B-cell precursor acute lymphoblastic leukemia (BCP-ALL) is a heterogeneous disease that can be subdivided according to primary recurrent genetic abnormalities that are strongly associated with characteristic biological and clinical features. The first few cases with ZNF384-related rearrangements were described as early as 2002. The leukemic phenotype of these cases was not only BCP-ALL but also mixed phenotype acute leukemia (MPAL) and acute myeloid leukemia (AML) switched from ALL. The number of patients was small because this type of leukemia is rare and many of the fusions are cytogenetically cryptic. RNA sequencing revealed that 1% to 6% of childhood BCP-ALL cases, 5% to 15% of adult BCP-ALL cases and 48% of B/Myeloid MPAL cases harbored ZNF384 rearrangements. Of note, ZNF384 has a variety of partner genes such as TCF3, EP300 and TAF15. Their biological characteristics showed distinct expression profiles, and the cell origin might arise from primitive hematopoietic cells. The clinical features associated with ZNF384-related rearrangements have not been analyzed in a large cohort of patients.
To identify the clinical characteristics of ZNF384-related rearrangements in childhood BCP-ALL (MPAL was excluded), we studied a total with 226 cases of ZNF384-related rearrangements from 15 international consortia who participate in the Ponte di Legno study group registered between 1987 and 2018. We analyzed the impact of outcome in association with clinical and biological characteristics. ZNF384-related rearrangements were detected by fluorescence in situ hybridization (FISH), reverse transcription polymerase chain reaction (RT-PCR) and/or next generation sequencing (NGS), according to local selection policies, or because of poor response to therapy. Additional genetic abnormalities were detected by multiplex ligation-dependent probe amplification (MLPA), single nucleotide polymorphism array (SNP array) and/or NGS.
The median age of presentation was 9 years old (range, 1 - 25 years old). The female and male ratio was 1:1. Immunophenotypic characteristics were classified as BCP-ALL exclusively In addition, 33% were CD10 negative cases (cutoff 20%); 71% were CD13 positive; and 86% were CD33 positive. Complete hematological remission was achieved in 99% of cases. One third (31%) of patients were treated as high risk and one quarter (23%) of patients received a stem cell transplant in first remission. After a median follow-up of 5.3 years, the 5-year event free survival (EFS) rate was 84% (95%CI, 77 to 89%), and the 5-year overall survival (OS) rate was 91% (95% CI, 85 to 94%). There was no difference in survival rate by treatment era or by country or region of origin.
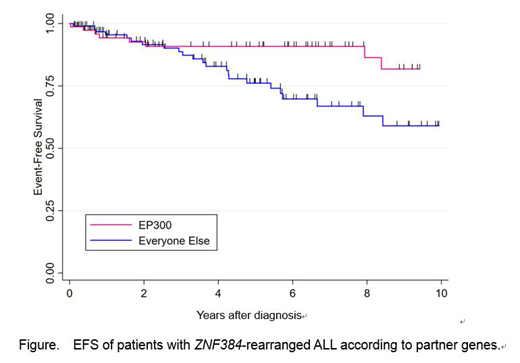
The proportion of partner genes with ZNF384 was as follows: EP300 (37%, n=84), TCF3 (27%, n=60), TAF15 (8%, n=17), CREBBP (7%, n=16), others (8%, n=18) of identifiable partners, and unknown (14%, n=31), although a prospective unselected analysis is needed for an appropriate estimate of the partners distribution. Patients with an EP300-ZNF384 fusion had a significantly lower relapse rate at 5 years compared with the remaining patients: 5% (95% CI 2-14) versus 20% (12-32), hazard ratio 4.58 (1.56-13.45), p=0.006), respectively. The corresponding EFS and OS rates were 91% (81-96) vs. 76% (64-85), p=0.024 and 92% (81-96) vs. 90% (80-95), p=0.3, suggesting that the non-EP300 relapses were salvageable (Figure). Multivariate analysis adjusting for sex, age, WBC and treatment era did not alter these results. Of note, in cases of TCF3 and TAF15, relapse occurred very late even after 5 years from diagnosis. Additional genetic abnormalities such as IKZF1, PAX5, CDKN2A/2B deletions were also analyzed. The distribution of deletions by partner genes was different between fusion partners but were not significant as prognostic factors.
We confirm that ZNF384 rearrangement is a biologically and clinically distinct subtype of BCP-ALL. Immunophenotype abnormalities imply that ZNF384 rearrangements arise from primitive hematopoietic cells. Even considering a potential selection bias for the retrospective nature of the study, the OS was excellent in this subtype, although, relapse events did not reach a plateau among patients with TCF3-ZNF384 and TAF15-ZNF384. On the other hand, EP300-ZNF384 showed good prognosis with a low relapse rate. The biological background in each fusion partner warrants further investigation.
Loh:Medisix Therapeutics, Inc.: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.