Abstract
Introduction
17p-/TP53-mutated CLL (17p- CLL) represents approximately 5 to 10% of newly diagnosed CLL cases. Patients with this abnormality have a poor prognosis after chemo-immunotherapy. According to current guidelines, allogeneic hematopoietic cell transplantation (HCT) is recommended in 17p- CLL cases as part of the first- or second-line treatment. In 2010, the European Society for Blood and Marrow Transplantation (EBMT) and the European Research Initiative on CLL (ERIC) started a non-interventional study, to evaluate the outcome of allogeneic HCT in 17p-CLL. Here we report first results from this study.
Patients & Methods
Major eligibility criteria were 17p- CLL in complete or partial remission after first-line therapy or treatment of relapse, age below 70 years, availability of an HLA-compatible related or unrelated donor with up to one HLA-mismatch at HLA-A, -B, -C or DRB1. The primary objective was to determine relapse-free survival.
Results
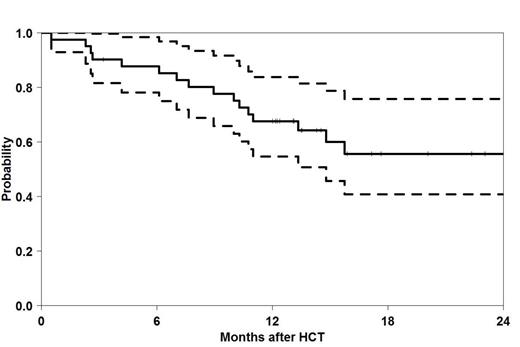
Forty-one patients (30 males, 11 females) from eleven transplant centres were registered for this study between June 2010 and September 2012. The median age was 59 years (range, 28 to 70 years). Twelve patients (29%) were transplanted in first remission. The median number of pre-treatments was 2 (range, 1 to 7) and included alemtuzumab in 31 patients (76%). The remission status at HCT was reported as partial remission in 31 patients (76%) and as complete remission in 10 patients (24%). The median time between diagnosis and HCT was 35 months (range, 4 to 229 months) and the median time between first treatment of CLL and HCT was 12 months (range, 2 to 227 months). Myeloablative conditioning was administered in 3 patients (7%), fludarabine-based reduced-intensity conditioning in 25 patients (61%) and non-myeloablative conditioning, based on 2 Gray TBI, in 13 patients (32%). Donors were HLA-identical siblings for 11 patients (27%), well-matched HLA-compatible unrelated donors for 25 patients (61%) and partially matched unrelated donors for 5 patients (12%). Thirteen patients received ATG. Fifteen patients experienced grade II to IV graft-versus host disease. By July 2014, 27 patients were alive and 14 patients had died. From the deceased patients, 4 patients died subsequent to relapse and 10 patients died without relapse. Causes of death were GVHD in 7 patients, infection in one patient and other causes in 2 patients. The median observation time for living patients was 16 months (range, 3 to 36 months). The probability of relapse-free survival (see also Figure 1) and overall survival at 2 years was 56% (95% CI, 42% to 74%) and 67% (95% CI, 51% to 83%). At two years the cumulative incidences of relapse and non-relapse mortality were 20% (95% CI, 6% to 34%) and 24% (95% CI, 10% to 39%).
Conclusions
When considering the high disease-specific risk and the median age of 59 years at transplantation of this cohort of patients, we present favourable early results after allogeneic HCT for patients with 17p- CLL. Non-relapse mortality, mainly caused by GVHD, compromised relapse-free survival. The data suggests that allogeneic HCT remains an attractive treatment option, especially for patients with a low transplant risk and a high disease-specific risk of mortality. These results may serve as benchmark for new drugs which are currently under clinical development or have recently received approval for this indication.
Relapse-free Survival in 41 patients with del(17p) CLL after HCT
Relapse-free Survival in 41 patients with del(17p) CLL after HCT
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.