Abstract
Background
Post-transplant lymphoproliferative disease (PTLD) represents a spectrum of clinically and morphologically heterogeneous lymphoid proliferations. Histology observed in the monomorphic subtype are similar to those observed in non-Hodgkin Lymphoma (NHL). Most of the PTLD are of B-cell origin, with diffuse large B-cell lymphoma (DLBCL) being the most common histology. Rituximab as a single agent to treat PTLD after organ transplant has demonstrated efficacy in adult patients, but data is limited in pediatric patients1. Recent adult data confirmed that obtaining complete remission after induction with Rituximab identifies a group with B-cell PTLD who do not need chemotherapy2. Low-intensity chemotherapy has been effective in EBV-positive, CD20-positive B-lineage PTLD in children. A study from Children's Oncology using a low intensity chemotherapy including Rituximab, cyclophosphamide and prednisone in children with PTLD after solid organ transplantation in whom immune suppression was reduced, demonstrated a 67% event-free survival3.
We aim to determine if long-term overall survival can be achieved in pediatric monomorphic PTLD DLBCL subtype without chemotherapy.
Methods
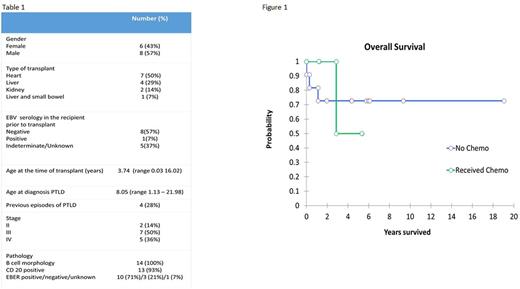
A single institution descriptive retrospective study (November 1998 to April 2017) was conducted in pediatric patients with solid organ transplant who developed monomorphic PTLD (DLBCL subtype). Kaplan-Meier analysis was performed for PTLD overall survival.
Results
Fourteen out of forty-three patients (32%) presented with monomorphic PTLD (DLBCL subtype). Solid organ transplantation included 7 heart, 4 liver, 2 kidney and 1 liver and small bowel transplant. Eight patients were male and 6 were female. Average age at the time of the transplant was 3.74 years (range 0.03-16.02) and at the time of the PTLD presentation was 8.05 (range 1.13-21.98) years. Epstein Barr Virus (EBV) serology prior to transplant showed 8 patients were EBV naive, 1 was seropositive and 5 were indeterminate or unknown. Four patients had been previously treated for other events of PTLD different than DLBCL. All patients were B cell subtype, 10 patients had EBER positive in the biopsy, 3 negative and 1 unknown. Thirteen/fourteen were CD20 positive. Two patients presented with stage II, 7 with stage III and 5 with stage IV (Table 1). Four patients (29%) were treated with reduction of immunosuppression (RIS) +/- antiviral +/- Intravenous Immunoglobulin G (IVIG), 8 patients (57%) received Rituximab + RIS +/- antiviral +/- IVIG, 2 patients (14%) Rituximab and chemotherapy concomitantly. Only one patient treated with Rituximab + RIS initially, presented with progressive disease after being in remission for 3 months requiring chemotherapy treatment. In this cohort, eleven/fourteen patients (79%) did not received chemotherapy. Nine/fourteen (64%) patients remained alive at 5.41 (range 0.01-19.05) years follow-up. The overall survival at 5 years was 73% in the group of patients who did not receive chemotherapy versus 50% in the group who received chemotherapy (Figure 1). None of the patients died as a result of PTLD. Causes of death included graft failure in 2 patients, severe infection with acute respiratory distress syndrome (ARDS) and hepatic failure in 1 patient, chronic lung disease and immunodeficiency in 1 patient and progressive hepatoblastoma, multi-organ failure and ARDS secondary to infection in 1 patient. One patient presented with Classical Hodgkin Lymphoma PTLD 48 months later.
Conclusion
This study suggests that for the majority of pediatric patients with Monomorphic PTLD (DLBCL subtype) long term remission and survival can be achieved without chemotherapy. Prospective data is required to further assess this treatment approach.
References
1 Evens AM et al J Clin Oncol 28(6):1038-46, 2010.
2 Trappe RU et al. J Clin Oncology 34: 1-7, 2016.
3 Gross TG et al. Am J Transplant 12 (11): 3069 - 75, 2012.
Desai: Bristol Myers: Research Funding; St Judes Children's Research Hospital: Research Funding; Alexion: Membership on an entity's Board of Directors or advisory committees. Peters: Lundbeck: Honoraria; Gilead: Honoraria; Janssen: Honoraria; Roche: Honoraria; Abbvie: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.