Abstract

Background: Most non-del 5q lower risk MDS patients (pts) are first treated with ESA, with about 50% (generally transient) responses, and second line treatments (TX) including hypomethylating agent (HMA), Lenalidomide (LEN) and investigational drugs are then often proposed, but their effect on overall survival (OS) is unknown. In a previous work on 253 such pts, we found worse OS with early failure to ESA, i.e. primary resistance (RES) or relapse (REL) < 6 months after ESA onset (Kelaidi, Leukemia, 2013), but only few pts had received, after ESA failure, TX other than RBC transfusions.
In the present study, we gathered non-del 5q lower risk MDS treated with ESA from several EU MDS cooperative groups, and analyzed their outcome after ESA failure, and the effect of second line TX on survival.
Methods: 1611 IPSS low and int-1 (lower risk) non del 5q MDS pts included in the French (GFM), Italian (FISM), Spanish (GESMD), Greek, Düsseldorf and Munich registries between 1997 and 2014, and treated by ESA were studied. Survival was assessed from failure of ESA (i.e. from primary failure evaluated after 12 to 24 weeks of ESA treatment, or from relapse after a response). Progression at ESA failure was defined upon progression to a higher IPSS-R class at ESA failure as compared with ESA onset.
Results: At ESA onset, the 1611 pts were reclassified by IPSS-R in 16% very low, 54% low, 13% int, 6% high, 1% very high and 10% ND. HI-E (using IWG 2006 criteria) to ESA treatment was 66.9%, and the median duration of response was 15 months. The cohort of 1038 pts with ESA failure included 521 RES and 517 REL. Median OS was 4.2 years in REL and 3.7 years in RES pts (p=0.56), and no significant difference was seen, even after restricting the analysis to very low and low IPSS-R pts (p=0.81), or when analyzing "early" vs "late" failures, with cut-off points at 6 or 12 months, as we previously reported (Kelaidi, Leukemia, 2013).
336 (32%) pts received second line treatment (TX2) other than RBC transfusions, including HMA in 88 pts, LEN in 169 pts, and other TX (OT) in 79 pts (including 11 chemotherapy, 17 thalidomide, 11 immunosuppressors (ATG, cyclosporine), or investigational drugs), with response rates of 46%, 39% and 33% respectively (p=0.4). 87 pts had a third line TX (mostly a new drug, but also 7 pts who received HMA after LEN, and 33 pts LEN after HMA).
Pts treated with LEN as TX2 were younger (median age 70 vs 75 for BSC, and 70 for HMA p<10-4), had more RARS (67% vs 28% for BSC and 27% for HMA, p<10-4), while pts treated with HMA as TX2 had more RAEB-1 (34% vs 10% for BSC and 12% for LEN, p<10-4) and more high and very high IPSS-R at onset of TX2 (48% vs 4.6% for BSC and 3.1% for LEN, p<10-4).
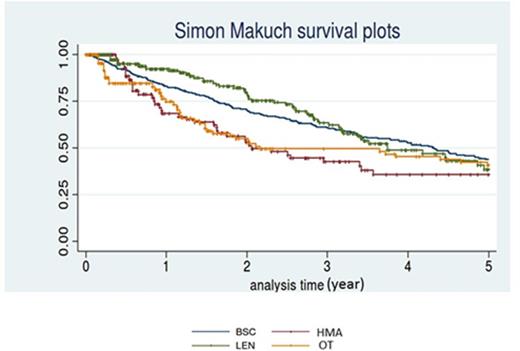
Median OS for pts receiving BSC, LEN, HMA and OT as TX 2 was 4.3y, 3.7y (HR 1.1 [0.81-1.50] p=0.5), 2.1y (HR 1.59 [1.12-2.72], p=0.01) and 2.2y (HR1.17 [0.81-1.68], p=0.41) respectively (Figure). However, in a multivariate analysis adjusted on age, gender, and IPSS-R progression at ESA failure, OS difference became not significant. Analysis of AML progression in the different TX2 groups is currently being finalized.
C onclusion: In this large multicenter retrospective cohort of non-del 5q lower risk MDS pts having failed ESA treatment, OS from failure was similar in RES and REL pts, contrary to our previous smaller experience. About 1/3 of the pts received second line treatments other than RBC transfusion, mainly LEN or HMA. However, none of those treatments was able to improve OS compared to BSC. Newer treatments are required in this situation, possibly including allogeneic SCT in younger pts.
Park:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Hospira: Research Funding; Celgene: Research Funding. Off Label Use: Lenalidomide in non del 5q MDS. Santini:celgene, Janssen, Novartis, Onconova: Honoraria, Research Funding. Cony-Makhoul:BMS: Consultancy, Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau. Cheze:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees. Wattel:PIERRE FABRE MEDICAMENTS: Research Funding; CELGENE: Research Funding, Speakers Bureau; Janssen: Consultancy, Honoraria, Research Funding; NOVARTIS: Research Funding, Speakers Bureau; AMGEN: Consultancy, Research Funding. Vey:Celgene: Honoraria; Roche: Honoraria; Janssen: Honoraria. Fenaux:Amgen: Honoraria, Research Funding; Celgene Corporation: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract