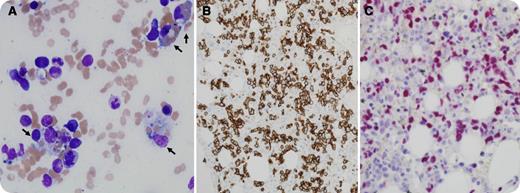
A 46-year-old man with HIV was admitted with subacute onset of fever, cough, generalized weakness, and weight loss. He went on to develop multiorgan failure with encephalopathy, acute kidney injury, fulminant liver failure, and disseminated intravascular coagulation. He was also found to have splenomegaly, pancytopenia, and cavitary lesions in the lungs at presentation. Further workup showed hyperferritinemia (>90 000 μg/L), hypertriglyceridemia (782 mg/dL), and Epstein-Barr virus (EBV) viremia (61 200 copies/mL). The diagnostic criteria for hemophagocytic lymphohistiocytosis (HLH) were met. Bone marrow biopsy showed extensive hemophagocytosis (panel A, black arrows). The infiltrating neoplastic cells were intensely positive for CD8 immunostaining, suggesting cytotoxic phenotype (panel B), and EBV RNA by in situ hybridization (panel C). Cytogenetic analysis showed complex karyotype and the T-cell gene receptor was clonally rearranged. The final diagnosis was HIV-associated EBV-positive peripheral T-cell lymphoma of cytotoxic phenotype with extensive hemophagocytosis.
The patient received supportive care, including hemodialysis, and was treated with cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone. He tolerated the therapy very well. His mental status and liver functions normalized within the following week, and renal function normalized within the next month. Given his excellent response, he is now being considered for high-dose chemotherapy and autologous stem cell transplantation.
A 46-year-old man with HIV was admitted with subacute onset of fever, cough, generalized weakness, and weight loss. He went on to develop multiorgan failure with encephalopathy, acute kidney injury, fulminant liver failure, and disseminated intravascular coagulation. He was also found to have splenomegaly, pancytopenia, and cavitary lesions in the lungs at presentation. Further workup showed hyperferritinemia (>90 000 μg/L), hypertriglyceridemia (782 mg/dL), and Epstein-Barr virus (EBV) viremia (61 200 copies/mL). The diagnostic criteria for hemophagocytic lymphohistiocytosis (HLH) were met. Bone marrow biopsy showed extensive hemophagocytosis (panel A, black arrows). The infiltrating neoplastic cells were intensely positive for CD8 immunostaining, suggesting cytotoxic phenotype (panel B), and EBV RNA by in situ hybridization (panel C). Cytogenetic analysis showed complex karyotype and the T-cell gene receptor was clonally rearranged. The final diagnosis was HIV-associated EBV-positive peripheral T-cell lymphoma of cytotoxic phenotype with extensive hemophagocytosis.
The patient received supportive care, including hemodialysis, and was treated with cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone. He tolerated the therapy very well. His mental status and liver functions normalized within the following week, and renal function normalized within the next month. Given his excellent response, he is now being considered for high-dose chemotherapy and autologous stem cell transplantation.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.