Abstract
Natural killer (NK) cells are a major component of the innate immune system, possessing the ability to lyse their targets without the need for prior sensitization or specificity for antigen. Besides their classical role in providing potent antitumor and antiviral immunity, NK cells can reduce the risk of graft-versus-host disease (GVHD) by targeting host antigen-presenting cells, as well as activated alloreactive donor T cells, indicating that NK-mediated graft-versus-leukemia (GVL) responses may occur in the absence of GVHD. Although most groups have relied on autologous or adult peripheral blood donor-derived NK cells, we have studied umbilical CB as a potential source of NK cells because of their availability as an "off-the-shelf" frozen product and their potent preclinical activity against leukemia cells. To overcome the obstacle of limited numbers of NK cells in a single CB unit, we have established GMP-compliant conditions for the ex vivo expansion of clinically relevant doses of such cells. By using GMP grade K562-based artificial antigen-presenting cells (aAPCs), which express membrane-bound IL-21 (clone 9.mbIL21), to numerically expand highly functional and mature CB-derived NK cells.
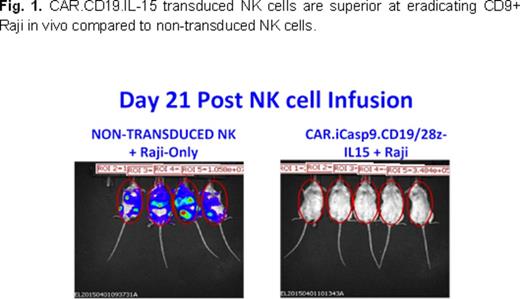
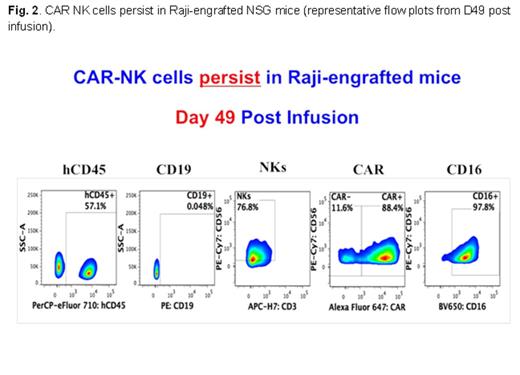
To further enhance the GVL effect independent of KIR-ligand mismatch, we have genetically modified human CB-derived NK cells with a retroviral vector, CAR19-CD28-zeta-2A-IL15 (CAR19/IL15), which incorporates the genes for CAR-CD19, IL-15 to enhance proliferation and survival, and the inducible caspase-9 molecule. CB-NK cells could be stably transduced with CAR19/IL15, proliferated efficiently in vitro and maintained superior effector function against CD19-expressing leukemia cell lines and primary CLL cells. Moreover, the effector functions of both NK-CAR and nontransduced NK cells against K562 were comparable, indicating that the genetic modification of CB-NK cells does not alter their intrinsic cytotoxicity against NK-sensitive targets. Because of concerns over autonomous, uncontrolled NK cell growth due to autocrine production of IL15, we also incorporated into our construct a suicide gene based on the inducible caspase-9 (IC9) gene. The addition of as little as 10 nM of the small molecule dimerizer CID AP20187 to cultures of iC9/CAR19/IL15+ NK cells induced apoptosis/necrosis of >60% of transgenic cells within 4 hours as assessed by annexin-V-7AAD staining. The infusion of CAR.CD19.IL15-transduced CB-NK cells into a NOD-SCID-gamma null model of lymphoblastic lymphoma (Raji model) resulted in impressive anti-tumor responses (Fig. 1). Moreover, adoptively infused CAR-transduced CB NK persisted for up to 70 days post-infusion (Fig. 2), supporting our hypothesis that IL-15 enhances the proliferation and survival of the engineered CB-NK cells. Based on these promising data, we now propose to manufacture a GMP-grade CAR19-CD28-zeta-2A-IL15 vector for a phase 1 dose escalation trial in patients with high risk B-cell leukemia.
Wierda:Celgene Corp.: Consultancy; Glaxo-Smith-Kline Inc.: Research Funding. Rezvani:Pharmacyclics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.