In this issue of Blood, Bhatia et al demonstrate the critical importance of an adherence to oral chemotherapy regimens in attaining cure for children with acute lymphoblastic leukemia (ALL) and identify race-specific determinants of adherence.1
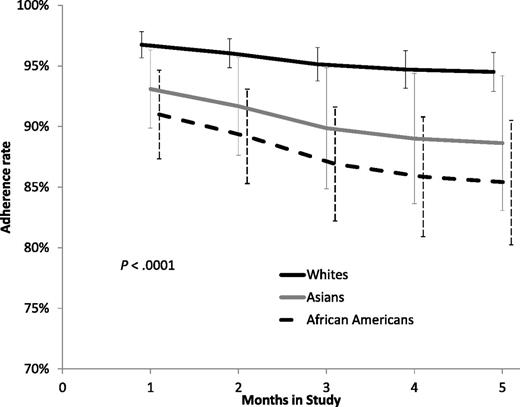
Adherence over time to 6-MP delivery among white, Asian-American, and African-American populations. See Figure 1B in the article by Bhatia et al that begins on page 2345.
Adherence over time to 6-MP delivery among white, Asian-American, and African-American populations. See Figure 1B in the article by Bhatia et al that begins on page 2345.
Since 1970, the cure rate for children with ALL has increased dramatically from <30% to ∼80%. This remarkable improvement reflects intense study of leukemia biology and carefully orchestrated clinical trials that have (1) defined the need for presymptomatic treatment of the central nervous system in addition to systemic chemotherapy; (2) delineated effective applications of standard chemotherapeutic agents; and (3) allowed for the establishment of a robust risk classification schema that modulates the intensity of therapy to the predicted risk of relapse, leading to moderation of toxicity for some while enhancing the overall likelihood of cure. Now, an increasing understanding of clinically relevant gene mutations and the pathways they impact offers the opportunity to further enhance risk classification and to develop targeted therapies. Bhatia et al now illuminate another critical element in achieving cure: taking your medicine.
Hunger et al2 recently studied survival among patients with ALL, diagnosed in successive 5-year blocks, and found that survival improved for all subgroups, except infants, from 1990 to 2005. The discrepancy in absolute survival between black and white patients (Asian Americans were not identified as a cohort) decreased from 11% in 1990 to 1994 to 3.3% in 2000 to 2005. This discrepancy is, in part, attributable to a higher incidence of high-risk features among black children and adolescents, but the work of Bhatia et al indicates that significant differences in adherence to oral 6-mercaptopurine (6-MP) may also play a role.1,3 Using a medication event monitoring system to measure adherence, they were able to analyze data for 39 803 person-days in 295 patients. Adherence to 6-MP decreased from the end of month 1 to the end of month 5 for the entire cohort, from 95% to 91.8%, but adherence rates among Asian Americans and African Americans were significantly less than those of non-Hispanic whites at 90.0 ± 4.9 and 87.1 ± 4.4% compared with 95.2 + 1.3% (see figure). An adherence rate <90% was associated with a 3.9-fold increase in the risk of relapse, and using this 90% cutoff, 44% of African Americans and 15% of Asian Americans were nonadherent compared with 13% of non-Hispanic whites (P < .0001). Furthermore, 33% of relapses were attributable to nonadherence. Male gender and low maternal education were associated with poor adherence among African Americans, whereas low-income households were linked to poor adherence in Asian Americans. When adherence was assessed in Asian-American and African-American patients from households with higher incomes and maternal education where mothers were full-time caregivers, rates of adherence were comparable to those of non-Hispanic whites.
The findings of Bhatia et al are consistent with those described by the American Academy of Pediatrics Task Force on the Family in 2003.4 They detail the powerful impact of family well-being on child health and developmental outcomes. Complex living arrangements resulting in loss of stability were linked to poorer health outcomes in children as was chaos in daily living (noise, crowding, and a lack of sustained household routines) and parental psychopathology. Clearly, these factors, compounded by the stressors associated with the diagnosis of cancer in a child, may preclude the establishment of a routine conducive to regimented adherence to oral chemotherapy regimens. Fiese et al,5 in Pediatrics, provided guidelines for pediatricians, urging them to use them to identify the aspects of family structure and function that may impact a child’s health. They also provide a review of educational approaches to promote healthy behaviors that have been of value in noncancer populations. Bhatia et al provide pediatric oncologists with clear guidelines as to the level of adherence that must be achieved to optimize the chance of cure and insight into the factors associated with poor adherence. Like Fiese et al, they are also seeking an approach to support family function and improve adherence. Specifically, this team is currently evaluating the feasibility, utility, and efficacy of an interactive patient education program coupled with a web-based medication scheduling and text-messaging reminder system that uses cell phones to remind parents to give the 6-MP.6
Remember that despite the ability to identify subsets of patients with ALL at extremely high risk of relapse based on blast cell genetics and/or measures of response,7 the majority of deaths in children and adolescents with ALL actually occur among those with good-risk clinical features, because those with a favorable prognosis represent the majority of pediatric patients with ALL.2 It is conceivable then that many of these better-risk patients have chemotherapy-responsive disease and with adequate adherence will be cured. It may take a village to ensure adequate adherence among all patients with ALL, but the benefit will be significant, and it might be achievable with relatively low-cost interventions.
Conflict-of-interest disclosure: The author declares no competing financial interests.