Abstract
Differentiation syndrome (DS), formerly known as retinoic acid syndrome, is a relatively common and potentially severe complication seen in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and/or arsenic trioxide. The full-blown syndrome consists of unexplained fever, weight gain, dyspnea with pulmonary infiltrates, pleuropericardial effusion, hypotension, and renal failure. Most measures currently used for management of DS have very little evidence-based support, and therefore, many remain controversial. Despite the lack of evidence supporting DS prophylaxis, several groups have adopted a preventive strategy with corticosteroids, especially for patients with leukocyte levels higher than from 5 to 10 × 109/L. DS diagnosis should be suspected in the presence of any of the above-mentioned signs and symptoms, and preemptive treatment with dexamethasone should be started immediately. Other supportive measures can also be crucial for the correct management of DS, especially in those patients with life-threatening complications. Temporary discontinuation of all-trans retinoic acid or arsenic trioxide is indicated only for patients in very poor clinical condition or with severe renal or pulmonary dysfunction, sometimes requiring admission to the intensive care unit. Recognition of specific biomarkers and a better understanding of DS pathogenesis can be helpful for the development of specific therapies to counteract DS in a timely manner.
Introduction
Differentiation syndrome (DS), originally described as retinoic acid syndrome, is a relatively common and serious complication that can occasionally be life-threatening in patients with acute promyelocytic leukemia (APL) undergoing induction therapy with all-trans retinoic acid (ATRA) and/or arsenic trioxide (ATO). The full-blown syndrome is characterized by unexplained fever, weight gain, peripheral edema, dyspnea with interstitial pulmonary infiltrates, pleuropericardial effusion, hypotension, and acute renal failure.1
Although the pathogenesis of DS has not been entirely clarified, it has been speculated that ATRA would activate a cascade of pathophysiologic mechanisms, leading to a systemic inflammatory response syndrome (SIRS), endothelium damage with capillary leak syndrome, occlusion of microcirculation, and tissue infiltration. SIRS would be mediated by cytokine release from differentiating myeloid cells, such as interleukin 1 (IL-1), IL-β, IL-6, IL-8, and tumor necrosis factor α,2 whereas cathepsin G, a serine protease that is also a potent enhancer of capillary permeability, would mainly be involved in endothelium damage.3 It has been also suggested that ATRA would induce changes in the adhesive properties of APL cells that promote the aggregation of promyelocytes, leukostasis, and vessel occlusion, as well as leukocyte migration from the blood into tissue. All these mechanisms mediated by interaction of adhesion molecules such as intercellular adhesion molecule 2 and lymphocyte function-associated antigen 1 would contribute to the multiorgan failure seen in DS.4,5
In general, there is very little evidence-based clinical research on most measures currently used for the prevention and management of DS in patients with APL, and therefore, many issues remain controversial. Some of these issues were addressed in a recent Spanish Programa Español de Tratamientos en Hematología (PETHEMA) study carried out in a large series of patients.6 In this study, we established the incidence, severity, prognostic factors, and outcome of this complication in the context of patients with APL treated for induction with the AIDA regimen (ATRA plus idarubicin).7,8 Our experience with the management of DS has been extended recently to relapsed patients treated with ATO with or without ATRA.
In the present article, we discuss relevant clinical issues related to the prevention, diagnosis, and treatment of DS in patients with APL who receive ATRA, ATO, or both with or without chemotherapy for induction therapy. All sections are preceded by a clinical vignette of a patient who was admitted to our hospital and illustrate representative clinical scenarios regarding prevention, diagnosis, and treatment of DS. These and other less-representative scenarios in patients with or at risk of developing DS are discussed in light of current available evidence to assist physicians in terms of decision-making.
How do we prevent DS?
Case 1
A 27-year-old previously healthy man arrives at the emergency ward with bleeding diathesis and fatigue. His white blood cell count (WBC) is 33 × 109/L with 80% blasts, a hemoglobin level of 9.2 g/dL, and a platelet count of 6 × 109/L. A diagnosis of APL is suspected because of the morphology of the blasts and coagulation tests, with the latter showing biological signs of disseminated intravascular coagulation. ATRA treatment and liberal blood product support with fresh-frozen plasma, cryoprecipitate, and platelet transfusions are immediately started. Dexamethasone 2.5 mg/m2 every 12 hours is also started for DS prophylaxis. Peripheral blood and bone marrow samples are sent to the laboratory for morphologic, immunophenotypic, cytogenetic, and molecular analysis to confirm the diagnosis. Immunostaining with an anti–PML antibody displays a typical microspeckled pattern of APL. This allows for immediately starting chemotherapy with idarubicin 12 mg/m2 per day every other day, with a total of 4 doses. At this point, we should ask the following questions: Is DS prophylaxis needed? Should we take into account WBC count and other predictive factors? Which corticosteroids can be used, and for how long? Should we modify the chemotherapy regimen to reduce the risk of developing DS?
Despite the lack of strong evidence supporting the use of DS prophylaxis, several major groups have adopted some type of preventive strategy with corticosteroids (Table 1). Prophylaxis has been carried out mainly with prednisone,8-11 methylprednisolone,12 or dexamethasone,7,13-15 given during the entire duration of induction therapy9,11 or during a limited period of time, ranging from 5 to 15 days,8,10,12,15 for patients treated with ATRA plus chemotherapy or ATRA plus ATO. These prophylactic approaches were given to all patients with APL8-12 or only for those with a WBC count higher than 5 to 10 × 109/L at presentation or developing during induction therapy.7,13,14 These strategies to decrease the incidence and severity of DS in patients with APL with hyperleukocytosis have been based on the weak evidence provided by a few early reports.16,17 In this regard, the study by Wiley and Firkin16 showed, in a small series of patients treated with ATRA alone, a reduction in DS-related pulmonary complications when prednisone was given to patients with WBC counts higher than 10 × 109/L. An additional study of the European APL group17 also suggested that patients with WBC counts greater than 5 × 109/L and DS tended to need mechanical ventilation more frequently.
Approximately half of the patients treated with ATO-based regimens without chemotherapy develop leukocytosis, with a peak WBC count occurring at approximately 20 days after the first dose. In cases of marked hyperleukocytosis when ATO-based regimens are used, a frequent option is the administration of cytoreductive agents, such as hydroxyurea, anthracyclines, and gemtuzumab ozogamicin. However, the clinical benefit of this approach in terms of DS-related morbidity and morbidity is still unclear. In contrast, for patients with hyperleukocytosis treated with ATRA plus chemotherapy regimens, apart from the use of prophylactic corticosteroids, very early institution of chemotherapy is generally recommended. This policy is not only to control the coagulopathy but also to reduce the risk for DS, which is particularly high in this setting.18 However, modifications to the planned treatment based on the presence of high WBC counts are not supported by the available data and, therefore, are not recommended.
In an attempt to decrease the morbidity and mortality associated with DS after induction therapy with ATRA plus idarubicin, the PETHEMA LPA99 trial included a systematic 15-day prophylaxis with prednisone for all patients, regardless of WBC counts. This strategy resulted in a reduction of the incidence of severe DS compared with the previous LPA96 trial (11.3% vs 16.6%; P = .07), in which only patients with WBC count higher than 5 × 109/L received prophylaxis with dexamethasone.6 However, this apparent benefit in terms of the severity of DS did not translate into a significant improvement in the DS mortality rate (1.1% vs 1.4%).19 Therefore, in the most recent LPA 2005 trial, we returned to the original strategy of selective prophylaxis with a reduced dose of dexamethasone (2.5 mg/m2 per 12 hours intravenously for 15 days) for patients with WBC counts higher than 5 × 109/L before or during treatment with ATRA. An interim analysis of the first 402 patients included in this trial showed that this approach resulted in an overall DS-associated mortality rate of 1.0%.14 A selective prophylaxis strategy with dexamethasone for patients with hyperleukocytosis has been maintained in the ongoing PETHEMA LPA 2012 trial, but this approach has been extended to patients with increased serum creatinine levels, regardless of the WBC count, because an impaired renal function was also found to be an independent predictive factor of severe DS.19
Apart from the lack of solid evidence regarding the role of DS prophylaxis, an additional question raised is whether the only objective of prophylaxis should be to decrease not only direct but also indirect DS-related mortality. It should be noted that apart from those patients who die in the context of severe DS with apparently no other contributing cause of death, this complication has also been associated with both the development of severe hemorrhages20 and death resulting from hemorrhage.6 In addition, the exacerbation of the procoagulant state of APL observed with the development of DS4,21-23 may also lead to a higher incidence of thrombosis. In fact, in a PETHEMA study,6 we found that severe DS, especially the early form of the syndrome, was associated not only with coagulopathy and an increased use of blood products during induction but also with a significantly higher thrombosis rate compared with that in patients who did not present with or who developed a moderate DS. Given the relationship between DS and thrombohemorrhagic syndrome, it is reasonable to speculate that the development of drugs targeting the mechanisms underlying the coagulopathy may also prove useful in preventing DS. Among other potential causes of indirect DS-related morbidity and mortality, one might speculate that the use of corticosteroids, either for prophylaxis or treatment of DS, can increase the risk for infections. As far as we know, this specific issue has not been addressed in the literature, but our feeling is that in case of an effect, if any, this would be negligible. In fact, a PETHEMA study analyzing the causes of induction failure did not show an increased infectious mortality when corticosteroids were systematically used for all patients or when they were selectively used in patients with WBC counts higher than 5 × 109/L.19
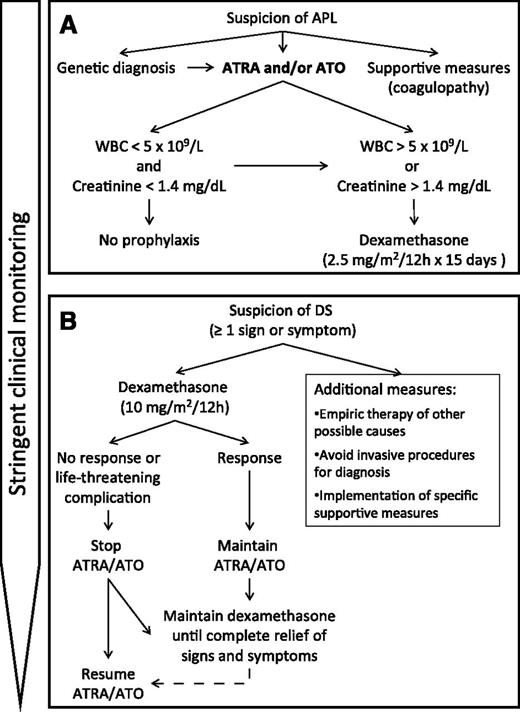
In summary, as mentioned earlier, we currently use selective DS prophylaxis with dexamethasone (2.5 mg/m2 per 12 hours intravenously for 15 days) for patients with WBC counts higher than 5 × 109/L at any time during induction therapy and in those with increased serum levels of creatinine (Figure 1A), but the benefit provided by this and any other DS prophylaxis is still debatable, with many unanswered questions; for example, is DS prophylaxis required, or can it be substituted by a preemptive approach? If needed, should prophylaxis be given to all patients or only selectively to those with a high risk of developing DS? What are the best corticosteroid, dose, and schedule to be used for DS prevention? Does the addition of cytoreductive agents, such as hydroxyurea, anthracycline, or gemtuzumab ozogamicin, provide any benefit for prevention of DS in patients with hyperleukocytosis? These and other questions still lack an evidence-based response; therefore, well-controlled randomized studies are warranted to answer these questions.
Current algorithm for the management of DS in the PETHEMA trials. (A) Prophylaxis. (B) Treatment.
Current algorithm for the management of DS in the PETHEMA trials. (A) Prophylaxis. (B) Treatment.
Regarding the predictive factors of developing DS, hyperleukocytosis seems the most consistently found related to the syndrome and its severity.6 Other factors, such as age and the presence of coagulopathy, have shown a marginal effect or had not independent prognostic value.
How do we diagnose and grade DS?
Case 2
A 34-year-old woman is admitted to the emergency ward with bleeding diathesis characterized by easy bruising, epistaxis, and bleeding gums. At presentation, her WBC count is 3.4 × 109/L, hemoglobin level is 10.7 g/dL, and platelet count is 27 × 109/L. Her coagulation studies indicate disseminated intravascular coagulation with reactive hyperfibrinolysis. A diagnosis of APL is confirmed by morphology and cytogenetic and molecular analysis. Remission induction with ATRA plus idarubicin (AIDA regimen) is initiated. Five days after starting ATRA, her WBC count rises to 8.7 × 109/L, and she develops peripheral edema, 5 kg weight gain, fever (38.5°C), and dyspnea. Her oxygen saturation is 82%. A chest X-ray reveals bilateral pulmonary infiltrates and an enlarged cardiac shadow with pleural effusion. Echocardiography shows moderate pericardial effusion and an ejection fraction of 40%. ATRA is discontinued, and dexamethasone 10 mg/12 hour and broad-spectrum antibiotics are started. The patient is transferred to the intensive care unit for respiratory support. A dramatic relief of symptoms and radiological signs is observed during the following days. ATRA is resumed when all signs and symptoms disappear. The severity of the complications that are observed lead us to ask the following questions: Is DS the only diagnosis to be considered? Should we also treat other possibilities in addition to DS? What treatment should be given? Should ATRA be withdrawn?
Diagnosis of DS should be suspected clinically in the presence of any of the following signs and symptoms: unexplained fever, weight gain, peripheral edema, dyspnea with interstitial pulmonary infiltrates, pleuropericardial effusion, hypotension, and acute renal failure. Physicians caring for patients with APL treated with ATRA and/or ATO should be aware of early signs or symptoms suggestive of DS and follow a stringent clinical monitoring plan from the start of induction therapy. Specific treatment with dexamethasone should be started promptly at the very earliest manifestation. This policy, which is addressed more extensively in the next section, is highly recommended even though none of the aforementioned signs and symptoms is pathognomonic of the syndrome, as they can be a result of other concurrent medical problems.
The initial clinical manifestations of DS can occasionally appear on the very first day of ATRA or ATO treatment. In a large series of 739 patients treated with the AIDA regimen,2 the most frequent clinical manifestations of severe DS were dyspnea (95%), pulmonary infiltrates (81%), unexplained fever (74%), weight gain of more than 5 kg (68%), pleural effusion (58%), and renal failure (46%). In a small proportion of patients (4.5%) with possible DS, a definitive diagnosis could not be made because of the presence of other complications that may have similar signs and symptoms resulting from pulmonary hemorrhage, pneumonia, cardiac toxicity, fluid overload, renal failure, and septic shock.
One of the questions raised here is whether the special attention to detect any early manifestation of DS should be restricted to the first days or be extended to the complete period of induction therapy. Around a quarter of the patients treated with AIDA in the PETHEMA study developed DS, defined as the presence of at least 2 of the signs or symptoms mentioned earlier.6 DS was similarly distributed between moderate and severe forms of the syndrome, with the latter being defined as those with at least 4 of the signs or symptoms. Interestingly, in this study, DS had a bimodal time distribution, with a first peak during the first week of treatment and a second peak during the third week (47% and 25%, respectively). In contrast, only 5% and 3% of DS cases were seen during the second week and after the fourth week, respectively. It should be noted that compared with DS occurring during the third week or beyond, early severe DS more frequently required mechanical ventilation and was associated with a higher induction death rate. This form of the syndrome was also frequently associated with a higher frequency of pulmonary infiltrates and weight gain, probably related to an initial rise of leukocyte count and fluid overload. In contrast, hypotension, unexplained fever, pericardial effusion, and renal failure were more common in late severe DS. We should emphasize that in this situation, a differential diagnosis of DS from other clinical complications, particularly sepsis but also others mentioned earlier, may be difficult. Therefore, in these cases, treatment of DS should be complemented with empirical therapy for any other suspected complication.
Although the use of distinct regimens, including variable combinations of chemotherapy ATRA and ATO and the type of prophylactic strategies, could explain the different incidence of DS reported, ranging from 2% to 27%,1,16,17,24-30 we believe that such wide range also relates to the variability of criteria used for syndrome diagnosis and grading. In this regard, the incidence of DS reported by the Gruppo Italiano Malattie EMatologiche dell'Adulto (GIMEMA) using the AIDA regimen is paradigmatic. In earlier studies,30 this group reported a low incidence of overt or “definitely present” DS of 2.5% (6/240 patients), defined as the presence of the following 5 signs and symptoms: fever, dyspnea, pleural and/or pericardial effusion, interstitial pulmonary infiltrates on chest X-ray, and unexplained weight gain greater than 5 kg. Eleven additional cases (4.6%) were classified as having “indeterminate” DS, which was defined by a combination of 2 to 4 above-mentioned signs and symptoms and/or lower extremity edema and hypotension. In the remaining patients (93%), DS was considered “definitely absent.” However, the most recent report of this group,7 using the criteria for diagnosis and grading of DS as defined by Montesinos and colleagues,6 reported a significantly higher incidence of DS in patients treated with AIDA induction, despite it being restricted to low- to intermediate-risk patients, all preventively treated with prednisone from the start of ATRA until the end of induction therapy. The randomized nature of this study, which compared conventional ATRA plus chemotherapy with ATRA plus ATO in newly diagnosed patients,7 has permitted a comparison of the incidence and severity of DS in both types of therapies in patients with WBC counts of 10 × 109/L or less. The incidence of DS was not statistically different in both groups (16% and 19% in the chemotherapy- and in the ATO-based groups, respectively), with a similar incidence of severe forms of DS (5% each). In this study, all patients received the same DS prophylaxis with prednisone (0.5 mg/kg per day) from day 1 until the end of induction therapy.
Two decades after the first description of DS, its diagnosis still relies on nonspecific clinical and radiological findings, which may also be caused by other relatively common concurrent complications. The nonspecific radiographic features of DS, usually described as pulmonary infiltrates, also can include increased cardiothoracic ratio, increased vascular pedicle width, ground glass opacity, peribronchial cuffing, septal lines, pulmonary nodules, consolidation, and pleural effusion.31 In most cases, a dramatic relief of signs and symptoms after treatment with corticosteroid will lead to a diagnosis ex juvantibus of DS. In addition, a better knowledge of prognosis and grading of DS in moderate and severe forms, according to the number of signs and symptoms, can be a useful tool for therapy decision-making in patients who develop this syndrome.
How do we treat patients with DS?
Preemptive approach
Because of the life-threatening nature of the full-blown syndrome, a preemptive use of corticosteroids at the very earliest symptom or sign suggestive of DS has been adopted as the standard management (Figure 1B).18 Dexamethasone, at a dose of 10 mg twice daily by intravenous injection, is the most common treatment. This policy is highly recommended even though none of the signs and symptoms is pathognomonic of the syndrome and can be also observed with other complications, such as bacteremia, sepsis, fungal infection, pulmonary hemorrhage, pneumonia, renal failure, and congestive heart failure.
Ruling out clinical complications mimicking DS
Additional diagnostic procedures, such as echocardiography and microbiological studies, can be of help for differential diagnosis and therapy decision-making. However, it should be noted that the presence of findings supporting a clinical picture of infection, left ventricular failure, or even pulmonary hemorrhage does not rule out a concomitant DS. For this reason, it is judicious to start empirical/preemptive treatment that covers all suspected complications, including DS.
Should ATRA and/or ATO be discontinued?
Temporary discontinuation of ATRA or ATO is indicated only in the case of DS with very poor clinical condition or severe organ dysfunction, such as patients developing renal failure or requiring admission to the intensive care unit because of respiratory distress. Otherwise, these differentiating agents could be maintained unless progression to overt syndrome or lack of response to dexamethasone is observed. If a favorable response is obtained, dexamethasone should be maintained until complete disappearance of signs and symptoms, and then ATRA or ATO should be resumed. In a few cases, a first episode of DS resolved with corticosteroids can be followed by a recurring episode.26 In such cases, dexamethasone should be resumed until resolution of the second wave of DS. It should be noted that DS is never observed beyond induction therapy, once the patient has achieved CR.
As already mentioned for DS prevention, in cases with marked hyperleukocytosis using ATO-based regimens, hydroxyurea, anthracyclines, or gemtuzumab ozogamicin are commonly given, although a potential clinical benefit of this approach is not evidence-based. However, when ATRA plus chemotherapy is used, apart from the recommendation of a very early institution of chemotherapy in patients with high WBC count, no other modification to the scheduled chemotherapy is supported by the available data and therefore not recommended.
Additional supportive measures
Other supportive measures are also crucial in the correct management of DS. In the PETHEMA protocols, furosemide is usually administered to treat signs or symptoms of fluid overload. Some cases with refractory acute renal failure and/or fluid overload may need renal replacement therapy. In patients at risk for fluid overload and high requirements of blood products to control the coagulopathy, the use of cryoprecipitate, fibrinogen, and other coagulation factor concentrates instead of fresh-frozen plasma may be considered. Invasive, but also noninvasive, mechanical ventilation is indicated in some patients with severe acute respiratory failure who do not respond to high-flow oxygen therapy. In our experience,6 diuretics, dialysis, and mechanical ventilation were needed in 87%, 12%, and 26% of patients with DS, respectively. These supportive measures were more frequently needed in patients with severe DS than in those with moderate DS. In addition, many patients will develop prerenal failure and hypotension in the context of a vascular leak syndrome. In these cases, careful fluids and/or vasopressor agents, in conjunction with empirical therapy with intravenous antibiotics, should be implemented. In general, invasive procedures for the diagnosis of pleural and pericardial effusions should be avoided. Fortunately, the vast majority of patients presenting with these and other life-threatening complications of DS have a dramatic and rapid resolution of the clinical picture when treated early with dexamethasone and the appropriate supportive measures.
Conclusions and future perspectives
Two decades after the first description of DS, its diagnosis still relies on nonspecific clinical and radiological findings, which also may be caused by other relatively common concurrent complications during induction therapy with ATRA and/or ATO in APL. Because of the sudden presentation and potential severity of the syndrome, as well as the absence of biomarkers or pathognomonic signs and symptoms, a preemptive treatment with dexamethasone (10 mg/m2 per 12 hours) is indicated. In most cases, a dramatic relief of signs and symptoms after corticosteroid therapy will lead to a diagnosis ex juvantibus of DS. However, as the clinical features of DS can be also observed with other complications, such as fluid overload, sepsis, pulmonary hemorrhage, pneumonia, renal failure, and congestive heart failure, these should be also treated if they are considered in the differential diagnosis. A better knowledge of prognosis and grading of DS in its moderate and severe forms can be a useful tool for therapy decision-making in patients who develop this syndrome. The physiopathological mechanisms of this potentially life-threatening complication are complex and still remain largely unknown. Specific biomarkers to confirm diagnosis and better evaluate outcome, as well as targeted therapies, are still not available. As to DS prophylaxis, we currently use selective DS prophylaxis with dexamethasone (2.5 mg/m2 per 12 hours intravenously for 15 days) for patients with WBC counts higher than 5 × 109/L and in those with increased serum levels of creatinine. However, the benefit provided by this and any other DS prophylaxis is still debatable. Well-designed laboratory and clinical studies are warranted to address all the above-mentioned pending issues regarding the physiopathology, diagnosis, prevention, and management of this peculiar syndrome.
Acknowledgments
The authors thank all participating institutions and clinicians in the PETHEMA studies.
This work was supported in part by Cooperative Research Thematic Network Grant RD12/0036/014 (Instituto de Salud Carlos III and European Regional Development Fund).
Authorship
Contribution: M.A.S. and P.M. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Miguel A. Sanz, Head of Hematology Department, University Hospital La Fe, Bulevar Sur S/N, 46026 Valencia, Spain; e-mail: msanz@uv.es.