Abstract
AML in the elderly has a very poor outcome. Despite advances in the characterization of molecular alterations in younger AML patients, comprehensive studies in elderly AML are still lacking to uncover their distinct underlying molecular alterations. In this project, we investigated genetic and epigenetic modifications to unravel the molecular background of this unfavorable disease.
To capture a broad spectrum of relevant alterations in elderly AML, we performed genomic profiling by target enrichment of 555 candidate genes (mutated in cancer), followed by next generation sequencing on an Illumina HiSeq 1500 platform. Reads were mapped to NCBI hg19 RefSeq and SNV or INDELs were called if they were non-silent coding variations with a coverage of at least > 30x and a variant allele frequency higher than 20%. The mean coverage of the target sequence was 382±160x and 98±2% of the target sequence had a read depth of at least 30x. We applied this sequencing strategy on diagnostic bone marrow samples of 100 AML patients enrolled on the Studienallianz Leukämie (SAL) registry. This cohort was composed of patients 65 to 90 years old (median 72 years), 76% were classified as de novo AML, 19% as secondary AML, 5% as therapy-related AML. In addition, we investigated the DNA methylation profile for this cohort with an Illumina 450k methylation array to further characterize the heterogeneity of elderly AML.
Overall, 817 mutations were detected in 292 of the 555 candidate genes, 80 of these genes were mutated in more than two patients. A median number of 7 genes were mutated per patient (range: 1 to 23). Several known mutations were identified with a particular high frequency: DNMT3A 33%, TET2 24%, SRSF2 23%, ASXL1 21%, RUNX1 18%, IDH1 17%, NPM1 15%, IDH2 and BCOR 10% each. We also identified novel aberrations (not previously reported in AML) that provide new insights into the specificity of this disease, including mutations in the PI3K/mTOR pathway (PIK3C2B, MTOR), DNA damage proteins (BRCA2, ERCC2, FANCC, PMS1) and histone modifiers (EP300, JARID2, NSD1, MYST3).
When compared to younger AML (less than 65 years, TCGA cohort NEJM 2013), elderly AML showed significantly higher mutation rates in ASXL1 (21% vs 1%), TET2 (24% vs 7%), RUNX1 (18% vs 7%), BCOR (10% vs 1%) and BRCA2 (8% vs 0%). In addition, we found a high rate of mutations in splicing regulators affecting 38% of elderly AML patients (SRSF2 23%, U2AF1 6%, SF3B1 5%, DDX5 3%, ZRSR2 2%), similarly distributed between de novo and secondary AML.
Notably, 15% of elderly AML patients had mutations in the DNA repair genes TP53, NBN, ATM, FANCA, FANCC, likely responsible for drug resistance and unfavorable outcome: patients with DNA repair mutations had a median survival of only 4 months, compared to 16 months for patients without these mutations (p=5.99e-5); variations in these DNA repair proteins predicted poor overall survival independently of the TP53 mutational status (p=0.004).
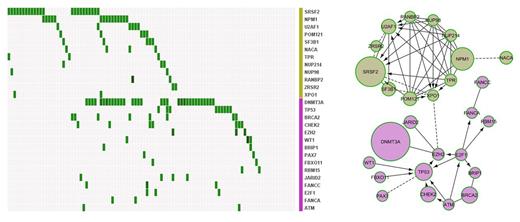
To describe the molecular heterogeneity of the disease we included 152 genes (mutated in more than 1 patient) to build a reactome functional interaction network and identified 9 different network modules. The first most prominent module comprised 15 mutual exclusively mutated genes including DNMT3A and genes of the DNA repair pathway (p=0.013; purple network in figure). The second most distinct module included 12 genes also being altered in a mutually exclusive manner (p=4.9e-4): NPM1, RNA splicing and transport genes (green network in figure). Together the alterations from these two modules affected 88% of the patients and showed no significant overlap (mutual exclusivity test p=7.5e-4). These findings indicate that elderly AML is characterized by two distinct molecular patterns, with patients frequently having one of the two modules altered (mutual-exclusive mutation plot of the two modules in figure).
In conclusion, elderly AML harbors a high frequency of molecular alterations in spliceosome components, epigenetic regulators and in DNA repair factors, the latter being associated with poor prognosis. The characterization of recurrent mutations may guide the development of new strategies to adapt treatment for older AML patients. In this regard, the molecular categorization of elderly AML into two groups (DNA repair or RNA processing deficient) underscores the distinct biology and the need for molecularly driven therapeutic approaches.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.