis of E10.5 AGM cells for CD31+c-Kithigh expression (left). The graph to the right shows the percentages of the gated populations (n = 3). (D) Representative FACS analysis of EYFP fluorescence in the CD31+c-Kithigh and CD41lowc-Kit+ subpopulations of the E11.5 Vav-Cre;ROSA-EYFP AGM region. The ROSA-EYFP littermate without the Cre transgene serves as the negative controls (red lines). (E) Representative FACS analysis of E11.5 AGM cells for CD31+c-Kithigh and CD41lowc-Kit+ expression (left). The graphs to the right show the percentages of the gated populations (n = 3). (F) Representative FACS analysis of EYFP fluorescence in the hematopoietic progenitors (CD45+c-Kit+) and hematopoietic cells (CD45+) of the E12.5 Vav-Cre;ROSA-EYFP fetal liver. The ROSA-EYFP littermate without the Cre transgene serves as the negative controls (red lines). (G) Graphs showing the frequencies of hematopoietic progenitors and hematopoietic cells in the E12.5 fetal liver of Vav-Cre;Smad4fl/fl and control embryos (n = 3). (H) Graph showing the number of hematopoietic colonies in the E11.5 AGM region of Vav-Cre;Smad4fl/fl and control embryos (n = 3). (I) Graphs showing the number of hematopoietic colonies in the E12.5 fetal liver of Vav-Cre;Smad4fl/fl and control embryos (n = 3). Data are mean ± standard deviation. DA, dorsal aorta; NS, not significant.
Deletion of Smad4 by Vav-Cre has no influence on hematopoietic progenitor generation and homeostasis. (A) Representative FACS analysis of EYFP fluorescence in the gated subpopulations (blue boxes) of E10.5 Tie2-Cre;ROSA-EYFP (upper) and E10.5 Vav-Cre;ROSA-EYFP (lower) AGM regions, respectively. The ROSA-EYFP littermate without the Cre transgene serves as the negative controls (red lines). (B) Whole mount immunostaining of c-Kit (red) and CD31 (green) at E10.5. Confocal images of the aorta region of Vav-Cre;Smad4fl/fl and control embryos are shown (three-dimensional reconstructions with totally 120 μm thickness). Higher magnification images of representative clusters are shown to the right, respectively. Scale bars: 40 μm. (C) Representative FACS analysis of E10.5 AGM cells for CD31+c-Kithigh expression (left). The graph to the right shows the percentages of the gated populations (n = 3). (D) Representative FACS analysis of EYFP fluorescence in the CD31+c-Kithigh and CD41lowc-Kit+ subpopulations of the E11.5 Vav-Cre;ROSA-EYFP AGM region. The ROSA-EYFP littermate without the Cre transgene serves as the negative controls (red lines). (E) Representative FACS analysis of E11.5 AGM cells for CD31+c-Kithigh and CD41lowc-Kit+ expression (left). The graphs to the right show the percentages of the gated populations (n = 3). (F) Representative FACS analysis of EYFP fluorescence in the hematopoietic progenitors (CD45+c-Kit+) and hematopoietic cells (CD45+) of the E12.5 Vav-Cre;ROSA-EYFP fetal liver. The ROSA-EYFP littermate without the Cre transgene serves as the negative controls (red lines). (G) Graphs showing the frequencies of hematopoietic progenitors and hematopoietic cells in the E12.5 fetal liver of Vav-Cre;Smad4fl/fl and control embryos (n = 3). (H) Graph showing the number of hematopoietic colonies in the E11.5 AGM region of Vav-Cre;Smad4fl/fl and control embryos (n = 3). (I) Graphs showing the number of hematopoietic colonies in the E12.5 fetal liver of Vav-Cre;Smad4fl/fl and control embryos (n = 3). Data are mean ± standard deviation. DA, dorsal aorta; NS, not significant.
By E12.5, more than 80% of the immunophenotypically defined HSCs (Lin−CD48−CD150+Mac1lowSca-1+), hematopoietic progenitors (CD45+c-Kit+), and hematopoietic cells (CD45+) in the fetal liver of Vav-Cre;ROSA-EYFP double transgenic embryos were YFP+ (Figure 3F and supplemental Figure 3B). Importantly, the deletion of Smad4 by Vav-Cre did not affect fetal liver cellularity, cell viability, or the frequencies of phenotypically defined hematopoietic stem progenitor cells (Figure 3G and supplemental Figure 3C-D). Functionally, hematopoietic colonies were highly enriched in the YFP+ populations in either the E11.5 AGM region or the E12.5 fetal liver of the Vav-Cre;ROSA-EYFP embryos (supplemental Figure 4A-B). Of note, the colony-forming capacity was quite comparable between the control and Vav-Cre;Smad4fl/fl embryos (Figure 3H-I and supplemental Figure 4C-D). Additionally, no difference in the number of immunophenotypically defined HSCs or colony-forming capacity was detected between Vav-Cre;Smad4fl/fl and control adult mice (supplemental Figure 5A-D). Thus, Smad4 was no longer functioning as a suppressor in hematopoietic cells from the embryonic stage.
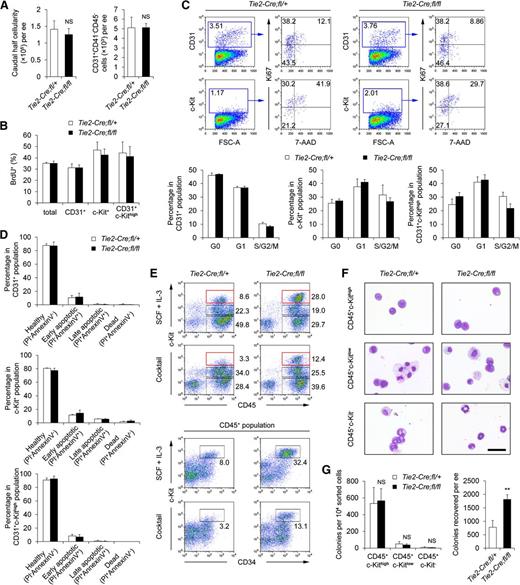
Smad4 deficiency in the endothelium results in a gain-of-BMP4 function in hemogenesis
Endothelial Smad4 has been reported to be involved in endothelium-mural cell interaction,19,31 and the subaortic mesenchyme in the mid-gestational embryo serves as the supportive microenvironment for blood emergence.32,33 To explore the possible role of the Tie2− stromal cells from Tie2-Cre;Smad4fl/fl embryos in the enhanced hemogenesis, we sorted Tie2+ and Tie2− populations from the Smad4 mutant and the control caudal half, respectively, and reciprocally mixed them in the AGM culture (Figure 4A). No hemogenic colonies could be generated from Tie2− cells alone (data not shown). Importantly, for both the control and Tie2-Cre;Smad4fl/fl embryo-derived Tie2+ cells, adding Tie2− cells from Tie2-Cre;Smad4fl/fl embryos, compared with those from control embryos, increased the production of hemogenic colonies and consequently CD45+ cells and CD45+c-Kit+ hematopoietic progenitors (Figure 4A). These data highly suggested the presence of an aberrant niche within the Tie2-Cre;Smad4fl/fl embryos.
Smad4 deficiency in the endothelium results in a gain-of-BMP4 function in hemogenesis. (A) Sorted Tie2+ and Tie2− cells from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos, respectively, were reciprocally mixed in the AGM culture. Colonies generated (left, n = 4) and different subpopulations detected by FACS (right, n = 2) are shown. fl/+, Tie2-Cre;Smad4fl/+; fl/fl, Tie2-Cre;Smad4fl/fl. (B) Real-time PCR analysis of gene expression in the caudal half of Tie2-Cre;Smad4fl/fl and control embryos. Relative expression fold to that of control embryos is shown (n = 3). (C) Immunofluorescence staining of BMP4 (green) and endomucin (red) in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos, showing the increased expression of BMP4 around the aorta of mutant embryo. Nuclei were stained with DAPI (blue). Scale bars: 50 μm. (D) Immunohistochemistry staining of pSmad1/5/8 in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos. Arrowheads indicate the pSmad1/5/8-positive aortic endothelium. Scale bars: 50 μm. (E) Real-time PCR analysis of gene expression in the sorted Tie2+ (left) and Tie2− (right) populations derived from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos. Relative expression fold to that of control embryos is shown (n = 3). (F) Graph showing the hemogenic colonies generated in the AGM cultures derived from E9.5 embryos. BMP4 addition significantly increases the colony generation in the AGM cultures (n = 6). (G) Caudal half Tie2+ cells from E9.5 embryos were cultured on OP9-DL1 with or without BMP4 for 7 to 9 days. Representative FACS analysis of cells generated in the cultures is shown. Data are mean ± standard deviation. DA, dorsal aorta; nt, neural tube. *P < .05; **P < .01.
Smad4 deficiency in the endothelium results in a gain-of-BMP4 function in hemogenesis. (A) Sorted Tie2+ and Tie2− cells from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos, respectively, were reciprocally mixed in the AGM culture. Colonies generated (left, n = 4) and different subpopulations detected by FACS (right, n = 2) are shown. fl/+, Tie2-Cre;Smad4fl/+; fl/fl, Tie2-Cre;Smad4fl/fl. (B) Real-time PCR analysis of gene expression in the caudal half of Tie2-Cre;Smad4fl/fl and control embryos. Relative expression fold to that of control embryos is shown (n = 3). (C) Immunofluorescence staining of BMP4 (green) and endomucin (red) in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos, showing the increased expression of BMP4 around the aorta of mutant embryo. Nuclei were stained with DAPI (blue). Scale bars: 50 μm. (D) Immunohistochemistry staining of pSmad1/5/8 in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos. Arrowheads indicate the pSmad1/5/8-positive aortic endothelium. Scale bars: 50 μm. (E) Real-time PCR analysis of gene expression in the sorted Tie2+ (left) and Tie2− (right) populations derived from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos. Relative expression fold to that of control embryos is shown (n = 3). (F) Graph showing the hemogenic colonies generated in the AGM cultures derived from E9.5 embryos. BMP4 addition significantly increases the colony generation in the AGM cultures (n = 6). (G) Caudal half Tie2+ cells from E9.5 embryos were cultured on OP9-DL1 with or without BMP4 for 7 to 9 days. Representative FACS analysis of cells generated in the cultures is shown. Data are mean ± standard deviation. DA, dorsal aorta; nt, neural tube. *P < .05; **P < .01.
Among the proposed niche components for AGM hematopoietic development,14,34 the expression levels of TGF-β/BMP and Hedgehog pathway members were checked, and an obvious upregulation of BMP4 in the caudal half of Smad4 conditional knockouts was detected (Figure 4B). Immunofluorescent staining further showed that in the Tie2-Cre;Smad4fl/fl embryos, BMP4 expression was increased in the mesenchyme surrounding the aorta, and the polarized distribution of BMP4 was apparently disturbed (Figure 4C). The increased BMP4 signaling in the Smad4 mutants was further confirmed by the increased expression of pSmad1/5/8 in the aortic endothelium (Figure 4D). BMP4 in Tie2+ cells showed a modest 1.3-fold upregulation in Tie2-Cre;Smad4fl/fl embryos compared with the controls, whereas Tie2− stromal-derived BMP4 exhibited a more evident 1.9-fold increase (Figure 4E), in accordance with the in situ observation.
Functionally, the addition of BMP4 to the AGM culture led to a significant increase in hemogenic colony generation (Figure 4F), with a concomitant augmentation of CD45+ cell production (Figure 5A). BMP4 treatment also caused an obvious increase in CD45+c-Kithigh frequency in the OP9-DL1 coculture (Figure 4G). Therefore, extrinsic BMP4 largely recapitulated the behavior of cells derived from Tie2-Cre;Smad4fl/fl embryos (Figure 1I-K and Figure 2E). Furthermore, we used E9.5 caudal half explant cultures to assess the influence of BMP4 on the generation of intravascular clusters by flow cytometric quantification of CD31+c-Kithigh cells. After 2 days of incubation with BMP4, the explants contained markedly more CD31+c-Kithigh cells compared with the vehicle-treated controls (Figure 5B), mimicking the change in Tie2-Cre;Smad4fl/fl embryos. Therefore, the upregulation of BMP4 beneath the endothelial layer of the dorsal aorta in Tie2-Cre;Smad4fl/fl embryos appeared to be involved in positively regulating the endothelial cell to hematopoietic progenitor transition.
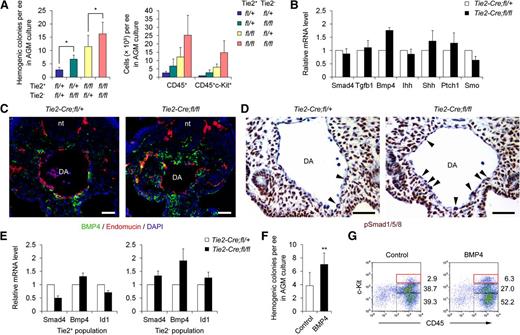
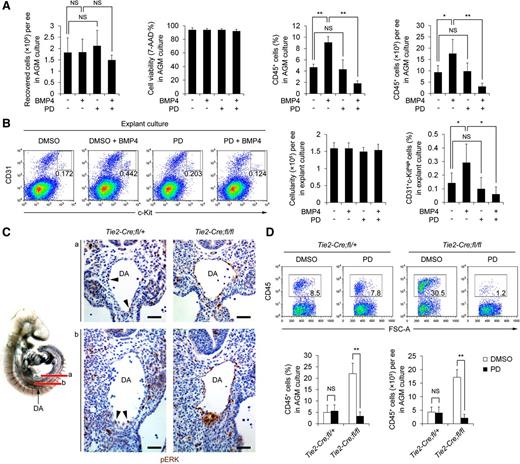
Increased activation of ERK is responsible for the enhanced hemogenesis in Tie2-Cre;Smad4fl/fl embryos. (A) Graphs showing the absolute number of recovered cells, the cell viability determined by 7-AAD staining, and the frequencies and total numbers of CD45+ cells generated in the AGM cultures derived from E9.5 embryos (n = 4). BMP4 and/or PD 98059 were added as indicated. (B) Caudal half of E9.5 embryos were cultured as explants in the presence of BMP4 and/or PD 98059. Representative FACS analysis for CD31+c-Kithigh expression is shown (left). The graphs to the right denote the cellularity recovered and the percentages of the gated populations in the explant cultures (n = 3). (C) Immunohistochemistry staining of pERK in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos, showing apparently increased expression of endothelial pERK in the mutants. Arrowheads indicate the pERK-positive aortic endothelium in the control embryos. The diagram on the left illustrates locations analyzed. Scale bars: 50 μm. (D) AGM cultures derived from E9.5 embryos were performed and PD 98059 was added as indicated. Representative FACS analysis for CD45 expression is shown (upper). The graphs to the lower denote the frequencies and the total numbers of CD45+ cell generated in the cultures (n = 4). Data are mean ± SD. DA, dorsal aorta; NS, not significant. *P < .05; **P < .01.
Increased activation of ERK is responsible for the enhanced hemogenesis in Tie2-Cre;Smad4fl/fl embryos. (A) Graphs showing the absolute number of recovered cells, the cell viability determined by 7-AAD staining, and the frequencies and total numbers of CD45+ cells generated in the AGM cultures derived from E9.5 embryos (n = 4). BMP4 and/or PD 98059 were added as indicated. (B) Caudal half of E9.5 embryos were cultured as explants in the presence of BMP4 and/or PD 98059. Representative FACS analysis for CD31+c-Kithigh expression is shown (left). The graphs to the right denote the cellularity recovered and the percentages of the gated populations in the explant cultures (n = 3). (C) Immunohistochemistry staining of pERK in the aorta region of Tie2-Cre;Smad4fl/fl and control embryos, showing apparently increased expression of endothelial pERK in the mutants. Arrowheads indicate the pERK-positive aortic endothelium in the control embryos. The diagram on the left illustrates locations analyzed. Scale bars: 50 μm. (D) AGM cultures derived from E9.5 embryos were performed and PD 98059 was added as indicated. Representative FACS analysis for CD45 expression is shown (upper). The graphs to the lower denote the frequencies and the total numbers of CD45+ cell generated in the cultures (n = 4). Data are mean ± SD. DA, dorsal aorta; NS, not significant. *P < .05; **P < .01.
Increased activation of ERK is responsible for the enhanced hemogenesis in Tie2-Cre;Smad4fl/fl embryos
We speculated that BMP4 must signal through a non-Smad pathway in the absence of Smad4 to promote hemogenesis. We found that the MEK inhibitor PD 98059 did not affect the generation of hemogenic colonies and hematopoietic cells in wild type E9.5 AGM cultures, but that the stimulating role of BMP4 was completely abrogated (Figure 5A). Similarly, in E9.5 caudal half explant cultures, PD 98059 alone had no apparent influence on the generation of CD31+c-Kithigh cells, but completely abolished the positive effect of BMP4 (Figure 5B and supplemental Figure 6A).
To determine whether a non-Smad pathway was activated in the absence of Smad4, we assessed mitogen-activated protein kinase signaling in situ. At approximately 20 sp, the phosphorylated ERK (pERK) signal was detected in a few aortic endothelial cells of the control embryos. In sharp contrast, more than half of the aortic endothelium in Tie2-Cre;Smad4fl/fl embryos expressed pERK, whereas the expression in areas other than the dorsal aorta was quite comparable between the mutant and controls (Figure 5C).
We further evaluated the contribution of ERK activation to the augmented hemogenic activity in Tie2-Cre;Smad4fl/fl embryos. Inhibition of ERK activation in the AGM cultures from early E9.5 embryos (20-23 sp) did not affect hemogenesis (Figure 5D), which is consistent with the finding that ERK was seldom activated in the aortic endothelium. Strikingly, the addition of PD 98059 to the culture completely blocked the increase in hemogenic colonies and hematopoietic cell generation from the Tie2-Cre;Smad4fl/fl embryos (Figure 5D and supplemental Figure 6B). Hence, ERK activation is required for the enhanced hemogenesis in Smad4 mutants. Taken together, the notion that the increased stromal BMP4 in Tie2-Cre;Smad4fl/fl embryos signaled through the endothelial ERK pathway to facilitate hemogenesis was supported by the data.
Activated c-Kit signaling is functionally required for the enhanced hemogenesis in Tie2-Cre;Smad4fl/fl embryos
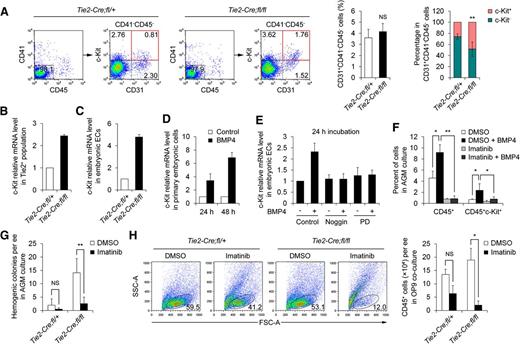
By flow cytometry, we found that the frequency of c-Kit+ cells in the putative endothelium (CD31+CD41−CD45−) was significantly increased in Tie2-Cre;Smad4fl/fl embryos, despite a comparable endothelial pool (Figure 6A). By real-time PCR, we observed a consistent upregulation of c-Kit transcripts in the Tie2+ population and in the immortalized endothelial cells derived from Smad4 mutants (Figure 6B-C). Then we investigated the possible regulation and function of endothelial c-Kit signaling in the augmented hematopoietic cell production in Tie2-Cre;Smad4fl/fl embryos.
Activated c-Kit signaling is functionally required for the enhanced hemogenesis in Tie2-Cre;Smad4fl/fl embryos. (A) Representative FACS analysis of the caudal half cells from Tie2-Cre;Smad4fl/fl and control embryos, showing obviously increased proportion of CD41−CD45-CD31+c-Kit+ cells (red quadrant) in the Smad4 mutants (left). The graphs to the right show the percentages of the putative endothelium (CD31+CD41−CD45−) and relative c-Kit+ and c-Kit− proportions within the CD31+CD41−CD45− population (n = 8). (B) Real-time PCR analysis of c-Kit expression in the sorted Tie2+ populations derived from the caudal half of E9.5 embryos (n = 3). (C) Real-time PCR analysis of c-Kit expression in the immortalized endothelial cells derived from Smad4 mutant and control embryos (n = 3). Relative expression fold to that of control embryos is shown. (D) Real-time PCR analysis of c-Kit expression in E9.5 primary embryonic cells treated with BMP4 for the indicated periods (n = 3). (E) Real-time PCR analysis of c-Kit expression in the immortalized embryonic endothelium line treated by the indicated regents for 24 hours (n = 3). Relative expression fold to that of control group is shown. (F) AGM cultures derived from E9.5 embryos were performed and BMP4 and/or imatinib were added as indicated. Graph showing the percentages of different subpopulations in the cultures determined by FACS analysis (n = 3). (G) Graph showing the hemogenic colonies generated in the AGM cultures from Tie2-Cre;Smad4fl/fl and control embryos with or without imatinib (n = 4). (H) Tie2+ cells from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos were cultured on OP9 with or without imatinib for 7 to 9 days. Representative FACS analysis of cells generated in the cultures is shown (left). The graph to the right denotes the numbers of CD45+ cells generated in the cultures (n = 3). Data are mean ± standard deviation. h, hours; NS, not significant. *P < .05; **P < .01.
Activated c-Kit signaling is functionally required for the enhanced hemogenesis in Tie2-Cre;Smad4fl/fl embryos. (A) Representative FACS analysis of the caudal half cells from Tie2-Cre;Smad4fl/fl and control embryos, showing obviously increased proportion of CD41−CD45-CD31+c-Kit+ cells (red quadrant) in the Smad4 mutants (left). The graphs to the right show the percentages of the putative endothelium (CD31+CD41−CD45−) and relative c-Kit+ and c-Kit− proportions within the CD31+CD41−CD45− population (n = 8). (B) Real-time PCR analysis of c-Kit expression in the sorted Tie2+ populations derived from the caudal half of E9.5 embryos (n = 3). (C) Real-time PCR analysis of c-Kit expression in the immortalized endothelial cells derived from Smad4 mutant and control embryos (n = 3). Relative expression fold to that of control embryos is shown. (D) Real-time PCR analysis of c-Kit expression in E9.5 primary embryonic cells treated with BMP4 for the indicated periods (n = 3). (E) Real-time PCR analysis of c-Kit expression in the immortalized embryonic endothelium line treated by the indicated regents for 24 hours (n = 3). Relative expression fold to that of control group is shown. (F) AGM cultures derived from E9.5 embryos were performed and BMP4 and/or imatinib were added as indicated. Graph showing the percentages of different subpopulations in the cultures determined by FACS analysis (n = 3). (G) Graph showing the hemogenic colonies generated in the AGM cultures from Tie2-Cre;Smad4fl/fl and control embryos with or without imatinib (n = 4). (H) Tie2+ cells from the caudal half of Tie2-Cre;Smad4fl/fl and control embryos were cultured on OP9 with or without imatinib for 7 to 9 days. Representative FACS analysis of cells generated in the cultures is shown (left). The graph to the right denotes the numbers of CD45+ cells generated in the cultures (n = 3). Data are mean ± standard deviation. h, hours; NS, not significant. *P < .05; **P < .01.
Sequence analysis of the c-Kit promoter identified a Smad4 binding site at −364 bp and a Smad binding site at +85 bp. By analyzing the effect of Smad4 knockdown on the expression and promoter activity of c-Kit in the embryonic endothelial cells, we found that the absence of Smad4 directly downregulated c-Kit expression in a cell autonomous manner, contrary to the in vivo finding (supplemental Figure 7A-B). Next we explored whether a noncell autonomous effect existed regarding the increased c-Kit expression in the absence of endothelial Smad4 in vivo. We detected an evident increase in c-Kit transcripts after BMP4 treatment in both primary embryonic cells and immortalized embryonic endothelium in a time-dependent manner (Figure 6D-E and supplemental Figure 8A-B). Importantly, the upregulation could be completely blocked by PD 98059 (Figure 6E), indicating that the BMP4-mediated elevation of c-Kit expression in the embryonic endothelium occurs largely through an alternative Smad-independent pathway. It has been reported that certain TGF-β superfamily members modulate c-Kit expression in different systems.35 For other TGF-β family members and antagonists, including activin A, TGF-β1, SB-431542, and Noggin, none of them showed an apparent influence on embryonic c-Kit expression (supplemental Figure 8A-B).
The addition of imatinib, a potent inhibitor of SCF/c-Kit signaling36 to the AGM culture abrogated the positive roles of BMP4 in hematopoietic cells generation (Figure 6F). Imatinib-mediated inhibition of SCF/c-Kit signaling could also completely reverse the increased production of hemogenic colonies in the Tie2-Cre;Smad4fl/fl embryos (Figure 6G). Furthermore, when Tie2+ cells derived from Tie2-Cre;Smad4fl/fl embryos were cocultured with OP9, the addition of imatinib led to a significant decrease in hematopoietic cell generation, in contrast to the control culture (Figure 6H). These results suggested a greater activation of c-Kit signaling in the Smad4 mutants. Interestingly, the inhibition of c-Kit signaling by imatinib treatment did not downregulate pERK expression in the endothelium of Tie2-Cre;Smad4fl/fl embryos (supplemental Figure 9), implying that the activation of endothelial ERK in the Smad4 mutants was not due to the increased activity of c-Kit signaling. Supportively, the most recent study has revealed a requirement of c-Kit for hemogenic endothelial cell specification.37
Discussion
Deciphering the molecular events that control the hemogenic fate of vascular endothelial cells during embryonic development is an important issue for better understanding how blood cells are generated and will have important implications in regeneration strategies. We speculate that apart from the intrinsic key regulators, some signals in endothelial cells can also function via other mechanisms, such as influencing the niche and/or overwhelming the alternative noncanonical pathways, to maintain appropriate hematopoietic program. In this study, we provide in vivo physiological evidence for a negative role of endothelial Smad4 specifically in the transition to hematopoietic progenitors, and suggest an endothelium-initiated change in the microenvironment as a modulator for this process.
Here, we deciphered the physiological role of a TGF-β/BMP-Smad signaling component in the development of hemogenic endothelium. Quite unexpectedly, as the central intracellular mediator of the canonical BMP pathway, Smad4 deficiency in the endothelium recapitulated the stimulating role of BMP4 on hemogenesis. Although a role for Smad-dependent BMP4 signaling in hematopoietic induction has been well-documented,38,39 we demonstrated a previously unknown requirement of ERK activity for the BMP4-promoted hemogenesis. Recently, Smad4 has been reported to be required for the upregulation of dual-specificity phosphatase 9 to inhibit ERK activity in embryonic stem cells.40 We could not exclude the possibility that the aberrant activation of aortic ERK in the Tie2-Cre;Smad4fl/fl embryos was partially due to the abolished inhibitory effect by Smad4 directly. Appropriate ERK activity is required for embryonic stem cell fate commitment.40,41 Our data suggest that in the aortic endothelium of mouse embryos, endogenous ERK activity should be tightly restricted, directly or indirectly by Smad4, to restrain excessive transition to hematopoietic progenitors. Thus, the signaling balance between Smad4 and ERK, 2 potent arms downstream of BMP4 signaling, determines the hemogenic fate choice by the aortic endothelium.
Hematopoietic fate decisions must be regulated by a complex network of niche signals linked to intrinsic pathways that have either a permissive or an inhibitory effect on the behavior of hemogenic endothelium.2,3,42 Currently, increasing studies have disclosed the molecular identities of the niche for regulating AGM hematopoiesis by affecting multiple cellular behaviors of hematopoietic cells.14,32,34,43 Most recently, the migration of the lateral plate mesoderm to the midline has been proven to be required for endothelial Runx1 expression to initiate aortic hematopoietic cluster generation in chick embryos.33 Nevertheless, how the endothelial-hematopoietic transition supporting microenvironment is physiologically modulated is unknown. Here, we provide in vivo evidence that in E9.5 embryos, the absence of endothelial Smad4 signaling leads to the increased expression of BMP4 in the mesenchymal layer in the vicinity of the dorsal aorta. Appropriate endothelium-mesenchyme interplay initiated by endothelial Smad4 is pivotal, therefore, to maintaining a proper blood-forming microenvironment. Actually, during embryonic blood vessel formation, endothelial cells induce the recruitment, differentiation, and proliferation of vascular smooth muscle cells via heterotypic cell-cell contact.44-46 Thus, it is conceivable that endothelial cell-derived signals, via similar manners, can also initiate the alteration in the adjacent mesenchymal niche for endothelial-hematopoietic transition. Further efforts to explore the complex orchestration of signaling between the endothelium and underlying mesenchyme are needed to gain further insight into the mechanisms of hemogenic endothelium development.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are very grateful to Professor Nancy Speck for helpful discussion and critical reading and modification of the manuscript. We thank Yan Zhang for sequence analysis of c-Kit promoter. We also thank Tomomasa Yokomizo for technical assistance on the whole-mount immunofluorescent staining. Thanks to Yu Zhang for OP9 and OP9-DL1 stromal cells, Chuxia Deng for Smad4fl/fl mice, and Xizhi Guo for ROSA-EYFP reporter mice.
This work was funded by the Chinese National Key Program on Basic Research (2011CB964800, 2012CB945100, 2012CB966904, and 2012CB966604), the National Natural Science Foundation of China (31030040, 81370596, 31371185, 30911130360, 81090410, 30900570, 31171410, 31171396, and 31271553), and the State Key Laboratory of Proteomics Grant (SKLP-K201102). This manuscript has been seen and approved by all authors.
Authorship
Contribution: Y.L., B.L., and X.Y. designed the study and experiments. Y.L., W.H., Z.L., Y.W., J.W., and J.G. performed experiments. W.W. and T.C. provided scientific input and reagents. Y.L., B.L., and X.Y. analyzed data and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Yu Lan, Institute of Biotechnology, Dongdajie 20, Beijing, 100071, China; e-mail: rainyblue_1999@126.com; and Bing Liu, Affiliated Hospital of Academy of Military Medical Sciences, Dongdajie 8, Beijing, 100071, China; e-mail: bingliu17@yahoo.com; and Xiao Yang, Institute of Biotechnology, Dongdajie 20, Beijing, 100071, China; e-mail: yangx@bmi.ac.cn.
References
Author notes
Y.L. and W.H. contributed equally to this study.