Abstract
Introduction:
Pre-transplant remission status in patients with acute myeloid leukemia (AML) is one of the most important factors determining their outcomes after allogeneic hematopoietic cell transplantation (allo-HCT). Patients not in remission prior to undergoing allo-HCT continue to have a very poor prognosis. Complete remission with incomplete cell count recovery (CRi) following chemotherapy for acute myeloid leukemia (AML) has also been associated with reduced overall survival and increased risk of relapse. However, there is currently a paucity of data on transplant outcomes in AML patients with ablated marrows after prior chemotherapy. In these patients, waiting for count recovery for an extended time period leads to increased infectious complications, often making them ineligible for allo-HCT. We hypothesized that outcomes of AML patients with pre-transplant ablated marrows who undergo allo-HCT would be similar to those of patients who are in complete remission (CR) prior to allo-HCT. To answer this question, we retrospectively analyzed the outcomes of AML patients from a single institution who underwent allo-HCT in CR, CRi, or with an ablated marrow.
Patient and methods:
For this retrospective study, we analyzed the outcomes of 270 AML patients (median age 54 years, range 17 to 74 years, 146 males and 124 females) who underwent 6/6 HLA-matched sibling or 10/10 HLA-matched unrelated donor transplantation at Washington University School of Medicine in St. Louis between 2006 and 2013. Patients with persistent disease based on bone marrow biopsy immediately prior to transplant were excluded. Data was collected on baseline characteristics including patient and donor sex, AML type, induction therapy, conditioning regimen, stem cell source, and graft-versus-host disease (GVHD) prophylaxis. Based on their cell count and marrow recovery prior to allo-HCT, patients were divided into 3 categories: CR, CRi, and ablated marrow, using response criteria from the International Working Group. The primary outcomes were overall survival (OS) and disease-free survival (DFS), and the secondary outcomes were cumulative incidence of non-relapse mortality (NRM), cumulative incidence of relapse, acute graft vs. host disease (aGVHD), and chronic graft vs. host disease (cGVHD). Propensity-score matching was used to adjust for potential confounding effects of patient characteristics, and the between-group differences in OS or DFS were compared by Cox proportional hazards model.
Results:
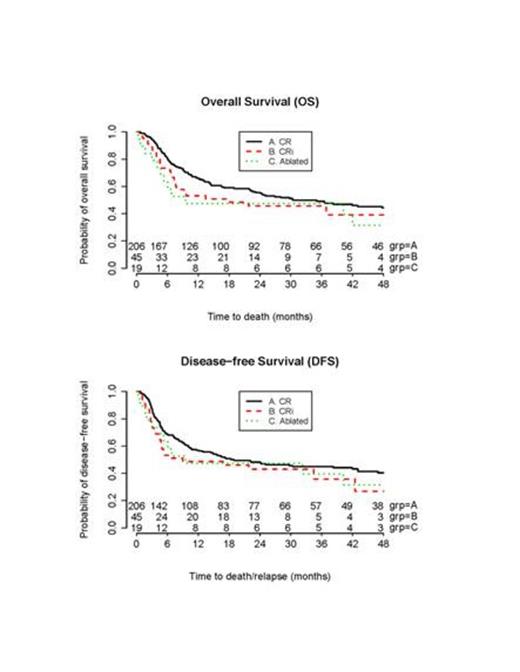
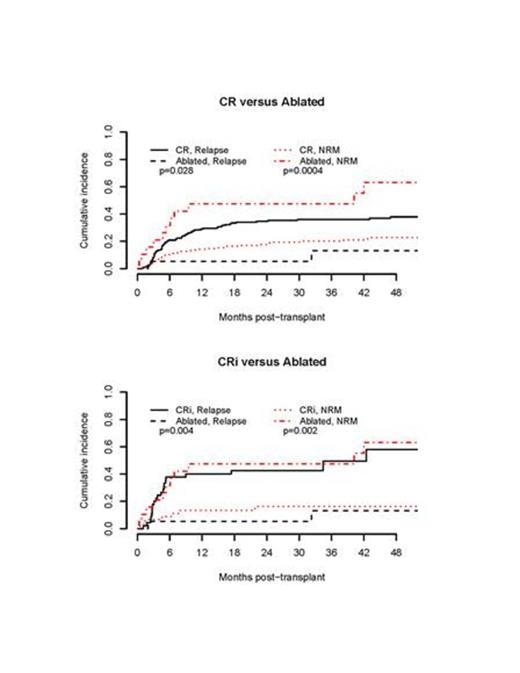
Of the 270 patients, 206 were in CR, 45 in CRi, and 19 had ablated marrow prior to their allo-HCT. Median follow-up for the CR, CRi, and ablated groups were 524, 410, and 290 days, respectively. The patients with ablated marrows had a 3-year OS of 47% and DFS of 40%, as compared to patients in CR whose 3-year OS and DFS were 49% and 45%, respectively (Fig. 1). Using a 1:3 propensity-score matching (3 CR per 1 ablated), no significant differences were found in OS (HR=1.66, 95% CI 0.88-3.12; P = 0.12) or DFS (HR=1.39, 95% CI 0.75 - 2.58; P = 0.30). The cumulative incidence of NRM in our ablated marrow cohort was 58%, significantly higher than those in CR and CRi who had cumulative incidences of NRM of 22% (P = 0.0004) and 16% (P = 0.002), respectively (Fig. 2). The cumulative incidence of grade 2-4 aGVHD in patients with CR, CRi, and ablated marrow, were 38%, 38%, and 42%, respectively (P = 0.93). Likewise, the cumulative incidence of cGVHD in patients with CR, CRi, and ablated marrow, were 34%, 38%, and 16%, respectively (P = 0.22).
Conclusions:
Allo-HCT continues to be the curative therapy for patients with AML. Based on our results, overall survival and disease-free survival following transplant for patients with ablated marrows do not differ significantly from those in CR or CRi. Interestingly, there was a higher incidence of non-relapse mortality among patient with ablated marrows compared to those in Cr or CRi, which is most likely related to the use of myeloablative conditioning regimen in our ablated patients. These results could have an important bearing on patients with ablated marrows whom treating physicians might post-pone allo-HCT to wait for marrow recovery, thereby potentially putting them at increased risk for infectious and bleeding complications. Smaller cohort size is the major limitation of our study, and our results suggest investigating this important question in a large registry.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.