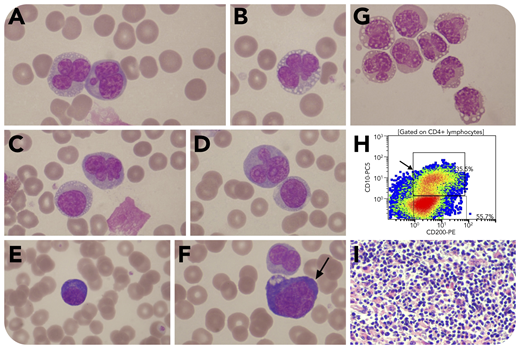
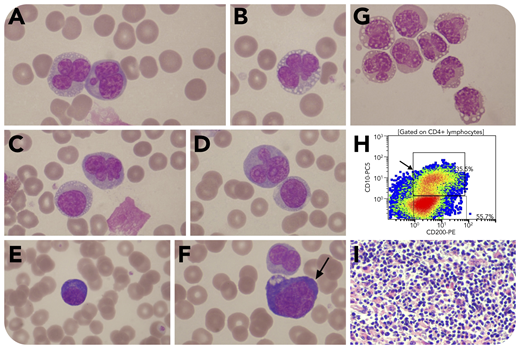
A 54-year-old man was admitted with a 4-week history of recurrent fever, fatigue, and shortness of breath. He had generalized lymphadenopathy, bilateral pleural effusions, splenomegaly, increased lactate dehydrogenase, and polyclonal hypergammaglobulinemia. Hemoglobin was 10.8 g/dL, leukocytes were 21.1 × 109/L (57% neutrophils, 32% lymphocytes, 7% monocytes, 4% eosinophils), and platelets were 207 × 109/L. The blood smear revealed 20% bizarre lymphoid cells with pronounced nuclear convolutions. Most had 3 to 5 nuclear lobulations and a collar of perinuclear vacuoles. Others had round, folded nuclei (panels A-D; original magnification ×1000; May-Grünwald-Giemsa stain). There were also 4% plasmacytoid lymphocytes (panel E; original magnification ×1000; May-Grünwald-Giemsa stain) and immunoblast-like cells (panel F, arrow; original magnification ×1000; May-Grünwald-Giemsa stain). Pleural fluid cytology showed infiltration by the same abnormal lymphoid cells with a single strand of vacuoles around the nucleus giving a “choker necklace” appearance (panel G; original magnification ×800; May-Grünwald-Giemsa stain). Flow cytometry revealed CD3−CD4+CD5+CD7dimCD25−TCL1− T cells coexpressing CD10 and CD200 (panel Η), indicating a T-follicular-helper-cell phenotype. HTLV-1 antibody was negative. These findings suggested a diagnosis of angioimmunoblastic T-cell lymphoma (AITL). Lymph node biopsy showed replacement by abnormal tissue consisting of plasma cells, eosinophils, vascular tissue, and abnormal lymphoid cells (panel I; original magnification ×200; hematoxylin and eosin stain), the latter being CD4+CD10+BCL6+, consistent with AITL. Bone marrow biopsy showed involvement with a similar cellular infiltrate.
This case illustrates that peripheral blood involvement can occur in AITL and teaches us that we should include AITL in the differential diagnosis of CD4+ T-lymphoproliferative disorders associated with circulating cells with hyperlobated nuclei.
A 54-year-old man was admitted with a 4-week history of recurrent fever, fatigue, and shortness of breath. He had generalized lymphadenopathy, bilateral pleural effusions, splenomegaly, increased lactate dehydrogenase, and polyclonal hypergammaglobulinemia. Hemoglobin was 10.8 g/dL, leukocytes were 21.1 × 109/L (57% neutrophils, 32% lymphocytes, 7% monocytes, 4% eosinophils), and platelets were 207 × 109/L. The blood smear revealed 20% bizarre lymphoid cells with pronounced nuclear convolutions. Most had 3 to 5 nuclear lobulations and a collar of perinuclear vacuoles. Others had round, folded nuclei (panels A-D; original magnification ×1000; May-Grünwald-Giemsa stain). There were also 4% plasmacytoid lymphocytes (panel E; original magnification ×1000; May-Grünwald-Giemsa stain) and immunoblast-like cells (panel F, arrow; original magnification ×1000; May-Grünwald-Giemsa stain). Pleural fluid cytology showed infiltration by the same abnormal lymphoid cells with a single strand of vacuoles around the nucleus giving a “choker necklace” appearance (panel G; original magnification ×800; May-Grünwald-Giemsa stain). Flow cytometry revealed CD3−CD4+CD5+CD7dimCD25−TCL1− T cells coexpressing CD10 and CD200 (panel Η), indicating a T-follicular-helper-cell phenotype. HTLV-1 antibody was negative. These findings suggested a diagnosis of angioimmunoblastic T-cell lymphoma (AITL). Lymph node biopsy showed replacement by abnormal tissue consisting of plasma cells, eosinophils, vascular tissue, and abnormal lymphoid cells (panel I; original magnification ×200; hematoxylin and eosin stain), the latter being CD4+CD10+BCL6+, consistent with AITL. Bone marrow biopsy showed involvement with a similar cellular infiltrate.
This case illustrates that peripheral blood involvement can occur in AITL and teaches us that we should include AITL in the differential diagnosis of CD4+ T-lymphoproliferative disorders associated with circulating cells with hyperlobated nuclei.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.