Abstract
INTRODUCTION
Acute lymphoblastic leukemia (ALL) is the most common cancer in children. Despite improvements in treatment over the past few decades, stark racial disparities persist in disease risk and cure rates. There is a paucity of data describing the genetic basis of these disparities, especially in relation to modern ALL molecular taxonomy and in the context of contemporary treatment regimens. To this end, we sought to determine the associations of genetic ancestry with ALL biology, and the relevance of genetic ancestry to survival outcomes of modern ALL therapy.
METHODS
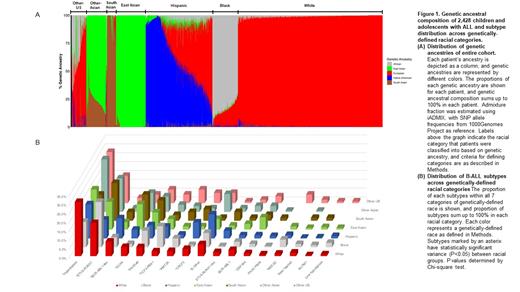
This was a multi-national genomic study of 2,428 children with ALL on front-line trials from United States (St Jude Children's Research Hospital and Children's Oncology Group), South-East Asia (Ma-Spore trials) and Latin America (Guatemala), representing diverse populations of European (EUR), African (AFR), Native American (NA), East Asian (EAS), and South Asian (SAS) descent. We performed RNA-sequencing to characterize ALL molecular subtype, and also estimated their genetic ancestral composition by comparing allele frequencies of patient and reference genomes (1000 Genomes Project reference populations). For categorization of patients into racial groups, individuals were classified based on composition of genetic ancestry as: "white" (EUR >90%), "black" (AFR >70%), "Hispanic" (NA >10% and NA greater than AFR), "East Asian" (EAS >90%), "South Asian" (SAS >70%), with the rest defined as "Other". We then evaluated the associations of ancestry with ALL molecular subtypes and survival.
RESULTS
Genetic ancestral composition of the entire cohort is shown in Figure 1A. Of 21 ALL subtypes, 11 showed significant associations with ancestry. Hyperdiploid ALL was most common in white children (30.6%) and the least frequent in blacks (14.4%) (P<0.001). The frequency of ETV6-RUNX1 was highest in blacks (25.6%) and lowest in Hispanics (10.6%) (P<0.001). The DUX4 subtype was markedly more common in Asian children (14.4% of East Asians and 14.8% of South Asians) compared to black children (1.9%) (P<0.001). There was a similar trend for ZNF384 fusion, representing 6.9% of East Asians, compared to 1.7% for whites (P=0.001). TCF3-PBX1 was most prevalent in blacks at 11.9%, with the lowest at 1.7% in whites (P<0.001). PAX5 alteration frequency was highest in South Asians (11.5%) and lowest in whites (4.5%) (P=0.046). CRLF2 rearrangement occurred significantly more frequently in Hispanics (9.0%) and was least common in blacks (1.3%) (P<0.001). BCR-ABL1-like (excluding CRLF2) was also overrepresented in Hispanic children (11.4%), and occurred less frequently in East Asians (4.2%) (P<0.001). MEF2D fusion was most common in blacks (4.4%), and rare in whites (1.4%) and South Asians (0%) (P=0.013). T-ALL differed dramatically in frequency amongst races, especially between blacks and Hispanics with a 7-fold difference (26.5% vs 3.6%, P<0.001). The pattern of ALL subtype in the "Other" racial category generally mirrored that of the dominant ancestral composition, indicating a strong correlation with ancestry even within admixed populations (Figure 1B).
We then examined outcomes across racial/ethnic categories. Event-free survival (EFS), overall survival (OS) and cumulative incidence of any relapse (CIR) all differed significantly across population groups (P=0.017 for EFS, P=0.05 for OS, P=0.015 for relapse). White, East Asian and South Asian children overall had more favorable outcomes compared to their black and Hispanic counterparts. Specifically, Hispanics had the poorest 5-year EFS (72.1 ± 4.2 %) and OS (82.3 ± 3.6 %), whereas South Asians had the highest EFS (94.6 ± 3.6 %) and OS (98.2 ± 2.1 %). Relapse risk trended in parallel with that of EFS and OS, with South Asians having one of the lowest CIR of 3.7 ± 2.6 %, and Hispanics having the highest at 22.8 ± 2.9 %. We repeated the analysis with genetic ancestry as a continuous variable and obtained largely similar results. Importantly, even after adjusting for biological subtypes and clinical features, Native American and African ancestries remained independently associated with poor prognosis.
CONCLUSIONS
ALL biology and prognosis are highly associated with genetic ancestry, pointing to a genetic basis for racial disparities in ALL. Biology-driven treatment individualization is needed to eliminate racial gaps in the cure of this cancer.
Evans: Princess Máxima Center for Pediatric Oncology, Scientific Advisory Board, Chair: Membership on an entity's Board of Directors or advisory committees; BioSkryb, Inc.: Membership on an entity's Board of Directors or advisory committees; St. Jude Children's Research Hospital, Emeritus Member (began Jan 2021): Ended employment in the past 24 months. Mullighan: Illumina: Membership on an entity's Board of Directors or advisory committees; AbbVie: Research Funding; Pfizer: Research Funding; Amgen: Current equity holder in publicly-traded company. Loh: MediSix therapeutics: Membership on an entity's Board of Directors or advisory committees. Yeoh: Amgen: Honoraria, Other: Chair, Steering Committee for ALL Academy in South East Asia. Pui: Novartis: Other: Data Monitoring Committee; Adaptive Biotechnologies: Membership on an entity's Board of Directors or advisory committees.