Abstract
Introduction:
Nilotinib is a second generation Tyrosine kinase inhibitor, approved for the treatment of CP-CML after imatinib failure and as frontline therapy. Nilotinib was first used as initial therapy in 2005 and the early results showed deep and fast response rates (JCO 2010 Jan 20; 28(3):392-7). The ENESTnd later showed response rates to be superior to those obtained with imatinib. Here we report the long-term follow-up results of the first trial of nilotinib frontline therapy for CML-CP.
Objective:
To assess the long term outcome of patients with CML treated with nilotinib as initial therapy.
Methods:
We analyzed a total of 148 patients (≥17 years old) with newly diagnosed CML who were enrolled between July 2005 and November of 2014 at MDACC on a clinical trial (NCT00129740) of nilotinib 400mg twice daily.
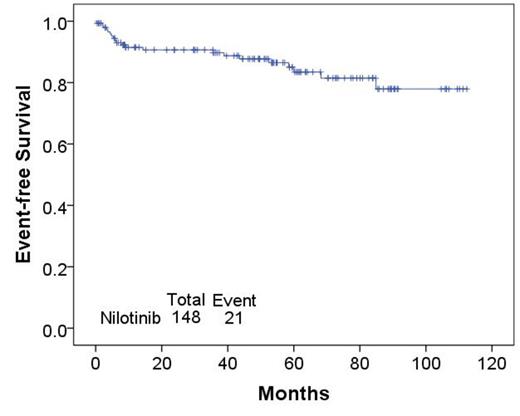
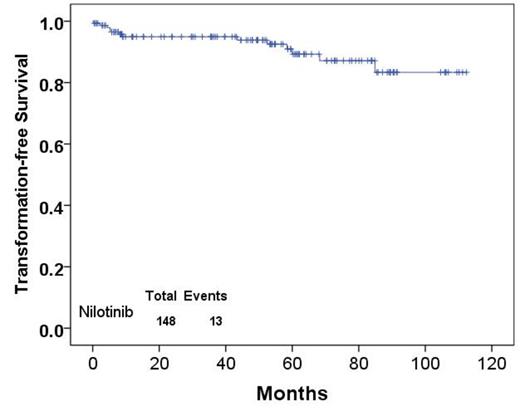
Patients were assessed for cytogenetic and molecular response rate (measured every 3 months for the first year, every 6 month thereafter), overall survival (OS), event-free survival (EFS), transformation-free survival (TFS), and failure-free survival (FFS) using Kaplan-Meier method.
Results:
The baseline patient characteristics are shown on table 1. The median age was 51 years, with 20 patients aged ≥65. High sokal risk score was seen in 17% patients, and 17% of patients were in accelerated phase (AP) at diagnosis. Rates of complete cytogenetic response (CCyR) were: 78% at 3 months, 89% at 1 year, 94% at 5 years, and 97% at 7 years. Rates of MMR were 76% at 1 year, 87% at 5 years, and 93% at 7 years. Corresponding rates of MR4.5 were 39%, 76% and 83%, respectively. With a median follow-up of 59 months, 51 (34%) patients have discontinued therapy. Reasons for treatment discontinuation includes: 9 (6%) with non- cardiac toxicity including 3 with grade ≥3 increase in liver function tests, 2 with acute pancreatitis, 1 with renal failure, 1 with grade ≥2 increase in creatinine, 1 with grade ≥3 elevated lipase, 1 with headache; 6 (4%) with cardiovascular events including 2 myocardial infarction, 1 positive stress test, 1 stroke, 1 pericarditis, and 1 atrial fibrillation; 8 (5%) transformed to blast phase; 5 (3%) for resistance in CP; and 16 (10%) for other reasons including; patient request (n=8), patient noncompliance (n=6), insurance reasons (n=2); and 5 because of death due to unrelated reasons. After nilotinib discontinuation, patients received dasatinib (n=13), imatinib (n=8), bosutinib (n=3), ponatinib (n=2), rebastinib (n=1), chemotherapy plus dasatinib (n=3), AML-like chemotherapy (n=1), hydroxyurea (n=1), stem cell transplant (n=1), and unknown or none (because of lost to follow up, insurance or noncompliance (n=11).
At 1, 5 and 7 year projected OS was 98%, 88% and 88%, respectively; EFS was 91%, 83% and 77%, respectively; TFS was 95%, 89% and 87%, respectively; and FFS was 82%, 70% and 57%, respectively, shown in figure (1,2,3)
Conclusion:
The long-term results from this study of nilotinib as frontline treatment of newly diagnosed CP-CML confirm the excellent results achieved with rapid and deep cytogenetic and molecular response, translating into very favorable long-term survival endpoints. Use of nilotinib in this setting has a favorable toxicity profile confirming its value as frontline therapy for CML-CP.
| Patient Characteristics . | Median [range] or No. (%) . |
|---|---|
| Patients, n | 148 |
| Age, years, median [range] | 51 [17-86] |
| Age ≥65 years | 20 (13) |
| Follow up in months | 59 [0-113] |
| Patients ≥ 65 | 20 |
| Male | 91 (61) |
| CP-CML | 121 (82) |
| AP- CML | 27 (17) |
| Risk score, n (%) - Low - Intermediate - High | 101 (68) 21 (14) 26 (17) |
| WBC (x109/L) | 57 [0.8-342] |
| PB Blast, % | 0 [0-20] |
| BM Blast, % | 2 [0-25] |
| PB Basophil, % | 3 [0-13] |
| BM Basophil, % | 2 [0-13] |
| Splenomegaly,cm | 0 (0-30) |
| Clonal evolution at diagnosis | 3 (0.2) |
| Patient Characteristics . | Median [range] or No. (%) . |
|---|---|
| Patients, n | 148 |
| Age, years, median [range] | 51 [17-86] |
| Age ≥65 years | 20 (13) |
| Follow up in months | 59 [0-113] |
| Patients ≥ 65 | 20 |
| Male | 91 (61) |
| CP-CML | 121 (82) |
| AP- CML | 27 (17) |
| Risk score, n (%) - Low - Intermediate - High | 101 (68) 21 (14) 26 (17) |
| WBC (x109/L) | 57 [0.8-342] |
| PB Blast, % | 0 [0-20] |
| BM Blast, % | 2 [0-25] |
| PB Basophil, % | 3 [0-13] |
| BM Basophil, % | 2 [0-13] |
| Splenomegaly,cm | 0 (0-30) |
| Clonal evolution at diagnosis | 3 (0.2) |
Patient Characteristics: Table (1)
Overall survival
Event-Free Survival
Transformation-free survival
Cortes:Novartis: Consultancy, Research Funding; Teva: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; BMS: Consultancy, Research Funding; ARIAD Pharmaceuticals Inc.: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.