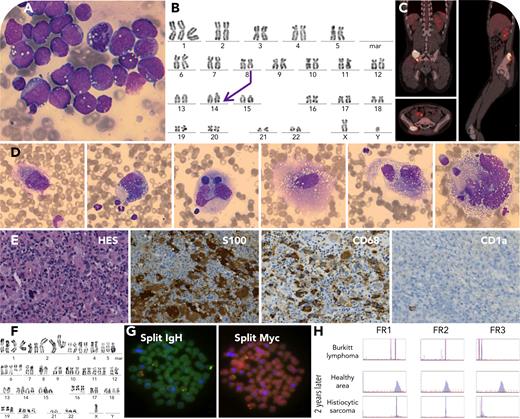
A young boy, previously in remission for 1 year from Burkitt lymphoma with t(8;14) (panels A-B, May-Grunwald-Giemsa (MGG) staining, 100× objective), presented with iliac crest pain. Imaging revealed aggressive lytic lesions in the right sacroiliac joint (panel C). Two bone marrow aspirates were performed in the iliac region. Myelogram of the injured area showed large atypical cells with contoured nuclei, occasionally segmented or multinucleated. The nuclei had nucleoli and fine chromatin. The cytoplasm was vacuolated, with hemophagocytosis, foaminess, basophilia, and occasional flame-like features (panel D, MGG, 100× objective). Biopsy and immunohistochemistry confirmed a proliferation of large cells, S100+, CD68+, and CD1a−, indicating a malignant histiocytic tumor: a histiocytic sarcoma (panel E, hematoxylin-eosin saffron [HES] staining, 40× objective). Cytogenetic analysis revealed a complex karyotype, and fluorescence in situ hybridization demonstrated MYC::IGH rearrangement (panels F-G, original magnification ×1000). The common origin of the initial Burkitt lymphoma and histiocytic sarcoma developed 2 years later was confirmed by studying the immunoglobulin heavy chain rearrangement (panel H). No BRAF V600E mutation was found, but KRAS (p.Q61H; variant allele frequency (VAF) = 9.4%) and TP53 (p.R283H; VAF = 63%) mutations were detected.
The World Health Organization 2022 classification refers to this particular type of histiocytic sarcoma occurring with or after a preceding lymphoma/leukemia, follicular lymphomas, and B-cell acute lymphoblastic leukemia as being the most frequent. The importance of the RAS/MAPK pathway is highlighted, and the pathophysiological process referred to is termed “transdifferentiation.”
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.