Background: Hematopoietic stem cell transplantation (HSCT) is still the only curative therapy for β-thalassemia major (BTM). Several new approaches have been applied to reduce the toxicity of conditioning regimens, improve strategies for the prevention of graft-versus-host disease (GVHD), and optimize supportive care.
Objectives: This study aimed to evaluate the thalassemia-free survival and outcome of HSCT in the Egyptian experience and to analyze patients and donors' characteristics as well transplantation related factors that could affect the graft success rate.
Methods: We report the results of 174 consecutive first related allogeneic stem cell transplants for children with β‐thalassaemia major performed between January 1997 and December 2014.
Patients and methods: the study included 174 consecutive patients with β-thalassaemia major received allogenic hematopoietic stem cell transplant (HSCT) from HLA fully matched sibling (n=153) or parent (n=10) donners.
Patients mean age was 6.1±4.2 (range: 0.7 to 23.7 yrs.), the median follow up was 34 months (range 1 to 134 months). The Pesaro risk class I, II, and III categories were 21.8, 63.2% and 14.9%, respectively. Bone marrow was the source of stem cells in 26 (14.9%) and peripheral blood(PBSC) in 148 (85.1%)cases. One hundred fifty-seven patients (90.2%) received conditioning with Busulphan(BU) followed by cyclophosphamide. ATG was added in 155/157 patients at a total dose of 110 mg/kg divided into 10 doses (5 pre and 5 post-transplant). Whereas 17 (9.8%) patients received long duration conditioning with Fludarabine, Busulphan followed by cyclophosphamide in 5 patients and ATG was added in 12/17 patients at a total dose of 60 mg/kg. Regarding Graft versus Host Disease GVHD prophylaxis; all patients received cyclosporine (CsA) at a dose of 3 mg/kg/day IV from day -1 until oral intake was possible then shifted to oral dose 5 mg/kg/day divided to 2 daily doses and maintained till day 270, then gradually tapered off. CSA was combined with methotrexate (MTX) in 79 patients (51.3%); at a dose of 15 mg/m2 IV on day +1, then 10 mg/m2 on days +3, +6, and +11. While 75 patients (48.7%) received CSA and methylprednisone 2 mg/kg starting from day -7 till day +4 then tapered gradually over two weeks.
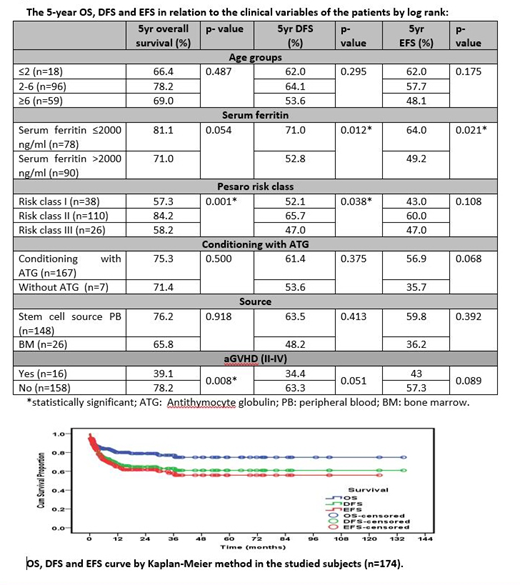
Results: The median time to achieve neutrophil recovery was 18 days (range 8-60 days) and for platelet recovery was 20.5 days (range 7-60 days). Graft failure rate was 12.6% (n=22); 12 (6.9%) as primary and 10 (5.7%) as secondary. The risk of GF was investigated in relation to risk class, serum ferritin level, stem cell source and use of ATG in conditioning regimen. Bone marrow as a source of stem cell was related to a higher graft failure rate (p=0.018) Five-year. Probabilities of overall-, disease-free and event-free survival in all patients were 74.9%, 61% and 55.8%, respectively. Five years overall survival was higher in patients with Pesaro risk class II (p=0.001). Moreover, DFS and EFS were significantly higher in patients with serum ferritin ≤2000 ng/ml (p =0.012, and 0.021 respectively). Transplant related mortality (TRM) was 18.4%, the leading causes of death were infection ( 40.5%), GVHD (16.7%)and respiratory failure(14.3%).
Conclusion: Patients with low serum ferritin , Pesaro Risk Class I &I I and PBSC transplant have a more favorable outcome .Infection was the leading cause of mortality among our patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.