Abstract
Background:
Hodgkin lymphoma (HL) patients who are relapsed/refractory to induction chemotherapy are salvaged with multiagent chemotherapy such as ICE followed by autologous hematopoietic cell transplantation (AHCT). This strategy yields a 2 year EFS of ~65%. Brentuximab vedotin (BV), an antibody drug conjugate, selectively induces apoptosis of CD30+ HL. We previously reported the response rates and toxicities of a multicenter phase II trial evaluating BV as first line salvage therapy in relapsed/refractory HL prior to AHCT. We now report the transplant outcome results of BV as first line salvage therapy in relapsed/refractory HL followed by AHCT.
Patients and Methods:
This is a prospective, multicenter (City of Hope, Cornell Weill Medical College), phase II trial in patients with relapsed/refractory HL prior to AHCT. All patients had biopsy proven relapsed/refractory HL post induction therapy with ABVD, BEACOPP or a combination +/- consolidative XRT. Patients were treated with 1.8 mg/kg of BV intravenously every 3 weeks for a maximum of 4 cycles. Patients who do not achieve CR after BV are allowed to receive multiagent salvage chemotherapy prior to AHCT. The primary endpoint was the best response rate according to revised Cheson criteria. Secondary endpoints were toxicities, stem cell mobilizations, engraftment analysis, and 2 year PFS/OS post AHCT
Results:
37 patients were accrued (Table 1). The overall best response (CR+PR) rate was 69% and CR rate was 35%. 33/37 (89%) patients successfully proceeded to AHCT (1went to alloHCT, 3 could not be salvaged). Among the 13 CR patients, all proceeded to AHCT without additional chemotherapy. Among the 12 PR patients, 4 proceeded to AHCT without additional chemotherapy while 8 received additional chemotherapy (ICE/DICE/IGEV/GND). All patients with SD/PD received additional chemotherapy with exception of 1 patient who received XRT. 24/33 patients were in CR at with 8/33 in PR and 1/33 in SD at time of AHCT.
All patients were primed with cyclophosphamide/G-CSF and 9 patients received plerixafor per institutional guidelines. The median time to collect was 2 days and median cells collected was 5.9 x 10^6 CD34 cells. As AHCT conditioning regimens, 22 patients received BEAM, 9 patients received CBV, and 2 patients received BEAM plus yttrium-90 labeled anti-CD25. The median time to reach ANC engraftment was 11 days and platelet engraftment was 14 days. The response rate post AHCT was 100% in all evaluable patients. Peritransplant toxicities are not evaluated on all patients but will be updated by ASH to include all 33 patients.
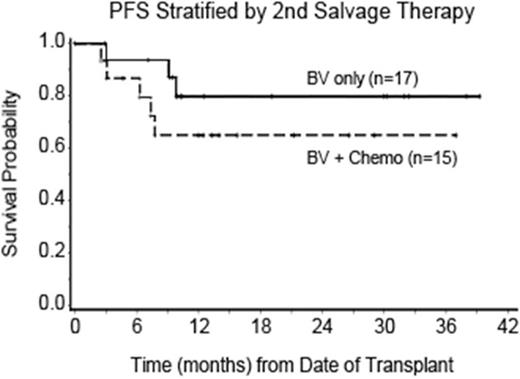
With a median follow up of 17.6 months, the 18 month PFS is 73%, OS is 97%, and NRM is 3%. When stratified by disease status at time of AHCT, the 18 month PFS is 78% for CR and 50% for non CR patients. The 18 month OS is 89% for CR and 88% for non CR patients. When stratified by patients who received BV only vs. BV followed by combination chemotherapy, the 18 month PFS is 80% for BV only vs. 65% for BV followed by combination chemotherapy (Fig 1). The 2 year PFS and OS will be updated by ASH presentation.
Conclusion:
BV as first line salvage therapy results in 89% of patient successfully going to AHCT. The overall 18 month PFS of patients who underwent AHCT is 73%, which compares favorably with historical control. Patients who received BV as the only salvage therapy prior to AHCT without combination chemotherapy had an 18 month PFS of 80%, which also compares favorably with historical control. BV prior to AHCT did not negative impact stem cell collection, engraftment, 18 month NRM, PFS or OS. Given the excellent post transplant outcome, BV as first line salvage is a viable option for relapsed/refractory HL patients undergoing AHCT.
| Characteristics . | N (%) or Median (Range) . |
|---|---|
| Age | 34 (11-67) |
| Institution City of Hope Weill Cornell | 31 (84%) 6 (16%) |
| Stage at Diagnosis I-II III-IV | 19 (51%) 18 (49%) |
| B symptoms | 23 (62%) |
| Bulky Disease (> 5 cm) | 32 (86%) |
| Induction Chemotherapy ABVD ABVD/BEACOPP ABVE-PC | 34 (92%) 2 (5%) 1 (3%) |
| Prior XRT | 9 (24%) |
| Best Response to Induction Primary Refractory Relapsed (within 7 months) | 24 (65%) 13 (35%) |
| Characteristics . | N (%) or Median (Range) . |
|---|---|
| Age | 34 (11-67) |
| Institution City of Hope Weill Cornell | 31 (84%) 6 (16%) |
| Stage at Diagnosis I-II III-IV | 19 (51%) 18 (49%) |
| B symptoms | 23 (62%) |
| Bulky Disease (> 5 cm) | 32 (86%) |
| Induction Chemotherapy ABVD ABVD/BEACOPP ABVE-PC | 34 (92%) 2 (5%) 1 (3%) |
| Prior XRT | 9 (24%) |
| Best Response to Induction Primary Refractory Relapsed (within 7 months) | 24 (65%) 13 (35%) |
Chen:Seattle Genetics, Inc.: Consultancy, Other: Travel expenses, Research Funding, Speakers Bureau; Genentech: Consultancy, Speakers Bureau; Millennium: Consultancy, Research Funding, Speakers Bureau. Off Label Use: 90-Y ibritumomab tiuxetan is a radiotherapeutic antibody targeting CD20. It is part of a regimen indicated for treating patients with relapsed/refractory, low-grade or follicular B cell non-Hodgkin lymphoma (NHL), or patients with previously untreated follicular NHL who achieved a complete or partial response to first-line chemotherapy. Martin:Genentech, Inc.: Consultancy, Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES, Speakers Bureau; Janssen: Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES; Celgene: Consultancy, Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES; Gilead: Consultancy. Siddiqi:Seattle Genetics: Speakers Bureau; Kite pharma: Other: attended advisory board meeting; Pharmacyclics/Jannsen: Speakers Bureau. Nademanee:Spectrum: Research Funding; Gilead: Consultancy; Celgene: Consultancy; Seattle Genetics Inc.: Research Funding. Forman:Mustang: Research Funding; Amgen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.