Abstract
Intoduction:
Allogenic hematopoietic stem cell transplantation (allo-SCT) is a curative procedure for several hematological malignancies. However, this treatment presents a significant morbidity and mortality, mainly related to infection, graft-versus-host disease (GVHD), and conditioning-related toxicity.
In recent years, a number of tissue-specific proteins have been described as biomarkers that could contribute to anticipate post allo-SCT complications. ST2 (suppression of tumorigenicity 2)is a member of the interleukin-1 receptor family and It has been directly related to response to therapy of acute GVHD (aGVHD) and non-relapse mortality (NRM). Our objective was to analyze plasma levels of ST2 at days +15 and +30 post allo-SCT in patients who underwent unmanipulated haploidentical transplantation (HAPLO-HSCT), and to correlate with the NRM and GVHD.
Material an methods:
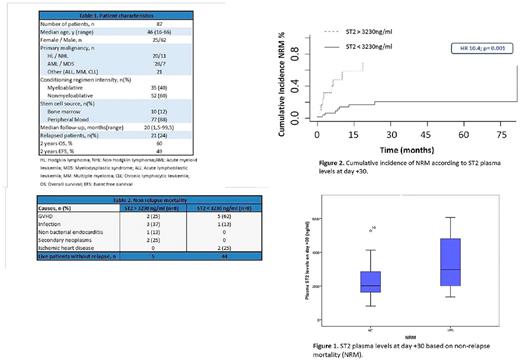
We retrospectively analyzed 110 consecutive patients (2009-2016) who underwent HAPLO-HSCT with post-transplant cyclophosfamide (days +3, +4), MMF and CsA as GVHD prophylaxis. A total of 23 cases were escluded, 9 cases due to early death (before day +30) and 14 cases due lack plasma sample. Characteristics of the 87 patients included in the analysis are described in Table 1. ST2 detection was performed by ELISA (Critical Diagnostics, San Diego, California) according to manufacturer's instructions on 200 μl of plasma obtained at day +15 and +30.
The association of the incidence of aGVHD with known clinical variables and plasma ST2 levels were performed by Cox regression and Mann-Whitney U-test, respectively. The determination of the best cut-off of ST2 levels to stratified patients who died due to toxicity was performed with ROC curves. The statistical program used was R v2.15.0.
Results:
The cumulative incidence (CI) of grade II-IV and grade III-IV aGVHD at 100 days was 51.5% and 14.2%, respectively. CI of relapse and NRM at 2 years was 30% and 22.2% respectively.
No association was found between usual clinical variables (stem cells source, age, sex, conditioning regimen intensity, disease status at trasplant, donor sex, and number of infused CD34 + cells) and NRM and with plasma ST2 levels at day +15 and +30. No differences were found between ST2 levels at day +15 and +30 and II-IV aGVHD, overal survival and steroid-resistant aGVHD.
Highlight, plasma ST2 levels at day +30 were slightly higher in patients who devolped grade III-IV aGVHD compared to patients who did not (median and range, 2503 (524-5275) vs . 2146 (809-4572) ng/ml, p=0.12) with no stadistical significance.
On the other hand, plasma ST2 levels at day +30 were significantly higher in patients with NRM compared to patients who did not (median and range, 2972 (1352-6072) vs. 2015 (809-5275) ng/ml, p= 0.022, Figure 1). Characteristics of NRM are shown in Table 2.
The best cut-off selected on day +30 was 3230 ng/ml (E 82%, S 50%). Patients with higher levels than 3230 ng/ml at day +30 presented a significantly higher incidence of NRM (HR 10.4, p = 0.001, Figure 2).
Conclusion:
Plasma levels of ST2 at day +30 after HAPLO-HSCT correlated with the occurrence of NRM. Prospective studies are needed to better understand the kinetics of ST2 and its possible clinical application.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.