TO THE EDITOR:
Colony-stimulating factor 3 receptor (CSF3R) is a driver of neutrophil differentiation, proliferation, and activation following granulocyte colony-stimulating factor binding, resulting in downstream signaling of tyrosine kinases, including JAK/STAT and SRC.1-3 Activating mutations in CSF3R are highly prevalent in chronic neutrophilic leukemia, but rarely identified in acute myeloid leukemia (AML).4,5 We previously reported on the identification of somatic CSF3R mutations in pediatric AML with a high degree of overlap with CEBPA mutations,6 which are associated with favorable prognosis.7 Small series have also identified CSF3R mutations among patients with the favorable risk lesions of core binding factor (CBF) AML (RUNX1-ETO fusion [t(8;21)] or CBFB-MYH11 [inv(16)/t(16;16)]).8
In this letter, we report on the prevalence and prognostic significance of CSF3R mutations and the impact of cooperating CEBPA mutations and t(8;21) on outcome. A total of 2150 pediatric patients treated on the Children’s Oncology Group phase 3 trials AAML0531 (n = 917) and AAML1031 (n = 1233) with comprehensive clinical and karyotype information were eligible for this study (NCT00372593, NCT01371981). CSF3R mutational status was determined by next-generation sequencing, and CEBPA mutation status was determined by fragment length analysis and Sanger sequencing, both described previously.7,9 Research was approved by the appropriate review boards and conducted in accordance with the Declaration of Helsinki. The Kaplan-Meier method was used to determine 5-year overall survival (OS), event-free survival (EFS), and relapse rate (RR).10 The significance of predictor variables was tested using log-rank statistics for OS and EFS, and Gray statistic for RR. The significance of observed difference in proportions was analyzed by Fisher’s exact test. Complete remission was defined as <5% blasts (AAML0531) or measurable residual disease of <0.1% blasts (AAML1031) at the end of induction 1 (EOI1).
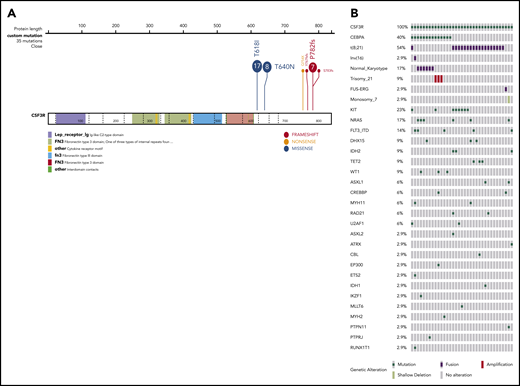
We identified 35 patients (1.6%) with CSF3R mutations (CSF3R+). Mutations occurred in the proximal region of the transmembrane domain (T618I, T640N) or in the cytoplasmic domain as truncating events (Q754X, Y767fs, P7872fs, and S783fs; Figure 1A). T618I (n = 17, 49%) was the most commonly detected mutation. Proximal transmembrane domain mutations result in ligand-independent activation, whereas those in the cytoplasmic domain result in cell surface overexpression with increased activation of downstream signaling pathways.4,11 Among CSF3R+ patients, the overwhelming majority (89%) had a cooccurring t(8;21) fusion (n = 18, 51%) or CEBPA mutation (CEBPA+; n = 12, 34%), whereas 1 patient harbored both a t(8;21) and CEBPA+ (Figure 1B). Among the 13 CEBPA mutations detected, 11 were biallelic and 2 harbored single bZip mutations. Of the 4 patients lacking t(8;21) or CEBPA+, 1 harbored an inv(16). Among non-CBF CSF3R+ patients, n = 6 (50%) had normal cytogenetics (Figure 1B). Additional genomic mutations frequently detected to cooccur with CSF3R included KIT (23%), NRAS (7%), and FLT3/ITD (14%) (Figure 1B). Variant allele frequencies (VAF) were available in 15 patients (43%) with a range of 0.07 to 0.74 (median, 0.29). Among patients with available VAF data, 9 harbored cooccurring signaling mutations (supplemental Figure 1, available on the Blood Web site). Analysis of outcome across patients who relapsed (n = 4; median, 0.28; range, 0.27-0.75) vs no relapse (n = 8; median, 0.325; range, 0.07-0.59) vs induction failure (n = 3; median, 0.29; range, 0.07-0.48) demonstrated similar median VAFs (P = .965).
Location and cooccurring genomic profile of CSF3R mutations in pediatric AML. (A) Protein structure of CSF3R showing location of mutations detected. (B) Mutational profile of CSF3R-mutant samples with cooccurring mutation and cytogenetic changes.
Location and cooccurring genomic profile of CSF3R mutations in pediatric AML. (A) Protein structure of CSF3R showing location of mutations detected. (B) Mutational profile of CSF3R-mutant samples with cooccurring mutation and cytogenetic changes.
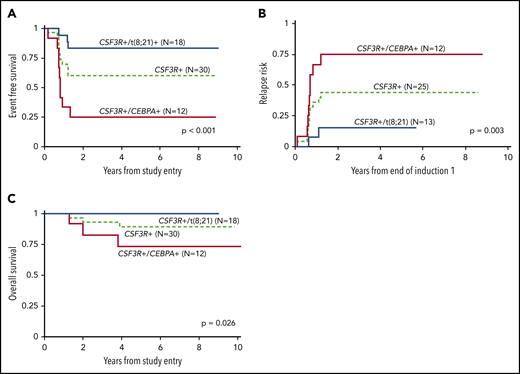
Based on the strong cooccurrence patterns, we analyzed the outcomes for CSF3R+ patients with CEBPA or t(8;21) variants. The EFS for the 31 patients with either of these mutations was 61% ± 18%. However, when stratified based on the cooccurring CEBPA or t(8;21) (n = 30), patients with dual CSF3R+/CEBPA+ had an EFS of 25% ± 25% vs 83% ± 18% for CSF3R+/t(8;21) patients (P < .001; Figure 2A). This was driven by a high RR of 75% ± 28% among CSF3R+/CEBPA+ patients vs 15% ± 21% among CSF3R+/t(8;21) (P = .003; Figure 2B). Despite significantly higher RR and inferior EFS, CSF3R+/CEBPA+ patients experienced an OS of 73% ± 26%, although differences persisted because the CSF3R+/t(8;21) patients experienced an OS of 100% ± 0% (P = .026; Figure 2C). Patients with t(8;21) had a comparable EFS, with a trend toward more favorable outcomes, according to CSF3R+ vs wild-type (WT) of 83% ± 18% vs 67% ± 16% (P = .151); however, a converse relationship was observed in CEBPA+ patients according to CSF3R+ vs WT of 25% ± 15% vs 69% ± 19% (P < .001). Comparison of initial response to therapy of CSF3R+/CEBPA+ vs CSF3R+/t(8;21) patients were similar as measured by achievement of CR (100% vs 76.5%; P = .121) and undetectable measurable residual disease (90% vs 88.2%; P = 1.00).
Outcomes according to CSF3R mutation and cooccurring CEBPA or t(8;21). Outcomes for CSF3R mutant patients according to cooccurring t(8;21) or CEBPA mutation, with overall outcomes of all CSF3R+ patients, including either of the 2 mutations, shown as reference for (A) EFS; (B) RR; (C) OS. P values indicate differences between the t(8;21) vs CEBPA+ subgroups.
Outcomes according to CSF3R mutation and cooccurring CEBPA or t(8;21). Outcomes for CSF3R mutant patients according to cooccurring t(8;21) or CEBPA mutation, with overall outcomes of all CSF3R+ patients, including either of the 2 mutations, shown as reference for (A) EFS; (B) RR; (C) OS. P values indicate differences between the t(8;21) vs CEBPA+ subgroups.
We report the incidence of CSF3R mutations in large cohort of pediatric AML and found that these mutations almost always cooccurred in a mutually exclusive manner with either CEBPA+ or t(8;21). Our findings on the prevalence of CSF3R mutations is in line with prior smaller studies in pediatric AML.6,12 Although t(8;21) and CEBPA+ are associated with favorable outcomes in AML, our findings demonstrate that CSF3R mutations had significant and variable prognostic effects in these groups. This was particularly notable among CEBPA+ patients because dual CSF3R+/CEBPA+ patients experienced poor outcomes with chemotherapy and very high relapse rates. Our studies are in line with recent reports by Su et al describing inferior outcomes with decreased relapse-free survival among CSF3R+/CEBPA+ patients.13,14 In the larger of these 2 studies, CSF3R+ was associated with inferior relapse-free survival and OS in a cohort of adult and pediatric CEBPA+ patients.14 Our findings in a more homogeneously treated pediatric cohort differ as we demonstrate CSF3R+/CEBPA+ patients were highly salvageable. Given that hematopoietic stem cell transplantation (HSCT) is the standard treatment of relapsed AML, our findings implicate efficacy of HSCT in dual CSF3R+/CEBPA+ patients. The use of HSCT has been shown to be an effective therapeutic strategy in CEBPA+ patients, and thus may especially efficacious for a subset with higher risk disease.15
CSF3R mutations occur in patients with severe congenital neutropenia who develop AML, with cooperativity implicated in leukemogenesis, but not solely capable of malignant transformation.16,17 In this setting, strong cooperation between CSF3R and RUNX1, a lineage determining transcription factor, is well recognized, with some studies finding 80% of patients are dual positive for RUNX1 mutations (RUNX1+) and CSF3R+.18 Further, RUNX1+/CSF3R+ CD34+ cells demonstrate enhanced proliferation and diminished proliferation compared with WT or single-mutant cells.18 The t(8;21) fusion similarly perturbs normal RUNX1 function, leading to altered expression of many downstream genes, including repressed CEBPA expression.19,20 Like RUNX1 alterations, CEBPA mutations inhibit myeloid differentiation. Signaling through the CSF3R T618I mutation promotes proliferation and differentiation of neutrophil precursors.21 CEBPA mediates the expression of differentiation-associated genes downstream of CSF3R.22 CEBPA mutations block the pro-differentiation program downstream of CSF3R, but not the proliferative program, leading to an expansion of myeloid cells, with arrested differentiation resulting in a lethal AML phenotype.21 This robust cooperation is consistent with the high rate of relapse observed in our cohort.
Mutations in CSF3R may be amenable to tyrosine kinase inhibitors directed against JAK as robust inhibitory activity has been demonstrated in vitro; however, variable clinical efficacy has been observed in CSF3R+ chronic neutrophilic leukemia.4,23-25 Targeted therapy as well as the conserved and divergent biology between CSF3R+ AML with CEBPA and RUNX1 alterations warrants further investigation. Additional functional studies will also elucidate the clinical differences between CSF3R+/CEBPA+ vs CSF3R+/t(8;21) AML. Our findings highlight that CSF3R mutations can further risk stratify pediatric patients with favorable risk AML. Patients with cooccurring t(8;21) experience excellent outcomes, while those with CEBPA mutations should not be considered favorable risk based solely on presence of a CEBPA mutation or an initial good response to therapy, as they experience very poor outcomes with high relapse rates with chemotherapy alone.
For original data, please e-mail the corresponding author.
The online version of this article contains a data supplement.
Acknowledgments
This work was supported by the National Institutes of Health, National Cancer Institute (grants U10 CA180899, CA 114563, and CA180886-01).
Authorship
Contribution: K.T. and S.M. designed the research; K.T., R.E.R., and T.H. performed the research; T.A., Y.-C.W., R.B.G., and J.L.S. analyzed the data; J.E.M. provided general scientific guidance; and K.T., J.E.M., and S.M. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Katherine Tarlock, 4800 Sand Point Way NE, Seattle Children’s Hospital, Seattle, WA 98105; e-mail: katherine.tarlock@seattlechildrens.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal