Key Points
CLL stereotyped subset #2 (IGHV3-21/IGLV3-21) is uniformly aggressive independently of somatic hypermutation status.
The prognosis for non–subset #2/IGHV3-21 CLL resembles that of the remaining CLL cases with similar somatic hypermutation status.
Abstract
An unresolved issue in chronic lymphocytic leukemia (CLL) is whether IGHV3-21 gene usage, in general, or the expression of stereotyped B-cell receptor immunoglobulin defining subset #2 (IGHV3-21/IGLV3-21), in particular, determines outcome for IGHV3-21-utilizing cases. We reappraised this issue in 8593 CLL patients of whom 437 (5%) used the IGHV3-21 gene with 254/437 (58%) classified as subset #2. Within subset #2, immunoglobulin heavy variable (IGHV)-mutated cases predominated, whereas non–subset #2/IGHV3-21 was enriched for IGHV-unmutated cases (P = .002). Subset #2 exhibited significantly shorter time-to-first-treatment (TTFT) compared with non–subset #2/IGHV3-21 (22 vs 60 months, P = .001). No such difference was observed between non–subset #2/IGHV3-21 vs the remaining CLL with similar IGHV mutational status. In conclusion, IGHV3-21 CLL should not be axiomatically considered a homogeneous entity with adverse prognosis, given that only subset #2 emerges as uniformly aggressive, contrasting non–subset #2/IGVH3-21 patients whose prognosis depends on IGHV mutational status as the remaining CLL.
Introduction
The somatic hypermutation (SHM) status of the immunoglobulin heavy variable (IGHV) genes is one of the most robust prognostic markers in chronic lymphocytic leukemia (CLL), allowing the identification of 2 groups with markedly different behavior. Those with no or few somatic mutations (“unmutated,” U-CLL) experience an aggressive disease, whereas those with a heavier SHM load (“mutated,” M-CLL) follow more indolent disease courses.1,2
However, patient stratification into M-CLL and U-CLL should not be unconditional: indeed, cases with borderline IGHV germline identity (GI) should be evaluated and characterized with caution because they comprise a mixture of indolent and aggressive cases.3-6 Moreover, cases with particular B-cell receptor immunoglobulin (BcR IG; eg, those expressing specific IGHV genes) have been reported to not abide by the M-CLL/U-CLL categorization rule.7-9 A paradigmatic example concerns IGHV3-21 gene usage, which has been correlated with shorter overall survival (OS) independently of SHM status.10-12 Interestingly, more than half of CLL cases utilizing the IGHV3-21 gene display highly similar variable heavy complementarity determining region 3 (VH CDR3) sequences and light-chain gene usage9-14 ; thus, they fulfill the criteria of BcR IG stereotypy, a frequent phenomenon in CLL, occurring in ∼30% of patients. These IGHV3-21-stereotyped cases form the largest stereotyped subset within CLL, namely subset #2 (∼3% of all CLL),15 with a distinctive biological profile.16-18 Realizing that subset #2 represents such a major fraction of IGHV3-21 CLL inevitably raised questions about the relative prognostic significance of IGHV3-21 gene usage per se as opposed to subset #2 membership. Put differently, is it the specific gene or the particular stereotyped BcR IG that is linked to clinical aggressiveness?
Previous studies seeking answers to this question have reached quite contradictory results, likely because of the small cohort sizes and the different end points (time to first treatment [TTFT] and/or OS).10,11,13,14,19,20 Although the jury is still out, IGHV3-21 gene usage is notably considered a feature of high-risk CLL and taken into consideration in the context of prospective clinical trials (NCT01243190, NCT01269385, NCT01625741, NCT00562328), clearly indicating the need for careful reappraisal, which is the focus of our study.
Study design
Patients
Overall, 8593 CLL patients were included in the study (supplemental Table 1, available on the Blood Web site). The study was approved by the local Ethics Review Committees.
Biological markers
Interphase fluorescence in situ hybridization, CD38 and zeta-associated protein 70 (ZAP70) expression, polymerase chain reaction amplification, sequence analysis, and interpretation of IGHV-IGHD-IGHJ rearrangements, including stereotyped subset assignment, were performed as reported21-23 (see also supplemental Methods).
Statistical analysis
Differences in frequencies were evaluated using descriptive statistics. OS was measured from the date of diagnosis until the last follow-up or death, whereas TTFT was evaluated from the diagnostic date until the date of initial treatment. Survival curves were constructed with the Kaplan-Meier method, and the log-rank test was used to determine differences between survival proportions. Multivariate Cox regression models were used to test the simultaneous effect of factors on outcomes taking into account the relative effect of remaining parameters. All statistical analyses were performed using Statistica Software 10.0 (Stat Soft Inc., Tulsa, OK).
Results and discussion
Within our series, 437/8593 cases (5%) expressed IGHV3-21 BcR IG. Of these, 254 (58%) were assigned to subset #2 as they shared homologous VH CDR3 sequences of identical length,15 whereas the remaining 183 (42%) IGHV3-21-expressing cases exhibited heterogeneous VH CDR3 lengths and amino acid composition (“non–subset #2/IGHV3-21”; supplemental Table 2).
No differences were observed between subset #2 vs non–subset #2/IGHV3-21 cases regarding age at diagnosis, gender distribution, CD38 and ZAP70 expression, or cytogenetic abnormalities detected by fluorescence in situ hybridization; subset #2 was enriched for Binet B/C cases (Table 1 and supplemental Table 3). Both groups exhibited mixed SHM status (ie, were composed of both M-CLL and U-CLL); however, non–subset #2/IGHV3-21 cases had overall a significantly lower (P = .002) SHM load, with 53% (97/183) of the non–subset #2/IGHV3-21 cases composed of U-CLL as opposed to 39% (98/254) of subset #2 cases. Subset #2 was enriched for cases with borderline identity (97% to 97.99%), whereas non–subset #2/IGHV3-21 M-CLL cases carried a heavier SHM load, more frequently displaying IGHV GI below 97% (supplemental Table 2A).
In order to avoid the possible confounding effects of different treatments, survival analysis was restricted to assessing TTFT in 6744 cases with treatment information (IGHV3-21: n = 355, 5.2%). Subset #2 exhibited a short median TTFT of 22 months, similar to all non-IGHV3-21 U-CLL (24 months, P = ns). Within subset #2, gender, CD38 or ZAP70 expression, the presence of del(13q) or del(17p), and also SHM status had no impact on TTFT (supplemental Table 4 and supplemental Figure 1). Notably, however, among M-CLL subset #2 cases, the presence of del(11q) was associated with significantly shorter TTFT (13 vs 29 months, P = .03); no such differences were observed among U-CLL subset #2 cases (P = .26; supplemental Figure 2A-C).
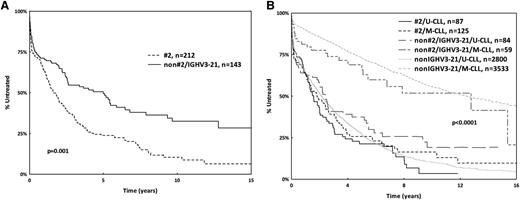
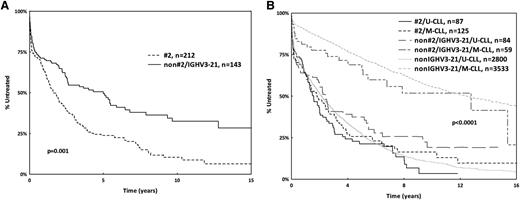
In contrast, non–subset #2/IGHV3-21 cases had significantly longer TTFT compared with subset #2 CLL (60 vs 22 months, P = .001; Figure 1A), also when limiting the analysis to Binet stage-A cases (P = .01; supplemental Figure 2D). This was because of the superior outcome of non–subset #2/IGHV3-21 M-CLL cases (median TTFT 153 months) vs non–subset #2/IGHV3-21 U-CLL cases, which did not differ significantly from subset #2 or all remaining U-CLL cases utilizing IGHV genes other than IGHV3-21 (30 vs 22 vs 24 months, respectively, P = .4). Given the aforementioned differences in SHM load, we also investigated separately cases carrying IGHV genes with <97% GI and found again significantly longer TTFT for non–subset #2/IGHV3-21 vs subset #2 cases (supplemental Figure 3). In multivariate analysis, U-CLL was the only parameter with independent significance (P = .01; supplemental Table 5), indicating that the prognosis of non–subset #2/IGHV3-21 cases is associated with SHM status (Figure 1B) rather than use of a specific IGHV gene and BcR IG as is the case with subset #2.
Kaplan Meier curves for TTFT. (A) Subset #2 exhibits significantly shorter TTFT compared with non–subset #2/IGHV3-21 CLL. (B) No difference regarding TTFT between non–subset #2/IGHV3-21 cases and the remaining CLL. Subset #2 exhibits TTFT similar to that of U-CLL independently of IGHV gene mutational status.
Kaplan Meier curves for TTFT. (A) Subset #2 exhibits significantly shorter TTFT compared with non–subset #2/IGHV3-21 CLL. (B) No difference regarding TTFT between non–subset #2/IGHV3-21 cases and the remaining CLL. Subset #2 exhibits TTFT similar to that of U-CLL independently of IGHV gene mutational status.
This conclusion is based on TTFT assessment and also confirmed within early stage patients only. Most published studies reached an opposite conclusion when assessing OS,10,11,19 which can be considered a limitation because patients may have been treated differently. That notwithstanding, it is worth mentioning that we could not discern any impact of SHM status on OS within subset #2, whereas the OS of non–subset #2/IGHV3-21 cases was influenced by the SHM status (supplemental Figure 4). However, definitive conclusions regarding OS can be reached only by prospective studies on uniformly treated patients.
Interestingly, our study also suggests the possibility to further refine prognosis within subset #2, where the presence of del(11q) within M-CLL subset #2 cases seems to be associated with a more unfavorable clinical profile. Further investigations are required before reaching definitive conclusions regarding this issue and, more generally, the precise impact of genetic aberrations (eg, SF3B1 mutations), which are very frequent in subset #2, yet their prognostic implications remain disputed.17,18
In conclusion, IGHV3-21 gene usage in CLL should not be axiomatically considered as an adverse prognostic indicator (ie, not included tout court in the stratification algorithm of prospective clinical trials). Hence, subset #2 emerges as uniformly aggressive, thus contrasting with non–subset #2/IGHV3-21 patients whose prognosis differs depending on SHM status, similar to all other CLL. Consequently, we argue that knowledge about subset #2 membership is clinically relevant, in particular for stratification purposes within clinical trials. More generally, our findings also support the concept of stratifying CLL based on the molecular features of the BcR IG,24 the ideal clonotypic marker, present in every CLL clone and unaffected by clonal evolution.25
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported in part by the ENosAI project (code 09SYN-13-880) cofunded by the European Union and the General Secretariat for Research and Technology of Greece; the KRIPIS action, funded by the General Secretariat for Research and Technology of Greece; the Swedish Cancer Society, the Swedish Research Council, Uppsala University Hospital, and Lion’s Cancer Research Foundation, Uppsala; the National Institutes of Health, National Cancer Institute (grant CA136591) (D.F.J.); Associazione Italiana per la Ricerca sul Cancro (AIRC) (Investigator Grant and Special Program Molecular Clinical Oncology, 5 per mille #9965) and Ricerca Finalizzata 2010 (RF-2010-2318823), Italian Ministry of Health, Roma; Central European Institute of Technology (CEITEC) grants MU (CZ.1.05/1.1.00/02.0068), SuPReMMe (CZ.1.07/2.3.00/20.0045), and NT13493/2012-4.
Authorship
Contribution: P.B. performed research and wrote the manuscript; A. Agathangelidis, A.H., L.-A.S., E.M., A.T., L.S., Z.D., X.-J.Y., T.S., K.P., Y.S., F.J.V., M.B., T.T., M.C., C.C.C., S.V., A.G., L.M., K.E.S., L.B.P., D.M., K.V.L., V.G., H.S.F., F.N.-K., P.P., G.J., L.A., A. Anagnostopoulos, M.-P.L., M.F., L.T., M.C., M.M., C.H.G., A.W.L., S.P., N.C., D.O., D.F.J., N.D., C.B., and F.D. performed research; P.G., R.R., and K.S. designed the study and wrote the manuscript; and all authors approved the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kostas Stamatopoulos, Institute of Applied Biosciences, Center for Research and Technology Hellas, 57001 Thermi, Thessaloniki, Greece; e-mail: kostas.stamatopoulos@gmail.com.
References
Author notes
P.G., R.R., and K.S. contributed equally to this study.