Abstract
Background: We have previously reported on ethnic disparities in outcomes of multiple myeloma (MM) pts (pts) and shown that Hispanics have the shortest median overall survival (OS) and myeloma-specific survival (MMS) while Asians have the longest. Ethnic minorities are increasing in number in the United States (US) and have been historically underrepresented in population databases with limited follow up since the introduction of novel agents for MM. We did an updated analysis with longer follow up for ethnic minorities to explore the changes in outcomes by race and also explored MM incidence rates, not reported previously.
Methods: Surveillance Epidemiology and End Results (SEER) 13 Registry data (1973-2013) for adult pts (>18 yr) with confirmed diagnosis of MM was utilized. To avoid bias of under representation of ethnic minorities, analysis was restricted to pts diagnosed in 1992 or later. Years of diagnosis were 1992-1995 (pre-stem cell transplant; SCT), 1996-2002 (after SCT but before novel therapeutics) and 2003-2013 (after introduction of novel therapeutics). Cases that received a diagnosis at death certificate/autopsy, without follow-up records, lacking documentation on age at diagnosis, sex, or race/ethnicity were excluded. Cox proportional hazards models were used to evaluate association between patient characteristics and survival. All statistical tests utilized the SAS software (v9.4) and were two-sided with a significance level of 0.05.
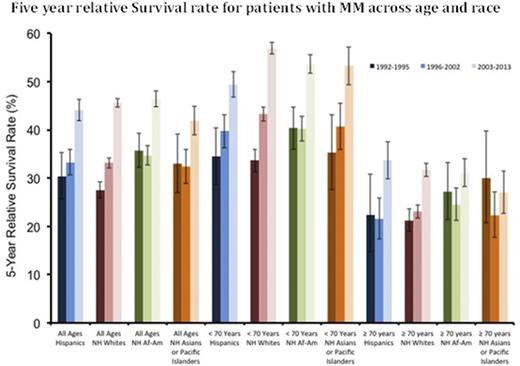
Results: The final analysis included 68431 MM pts (37300 males; 55%, 31131 females; 45%). Age-group cohorts included: 18-44 yr (2519; 4%), 45-54 yr (8131; 12%), 55-64 yr (15416; 23%), 65-74 yr (20214; 30%), and ≥75 yr (22151; 32%). Mutually exclusive racial subgroups included: non-Hispanic White (NHW; 44618, 65%), non-Hispanic African-American (AA; 13164, 19%), non-Hispanic Asian/Pacific Islanders (API; 3570, 5%), Hispanic (H; 6759, 10%) and Native American (NA; 320, 0.5%). Trends in age-specific incidence rates were similar for all races but except the 20-24 yr group, were highest for AA and lowest for API. (Figure 1) Survival analysis showed that females had a better median OS (3.4 vs 3 yr; p<0.001) and MMS (4.7 vs 4.4 yr; p<0.001) than males. Age was an independent predictor of OS (p<0.001) with the median OS changing from 7.3 yr in 18-44 to 1.9 yr in ≥75 age group. Similar results were seen for age groups and MMS as well (p<0.001). During the three pre-specified time periods for year of diagnosis, both the median OS and MMS progressively improved (P<0.001) suggesting improved outcomes secondary to treatment advancements. H and AA had the worst median OS (3.1 yr) as compared to NHW and API (3.3 yr) (p<0.001) and H had the worst median MMS (4.3 yr) while API had the best (5.1 yr) (p<0.001). Survival analyses were performed for ≥75 age group separately since it was the largest and traditionally with worst outcomes. The difference in median OS by gender was still significant (p<0.001) but less pronounced (1.8 vs 1.9 yr) and was not significant for MMS (p=0.33). Due to less SCT utilization, no incremental OS or MMS benefit was seen prior to advent of novel agents but since 2003 the ≥75 group did have a small benefit for OS (2 vs 1.6 yr, p<0.001) and MMS (3 vs 2.3 yr, p<0.001). Race no longer predicted for a statistically significant OS difference (p=0.52) while for MMS, H continued to have the worst (2.5 yr) and NA the best (3.8 yr) outcome (p<0.001). 5-year relative survival rates (RSR) over time showed an incremental improvement in recent years for all racial groups except API ≥70 yr (Figure 2) with generally an increased incremental benefit for the <70 yr age group than the elderly. For majority of races no incremental benefit was seen in 5-yr RSR for ≥70 yr pts between 1992-1995 and 1996-2003 but improvement was seen in 2004-2013.
Conclusions: In a fast changing US demographic mix, significant disparities for MM incidence and outcomes exist by race/ethnicity. As compared to our previous analyses, new trends have emerged with Whites having an improved median OS than AA while H continue to have the worst MMS and API the best. Differences in median OS among races are no longer significant in elderly pts. A modest benefit in OS is being seen for elderly pts since the advent of novel therapeutics. Studies of ethnic disparities are important for evaluating management needs of specific patient populations as well as optimal triaging of healthcare resources.
Kelly:Novartis: Consultancy, Speakers Bureau; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Consultancy, Speakers Bureau. Ailawadhi:Pharmacyclics: Consultancy; Novartis: Consultancy; Amgen Inc: Consultancy; Takeda Oncology: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.