Key Points
DOACs have similar efficacy as VKAs in the treatment of acute symptomatic VTE, but significantly reduce the risk of major bleeding.
The efficacy and safety of DOACs in the treatment of acute VTE are consistent in clinically important subgroups.
Abstract
In the last 4 years, 6 phase 3 trials including a total of 27 023 patients with venous thromboembolism (VTE) compared a direct oral anticoagulant (DOAC) with vitamin K antagonists (VKAs). To aid the clinician in assessing the amount of information, we address frequently raised clinical questions in a review of combined trial results. We included the phase 3 trials that compared dabigatran etexilate, rivaroxaban, apixaban, or edoxaban with VKA therapy in patients with acute symptomatic VTE. Recurrent VTE occurred in 2.0% of DOAC recipients compared with 2.2% in VKA recipients (relative risk [RR] 0.90, 95% confidence interval [CI] 0.77-1.06). Treatment with a DOAC significantly reduced the risk of major bleeding (RR 0.61, 95% CI 0.45-0.83). In parallel, intracranial bleeding, fatal bleeding, and clinically relevant nonmajor bleeding occurred significantly less in DOAC recipients. The efficacy and safety of DOACs were consistent in patients with pulmonary embolism, deep venous thrombosis, a body weight ≥100 kg, moderate renal insufficiency, an age ≥75 years, and cancer. In conclusion, DOACs and VKAs have similar efficacy in the treatment of acute symptomatic VTE, a finding that is consistent in key clinical subgroups. Treatment with a DOAC significantly reduces the risks of major bleeding.
Introduction
The treatment of venous thromboembolism (VTE) traditionally consists of initial unfractionated or low-molecular-weight heparin (LMWH) followed by vitamin K antagonists (VKAs) for at least 3 months. Recently, oral factor Xa and IIa (thrombin) inhibitors, collectively termed direct oral anticoagulants (DOACs), have proven to be an effective and safe alternative. DOACs offer significant simplification of long-term anticoagulation because these drugs, unlike VKAs, do not require frequent laboratory monitoring and subsequent dose adjustments. Between 2009 and 2013, 4 different compounds were compared with conventional therapy for the treatment of acute VTE. In total, 27 023 patients were enrolled in 6 phase 3 randomized controlled trials.1-6 Rivaroxaban has been approved for VTE treatment in most countries and approval for apixaban, dabigatran etexilate (hereafter, dabigatran), and edoxaban is expected soon.
Clinicians will need to choose between these new anticoagulants and standard treatment, and they will need clinically relevant information as to whether these agents are indeed suited for all of their patients with VTE. To aid the clinician in dealing with the overwhelming amount of information, we present a review of the combined results of the phase 3 trials and address various frequently raised clinical questions:
What is the overall efficacy of DOACs compared with VKAs on recurrent VTE?
What is the safety profile of DOACs compared with VKAs in terms of major bleeding, intracranial bleeding, major gastrointestinal bleeding, and clinically relevant nonmajor (CRNM) bleeding?
What is the efficacy and safety of DOACs compared with VKAs in specific subgroups (ie, patients with pulmonary embolism [PE], patients with deep venous thrombosis [DVT], patients with cancer, elderly patients, obese patients, and patients with impaired renal function)?
What is the net clinical benefit in terms of patient-relevant outcomes (ie, prevention of recurrence with minimal risk of major bleeding) of DOACs compared with VKAs?
Methods
Study selection and data collection
We performed a meta-analysis of phase 3 randomized controlled trials comparing DOACs with VKAs for treatment of acute symptomatic DVT, PE, or both. Six studies were included, evaluating the direct thrombin inhibitor dabigatran (RE-COVER and RE-COVER II studies1,2 ), and the factor Xa inhibitors rivaroxaban (EINSTEIN-DVT and EINSTEIN-PE studies5,6 ), apixaban (AMPLIFY study4 ), and edoxaban (Hokusai-VTE study3 ). Phase 2 dose-finding studies and studies evaluating extended anticoagulant treatment after the initial treatment period were excluded. Studies on the thrombin inhibitor ximelagatran were also excluded because this agent is unavailable for patient use.
Two authors independently extracted information about the following outcomes from the main trial publications and supplemental data: symptomatic recurrent VTE or VTE-related death, major bleeding, intracranial bleeding, fatal bleeding, major gastrointestinal bleeding, CRNM bleeding, all-cause mortality, and net clinical benefit defined as the composite of first occurrence of symptomatic recurrent VTE, VTE-related death, or major bleeding. The definitions of recurrent VTE and bleeding were similar across all included studies and in accordance with the criteria proposed by the International Society on Thrombosis and Haemostasis.7 Therein, major bleeding was defined as fatal bleeding, bleeding in a critical area or organ, or bleeding causing a fall in hemoglobin of 2 mg/dL (or 1.24 mmol/L). CRNM bleeding was defined as overt bleeding not meeting the criteria for major bleeding but associated with a medical intervention, an unscheduled contact with a physician, (temporary) cessation of study treatment, or being associated with discomfort for the patient such as pain, or impairment of activities of daily life.
We performed additional analyses for subgroups of patients with symptomatic PE with or without concomitant DVT, DVT of the leg only, cancer at baseline, age ≥75 years, creatinine clearance of 30 to 49 mL per minute, and body weight ≥100 kg. Furthermore, we performed a sensitivity analysis of studies evaluating a factor Xa inhibitor only (ie, AMPLIFY, EINSTEIN-DVT, EINSTEIN-PE, and Hokusai-VTE).
When data could not be retrieved from the trial publications, we approached the corresponding authors and sponsors for additional information.
Statistical analysis
Analyses were performed with data as provided by the trial publications in which the intention-to-treat population was used for efficacy outcomes and the safety population for bleeding outcomes. We calculated relative risk (RR) and corresponding 95% confidence interval (CI) for each outcome. Outcomes across the studies were combined using the Mantel-Haenszel method and compared with the DerSimonian and Laird random-effects model. We assessed and quantified statistical heterogeneity across the studies using the Cochran Q statistic and I2 test. All analyses were performed with Review Manager, version 5.2 (Copenhagen, The Nordic Cochrane Centre, The Cochrane Collaboration, 2012).
Results
Characteristics
Overall, 13 512 patients were randomized to a DOAC and 13 511 patients to a VKA with a target international normalized ratio (INR) of 2.0 to 3.0. Patient characteristics and study details are shown in Table 1. The overall mean age of patients was 56 years and 57% were men. Risk factors for recurrent VTE were evenly distributed. The index event was DVT of the leg in 57% of patients and PE with or without concomitant DVT in 43%. The majority of patients (72%) received anticoagulant treatment of 6 months. The overall time in the therapeutic INR range (TTR) in patients on VKAs ranged from 57% to 64% in the studies. Patients and physicians were blinded for treatment allocation, except for both EINSTEIN studies, which had an open-label design. All suspected outcomes were adjudicated by the same blinded, independent central adjudication committee in all studies. In the RE-COVER, RE-COVER II, and Hokusai-VTE studies, dabigatran and edoxaban were started after an initial course of parenteral anticoagulants for a minimum of 5 days. Rivaroxaban (EINSTEIN studies) and apixaban (AMPLIFY) were given as monotherapy during the entire treatment period with a higher dose in the first 3 weeks. In EINSTEIN-DVT, EINSTEIN-PE, and Hokusai-VTE, patients were treated for 3, 6, or 12 months as determined by the treating physician, whereas the treatment duration was six months in the other studies (Table 1).
Overall efficacy
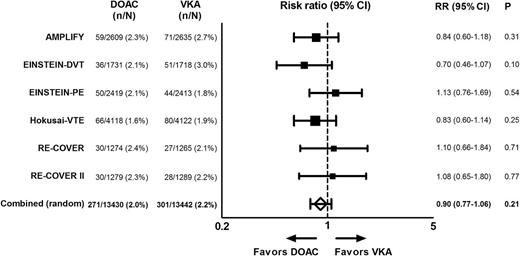
In total, 26 872 patients were included in the efficacy analysis. Recurrent VTE, including VTE-related death, occurred in 271 of 13 430 (2.0%) patients randomized to a DOAC vs 301 of 13 442 (2.2%) patients randomized to a VKA (RR 0.90, 95% CI 0.77-1.06; Figure 1). This is in line with the findings of the individual studies in which DOACs were consistently shown to be noninferior to VKAs. There was no evidence for heterogeneity (I2 = 0%).
First recurrent VTE or VTE-related death. For Hokusai-VTE, we used event data for the on-treatment period. Heterogeneity: I2 = 0%; P = .53.
First recurrent VTE or VTE-related death. For Hokusai-VTE, we used event data for the on-treatment period. Heterogeneity: I2 = 0%; P = .53.
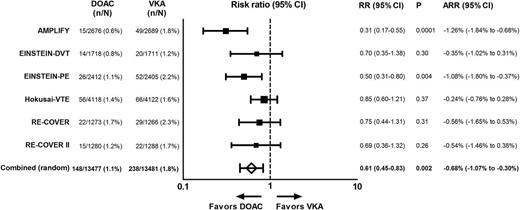
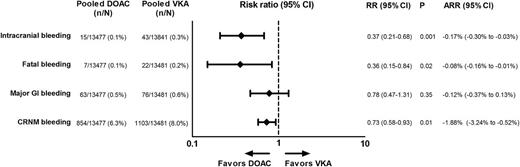
Overall bleeding
In total, 26 958 patients were included in the safety analysis. Treatment with a DOAC was associated with a 39% relative reduction in major bleeding (RR 0.61, 95% CI 0.45-0.83; Figure 2). In parallel, intracranial bleeding and fatal bleeding occurred significantly less in patients in the DOAC group (RR 0.37 [95% CI 0.21-0.68] and RR 0.36 [95% CI 0.15-0.84], respectively; Figure 3). In this VTE setting, DOACs were associated with a 22% nonsignificant relative reduction in major gastrointestinal bleeding (RR 0.78, 95% CI 0.47-1.31) and a relative reduction of 27% in CRNM bleeding (RR 0.73, 95% CI 0.58-0.93; Figure 3). Heterogeneity was substantial in the analyses of major bleeding, major gastrointestinal bleeding, and CRNM bleeding (I2 = 51% to 85%). Forest plots with individual study data are provided in the supplemental data.
Major bleeding. The sums of numbers of events from RE-COVER and RE-COVER II with respect to major bleeding slightly differ from those in the pooled analysis. We used data from the pooled analysis because these were most accurate. Heterogeneity: I2 = 51%, P = .07. ARR, absolute risk reduction.
Major bleeding. The sums of numbers of events from RE-COVER and RE-COVER II with respect to major bleeding slightly differ from those in the pooled analysis. We used data from the pooled analysis because these were most accurate. Heterogeneity: I2 = 51%, P = .07. ARR, absolute risk reduction.
Intracranial, major gastrointestinal, fatal, and clinically relevant nonmajor bleeding. Intracranial bleeding numbers comprise fatal and nonfatal events. Because CRNM bleeding was not a predefined outcome on its own in both RE-COVER studies, we obtained these numbers by subtracting major bleeding numbers from the composite of major and CRNM bleeding. Heterogeneity: intracranial bleeding I2 = 0%, P = .66; major GI bleeding I2 = 51%, P = .07; fatal bleeding I2 = 0%, P = .86; CRNM bleeding I2 = 85%, P < .00001. GI, gastrointestinal.
Intracranial, major gastrointestinal, fatal, and clinically relevant nonmajor bleeding. Intracranial bleeding numbers comprise fatal and nonfatal events. Because CRNM bleeding was not a predefined outcome on its own in both RE-COVER studies, we obtained these numbers by subtracting major bleeding numbers from the composite of major and CRNM bleeding. Heterogeneity: intracranial bleeding I2 = 0%, P = .66; major GI bleeding I2 = 51%, P = .07; fatal bleeding I2 = 0%, P = .86; CRNM bleeding I2 = 85%, P < .00001. GI, gastrointestinal.
Patient-relevant outcomes
Net clinical benefit, defined as the composite of a first episode of a patient-relevant outcome (ie, recurrent VTE, VTE-related death, or major bleeding) occurred in 424 of 13 430 (3.2%) DOAC recipients and in 537 of 13 442 (4.0%) patients treated with VKAs (RR 0.79, 95% CI 0.70-0.90). The all-cause mortality rate was similar in both groups (RR 0.98, 95% CI 0.84-1.14). There was no evidence for heterogeneity in the patient-relevant outcome analyses (I2 = 0%).
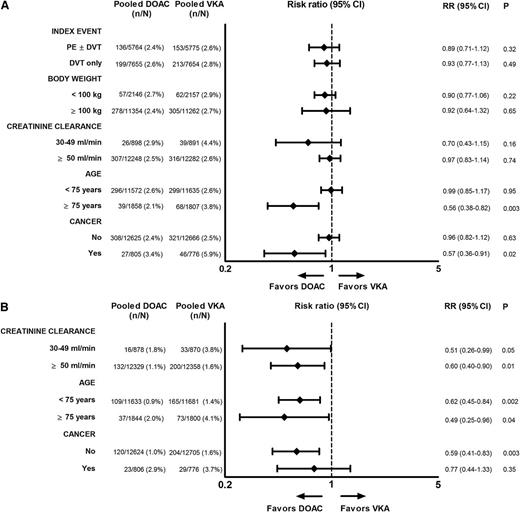
Subgroups
The efficacy of DOACs was consistent across the subgroups of patients with PE, patients with DVT only, patients with a body weight ≥100 kg, and patients with moderately impaired renal function (creatinine clearance 30-49 mL per minute) (Figure 4A). In elderly patients (age ≥75 years) and patients with cancer, we observed significantly less recurrent VTE in the DOAC group than in the VKA group (RR 0.56 [95% CI 0.38-0.82] and RR 0.57 [95% CI 0.36-0.91], respectively; Figure 4A).
First recurrent VTE or VTE-related death in specific subgroups. (A) For Hokusai-VTE, we used event data for the overall study period.3 The group of patients with impaired renal function includes 28 DOAC recipients and 32 VKA recipients with a creatinine clearance <30 mL per minute (protocol violations). Heterogeneity patients with an index PE I2 = 0%, P = .65; patients with an index DVT I2 = 0%, P = .41; patients with a body weight <100 kg I2 = 3%, P = .40; patients with a body weight ≥100 kg I2 = 0%, P = .71; patients with a creatinine clearance 30 to 49 mL per minute I2 = 0%, P = .61; patients with a creatinine clearance ≥50 mL per minute I2 = 0%, P = .59; patients <75 years of age I2 = 0%, P = .71; patients ≥75 years of age I2 = 0%, P = .95; patients without cancer I2 = 0%, P = .57; and patients with cancer I2 = 0%, P = .99. (B) Major bleeding in specific subgroups. For the subgroup analyses of patients >75 years of age and patients with a creatinine clearance of 30 to 49 mL per minute, we used the pooled RE-COVER data from the double-dummy period only. For Hokusai-VTE, we used event data for the overall study period.3 The group of patients with impaired renal function includes 28 DOAC recipients and 32 VKA recipients with a creatinine clearance <30 mL per minute (protocol violations). Heterogeneity patients with a creatinine clearance 30 to 49 mL per minute I2 = 11%, P = .35; patients with a creatinine clearance ≥50 mL per minute I2 = 63%, P = .03; patients <75 years of I2 = 28%, P = .24; patients ≥75 years of age I2 = 60%, P = .04; patients without cancer I2 = 54%, P = .06; patients with cancer I2 = 0%, P = .73.
First recurrent VTE or VTE-related death in specific subgroups. (A) For Hokusai-VTE, we used event data for the overall study period.3 The group of patients with impaired renal function includes 28 DOAC recipients and 32 VKA recipients with a creatinine clearance <30 mL per minute (protocol violations). Heterogeneity patients with an index PE I2 = 0%, P = .65; patients with an index DVT I2 = 0%, P = .41; patients with a body weight <100 kg I2 = 3%, P = .40; patients with a body weight ≥100 kg I2 = 0%, P = .71; patients with a creatinine clearance 30 to 49 mL per minute I2 = 0%, P = .61; patients with a creatinine clearance ≥50 mL per minute I2 = 0%, P = .59; patients <75 years of age I2 = 0%, P = .71; patients ≥75 years of age I2 = 0%, P = .95; patients without cancer I2 = 0%, P = .57; and patients with cancer I2 = 0%, P = .99. (B) Major bleeding in specific subgroups. For the subgroup analyses of patients >75 years of age and patients with a creatinine clearance of 30 to 49 mL per minute, we used the pooled RE-COVER data from the double-dummy period only. For Hokusai-VTE, we used event data for the overall study period.3 The group of patients with impaired renal function includes 28 DOAC recipients and 32 VKA recipients with a creatinine clearance <30 mL per minute (protocol violations). Heterogeneity patients with a creatinine clearance 30 to 49 mL per minute I2 = 11%, P = .35; patients with a creatinine clearance ≥50 mL per minute I2 = 63%, P = .03; patients <75 years of I2 = 28%, P = .24; patients ≥75 years of age I2 = 60%, P = .04; patients without cancer I2 = 54%, P = .06; patients with cancer I2 = 0%, P = .73.
The significant reduction in major bleeding associated with DOAC treatment was maintained in patients with a creatinine clearance 30 to 49 mL per minute and in patients ≥75 years (RR 0.51 [95% CI 0.26-0.99] and RR 0.49 [95% CI 0.25-0.96], respectively; Figure 4B). In cancer patients, we observed no difference in the risk of major bleeding (RR 0.77, 95% CI 0.44-1.33; Figure 4B). The absolute major bleeding rate in the DOAC and VKA groups was considerable in patients with impaired renal function, elderly patients, and cancer patients, indicating a higher bleeding risk in these subgroups. There was no evidence for heterogeneity in the subgroup analyses for efficacy (I2 = 0%). For major bleeding, heterogeneity was substantial in the subgroup analysis of elderly patients (I2 = 60%). Forest plots with individual study data are provided in the supplemental data.
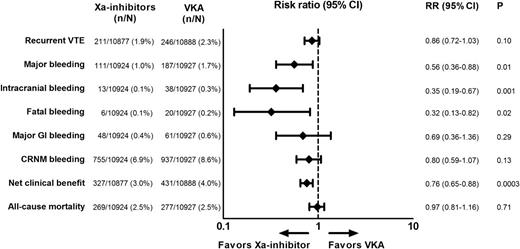
Factor Xa inhibitors only
In the sensitivity analysis of the 4 studies evaluating a factor Xa inhibitor, factor Xa inhibitors were as effective as VKAs in the prevention of recurrent VTE, with a significant relative reduction of 44% in major bleeding (RR 0.56, 95% CI 0.36-0.88; Figure 5). Point estimates for intracranial bleeding, major gastrointestinal bleeding, fatal bleeding, CRNM bleeding, net clinical benefit, and all-cause mortality were comparable with the overall analysis, although the benefit in CRNM bleeding did not reach statistical significance.
Efficacy and safety of factor Xa inhibitors. Heterogeneity overall I2 = 0%, P = .43; major bleeding I2 = 69%, P = .02; intracranial bleeding I2 = 0%, P = .60; major gastrointestinal bleeding I2 = 62%, P = .05; fatal bleeding I2 = 0%, P = .72; CRNM bleeding I2 = 89%, P = .13; net clinical benefit I2 = 11%, P = .34; all-cause mortality I2 = 10%, P = .34. Xa-inhibitor, oral direct factor Xa inhibitor.
Efficacy and safety of factor Xa inhibitors. Heterogeneity overall I2 = 0%, P = .43; major bleeding I2 = 69%, P = .02; intracranial bleeding I2 = 0%, P = .60; major gastrointestinal bleeding I2 = 62%, P = .05; fatal bleeding I2 = 0%, P = .72; CRNM bleeding I2 = 89%, P = .13; net clinical benefit I2 = 11%, P = .34; all-cause mortality I2 = 10%, P = .34. Xa-inhibitor, oral direct factor Xa inhibitor.
Discussion
The present clinical review of all phase 3 trials reveals that DOACs are clearly noninferior to VKA therapy with respect to overall efficacy in the treatment of acute symptomatic VTE. This effect is consistent in patients with PE, DVT, body weight ≥100 kg, and moderate renal insufficiency. An interesting observation is a possibly better efficacy of DOACs vs VKAs in elderly patients and cancer patients. It should be realized that the regimen of LMWH followed by VKAs is very effective with a relative reduction in recurrent VTE of 80% to 90% compared with no or inadequate treatment.8,9 As a consequence, all phase 3 trials were designed as noninferior studies for efficacy. Taken together, the observed comparable efficacy of DOACs should reassure the clinician that these agents are effective in all subgroups analyzed.
The most striking finding is the significant almost 40% relative reduction in major bleeding. Consistent with this observation are the reductions in important components of major bleeding, such as fatal bleeding (64% relative reduction) and intracranial bleeding (63% relative reduction). Although rare, they are the most feared complications of anticoagulant treatment. In line with these reductions, DOAC recipients have significantly less CRNM bleeding, and there are no indications that the risk of major gastrointestinal bleeding is increased in this setting of VTE. The benefit of DOACs with respect to major bleeding was maintained in patients with moderate renal insufficiency and elderly patients, whereas in cancer patients the risk of major bleeding was at least comparable with that in the standard treatment group, and possibly better. Taken together, our results indicate that DOACs can be prescribed safely for patients with VTE.
Our findings with respect to major bleeding are very similar to the results seen in the atrial fibrillation (AF) trials, where DOACs reduced intracranial hemorrhage by a significant 52% compared with VKAs.10 In contrast, DOACs were associated with a significant 25% relative increase in major gastrointestinal bleeding in the AF trials, whereas in the treatment of VTE, no difference in major gastrointestinal bleeding rates was seen.10 The reasons for this discrepancy are at present unclear but may include differences in patient characteristics (eg, use of concomitant antiplatelet drugs) and treatment duration.
The aforementioned conclusions are strengthened by the superiority of DOACs with respect to the composite measurement of patient-relevant outcomes (ie, recurrent VTE, VTE-related death, and major bleeding). Based on the sensitivity analysis of factor Xa inhibitors and the previously published pooled analysis of the thrombin inhibitor dabigatran, efficacy and safety are maintained across the 2 drug classes.2
Other meta-analyses of acute VTE trials have been published previously.11,12 Although the overall conclusions are similar, the present analysis includes all phase 3 data and additionally provides the treating physician with important safety and efficacy information for clinically relevant and frequently encountered subgroups. Furthermore, as a result of the larger number of patients included, the point estimates and the confidence intervals are more robust both for conclusions regarding noninferiority and superiority.
Our study has potential limitations. By combining the results of 6 trials, we presume that all DOACs are the same, but they are not. We have pooled data of 2 different compounds and the included studies were different in follow-up durations and treatment regimens. Three studies used initial heparin, but the need for this, particularly in clinically significant thrombosis, remains to be determined. Nevertheless, most combined results were quite homogeneous, hence it seems that the similarities between these compounds are larger than the differences. This is further supported by the results of the analyses of factor Xa inhibitors only. Of note, the observed heterogeneity for major gastrointestinal and CRNM bleeding was statistically significant across the studies at an α level of .10. Potential explanations, apart from differences between drugs, include variability in patient characteristics and study design.
Treatment with a DOAC has clear practical advantages over treatment with a VKA. Frequent treatment monitoring and individualized dose adjustments, as is usual in VKA treatment, are no longer required. Moreover, apixaban and rivaroxaban can be given as oral monotherapy without the need for cumbersome daily injections with LMWH or continuous infusion of unfractionated heparin during the initial phase. A potential downside is that patient adherence to DOACs may be worse than adherence to VKAs because of the absence of regular contact with anticoagulation clinics. Sometimes, missing a dose may lead to subtherapeutic drug levels more quickly because of the shorter half-life of DOACs. Nevertheless, it is impossible to predict how this will affect the relative efficacy and safety of DOACs vs VKAs in the real world, because the quality of INR control of VKA therapy is also lower in real-world patients compared with patients enrolled in randomized trials.13 Other concerns include the lack of a specific reversal agent for DOACs and the lack of DOAC-specific laboratory assays in most hospitals, complicating the management of DOAC-related bleeding episodes. This has to be balanced against the significant numerical reduction in major and CRNM bleeding associated with treatment with DOACs. Furthermore, emerging evidence suggests that major bleeding on DOACs tends to have a less severe presentation and take a less severe clinical course than VKA-related bleeding.14
The uptake of DOACs for treatment of acute VTE in clinical practice will also depend on regulatory and reimbursement approval. Some concerns have been raised that relatively high numbers needed to treat will not justify more costly drugs for a relatively short duration.12 However, this is not in line with the recent analyses of the financial consequences of VTE treatment with rivaroxaban presented by the British National Institute for Health Care and Excellence.15,16 They conclude that rivaroxaban represents a clinical and cost-effective option for treatment of DVT or PE for all treatment durations, and even dominates LMWH and VKA therapy in the 3-month treatment group. It is likely that with the more robust findings in efficacy and safety in the present analysis, the cost-effectiveness conclusions will be reinforced for this group of drugs.
Now that the clinical development programs of all DOACs for the treatment of acute VTE have been completed, several relevant questions are left unanswered. Postmarketing registries will need to assess whether the favorable trial results also apply to “real-world” patients that have more comorbidities and more co-medication and are less adherent than a standard trial population. Patients with severe renal impairment (creatinine clearance <30 mL per minute) were excluded from the trials, hence the results do not apply to this group of patients. Furthermore, the optimal therapy of VTE in cancer patients is uncertain. LMWH monotherapy is suggested over VKAs according to current clinical guidelines because of a better efficacy.8 DOACs could become an attractive alternative to daily LMWH injections for patients with active cancer, who frequently require indefinite anticoagulant treatment. However, it should be realized that patients with a life expectancy of less than the duration of the trial were excluded from the DOAC trials, as were patients for whom long-term treatment with LMWH was anticipated. Still, our results in the subgroup of cancer patients indicate a possibly better efficacy of DOACs over VKAs without increasing the risk of major bleeding, which is in line with the findings of trials comparing LMWH with VKAs. Direct comparisons of DOACs vs LMWH in randomized controlled trials are urgently needed to address the efficacy and safety of DOACs in cancer patients.
In conclusion, DOACs and VKAs have similar efficacy in the treatment of acute symptomatic deep venous thrombosis and pulmonary embolism, a finding that is consistent in key clinical subgroups. Treatment with a DOAC is associated with a significant reduction in the risk of major bleeding, intracranial bleeding, and fatal and clinically relevant nonmajor bleeding.
The online version of this article contains a data supplement.
There is an Inside Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: All authors made a substantial contribution to the concept and design of the study, interpreted the data, and reviewed the manuscript; N.v.E. and M.C. performed the data extraction; N.v.E. performed the analyses; N.v.E. and M.C. drafted the paper; and S.S., S.M., and H.R.B. critically revised the paper for important intellectual content.
Conflict-of-interest disclosure: M.C. received research support, lecturing, and consultancy fees from Boehringer Ingelheim, Bayer, Daiichi-Sankyo, and Bristol-Myers Squibb. S.S. received honoraria from Boehringer Ingelheim. S.M. received consulting fees from Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb/Pfizer, GlaxoSmithKline, and Daiichi-Sankyo, and research support from Bayer, Bristol-Meyers Squibb/Pfizer, GlaxoSmithKline, and Sanquin. H.R.B. has received consulting fees and research support from Bayer, Bristol-Meyers Squibb, Daiichi-Sankyo, GlaxoSmithKline, Isis, Pfizer, Roche, Sanofi-Aventis, and ThromboGenics. The remaining author declares no competing financial interests.
Correspondence: Nick van Es, Academic Medical Center, Department of Vascular Medicine Room F4-139, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands; e-mail: n.vanes@amc.nl.