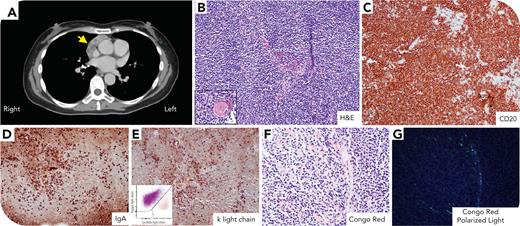
A 57-year-old woman with a history of Sjögren syndrome had an incidental 5.4 × 2.4-cm anterior mediastinal mass on computed tomography (panel A, arrow). A core biopsy demonstrated residual thymic tissue infiltrated by small to medium-sized atypical lymphoid cells with condensed chromatin, inconspicuous nucleoli, and scant cytoplasm (panel B and inset showing Hassall corpuscles, hematoxylin and eosin stain; 20× objective, ×200 total magnification). The neoplastic cells were positive for CD20, immunoglobulin A (IgA) heavy chain, and κ light chain (panels C-E; 20× objective, ×200 total magnification) and negative for IgM, IgG, and λ light chain (data not shown). Flow cytometry confirmed the presence of a κ-restricted B-cell population (panel E, inset), which was negative for CD10 and CD5 (data not shown). Congo red special stain was positive for amyloidosis (panels F-G; 40× objective, ×400 total magnification). Fluorescence in situ hybridization showed no evidence of MALT1 rearrangement. Molecular studies revealed mutation in CARD11, exon 6 p.L251P(c.752T>C). Peripheral blood, bone marrow, and lymph nodes were uninvolved. Laboratory evaluation showed elevated IgA (1501 mg/dL), IgG (3044 mg/dL), and ratio of serum free κ (4.77 mg/dL) to λ (2.03 mg/dL) light chain (2.35). Protein electrophoresis and immunofixation detected IgG κ/IgA κ biclonal gammopathy. There was no clinical suspicion of systemic amyloidosis.
Primary thymic marginal zone lymphoma with amyloidosis is rare but nearly exclusively associated with Sjögren syndrome and has favorable prognosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.