Abstract
One of the adverse consequences of chemotherapy exposure is the development of therapy-related myeloid neoplasms (t-MNs). However, the cause and origin of most t-MNs are unknown, and the prognosis remains dismal. Novel work has shown that in addition to TP53, PPM1D is selectively mutated in 15% of therapy related MDS (Lindsley et al., ASH Abstract). Truncating mutations of PPM1D are also found to commonly occur in clonal hematopoiesis (Jaiswal et al., NEJM 2014; Genovese et al., NEJM 2014; Xie et al., Nat Med 2014), as well as in the blood of cancer patients, particularly after exposure to chemotherapy (Ruark et al., Nature 2013; Swisher et al., JAMA Oncol 2016). We hypothesized that PPM1D truncating mutations confer chemotherapy resistance, causing selective outgrowth of PPM1D mutant hematopoietic stem cells in states of genotoxic stress. In addition, since PPM1D mutations lead to a gain of function, we examined the potential of targeting PPM1D-mutant cells pharmacologically.
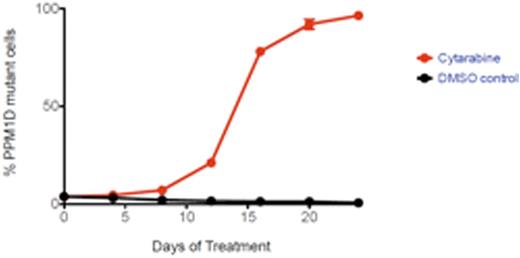
The protein phosphatase PPM1Dis a direct regulator of TP53 activity and the DNA damage response pathway (Fiscella et al., PNAS 1997). Consequently, gain-of-function PPM1D mutations lead to decreased TP53 activity. To examine whether PPM1D mutations drive chemotherapy resistance through an abrogation of the TP53 dependent DNA damage response, we engineered PPM1D-mutant subclones using the CRISPR-Cas9 system in the TP53 wild-type AML cell line MOLM-13. PPM1D exon 6 truncation led to increased expression of PPM1D and resistance to DNA damaging agents, including cytarabine, cyclophosphamide and cisplatin. In addition, PPM1D-mutant cells exhibited a selective advantage over wild-type cells in the presence of chemotherapy, expanding 100-fold over a 24-day period (Fig. 1). While treatment with chemotherapy induced phosphorylation of Chk1 and p53, cell cycle arrest and apoptosis in wild-type cells, this response was abrogated in PPM1D-mutant cells due to gain of function of PPM1D. Using phosphoproteomic analysis, we further demonstrate decreased phosphorylation of known and novel targets in PPM1D-mutant compared to wild-type cells.
We next investigated the effect of PPM1D mutation on normal marrow progenitors in response to chemotherapy treatment in vivo. We performed a competition experiment in which mouse bone marrow c-Kit+ cells expressing Cas9 were transduced with guide RNAs targeting exon 6 of PPM1D or a control guide, and then transplanted into mice in a 1:5 ratio. We observed a selective outgrowth of PPM1D-mutant myeloid cells in the peripheral blood of mice after exposure to chemotherapy. In addition, we found expansion of PPM1D-mutant cells in the lineage negative, c-Kit+ Sca-1+ population, which is enriched for hematopoietic stem cells and multipotent progenitors, indicating that PPM1D-mutant stem and progenitor cells have a competitive advantage over wild-type cells after exposure to genotoxic stress.
The generation of a selective, allosteric inhibitor of PPM1D (Gilmartin et al., Nat Chem Biol 2014) allowed us to examine whether pharmacologic inhibition of PPM1D decreases the chemotherapy resistance or survival of PPM1D-mutant cells. We found that PPM1D-mutant cells have a significantly increased sensitivity to PPM1D inhibition when compared to wild-type controls. In addition, PPM1D inhibitor treatment was able to re-sensitize mutant cells to chemotherapy and abrogate the selective outgrowth of PPM1D-mutant cells during chemotherapy exposure. Lastly, we demonstrate that the proteome-wide phosphorylation profile characteristic of PPM1D-mutant cells can be reversed through treatment with the PPM1D inhibitor.
In sum, these results demonstrate that PPM1D mutations confer a competitive advantage to hematopoietic stem cells undergoing genotoxic stress by abrogating the DNA damage response, and are likely to be the initiating mutation in a large proportion of t-MNs. Due to the gain-of-function nature of this mutation, PPM1D-mutant cells are differentially sensitive to treatment with a PPM1D inhibitor. PPM1D inhibition may therefore provide an opportunity for the prevention and targeted treatment of hematologic malignancies that harbor PPM1D mutations.
PPM1D mutant cells have a competitive advantage under the selective pressure of chemotherapy (cytarabine) treatment.
PPM1D mutant cells have a competitive advantage under the selective pressure of chemotherapy (cytarabine) treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.