Key Points
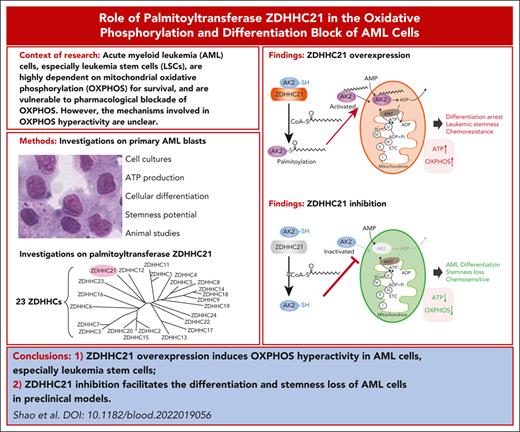
The palmitoyltransferase ZDHHC21 is the key factor that regulates OXPHOS hyperactivity in AML cells as well as LSCs.
ZDHHC21 inhibition facilitates the therapeutic differentiation of AML cells and eradicates AML blasts in relapsed/refractory leukemia.
Abstract
Acute myeloid leukemia (AML) is an aggressive hematological malignancy. Nearly 50% of patients who receive the most intensive treatment inevitably experience disease relapse, likely resulting from the persistence of drug-resistant leukemia stem cells (LSCs). AML cells, especially LSCs, are highly dependent on mitochondrial oxidative phosphorylation (OXPHOS) for survival, but the mechanism involved in OXPHOS hyperactivity is unclear, and a noncytotoxic strategy to inhibit OXPHOS is lacking. To our knowledge, this study is the first to demonstrate that ZDHHC21 palmitoyltransferase serves as a key regulator of OXPHOS hyperactivity in AML cells. The depletion/inhibition of ZDHHC21 effectively induced myeloid differentiation and weakened stemness potential by inhibiting OXPHOS in AML cells. Interestingly, FMS-like tyrosine kinase-3 internal tandem duplication (FLT3-ITD)–mutated AML cells expressed significantly higher levels of ZDHHC21 and exhibited better sensitivity to ZDHHC21 inhibition. Mechanistically, ZDHHC21 specifically catalyzed the palmitoylation of mitochondrial adenylate kinase 2 (AK2) and further activated OXPHOS in leukemic blasts. Inhibition of ZDHHC21 arrested the in vivo growth of AML cells and extended the survival of mice inoculated with AML cell lines and patient derived xenograft AML blasts. Moreover, targeting ZDHHC21 to suppress OXPHOS markedly eradicated AML blasts and enhanced chemotherapy efficacy in relapsed/refractory leukemia. Together, these findings not only uncover a new biological function of palmitoyltransferase ZDHHC21 in regulating AML OXPHOS but also indicate that ZDHHC21 inhibition is a promising therapeutic regimen for patients with AML, especially relapsed/refractory leukemia.
Introduction
Acute myeloid leukemia (AML) is a highly lethal malignancy characterized by the accumulation of hematopoietic stem/progenitor cells.1-3 Despite remarkable insights into molecular pathogenesis and modest advances in treatment, the 5-year survival rate of patients with AML is a dismal 25% to 30%. The current standard treatment strategy for AML is cytarabine plus anthracycline, but patients inevitably experience disease persistence/relapse.4 Novel therapeutic strategies for patients with AML are needed.
AML cells are highly dependent on mitochondrial oxidative phosphorylation (OXPHOS) for survival.5,6 Importantly, increased OXPHOS dependency is frequently a hallmark of cancer stem cells and chemoresistant AML cells.7,8 Targeting OXPHOS is a promising strategy to treat AML, especially relapsed/refractory leukemia. AML blasts are vulnerable to pharmacological blockade of OXPHOS, such as mitochondrial complex I inhibitors (rotenone and IACS-010759)9 and inhibitors of electron transport chain complex subunit synthesis (tigecycline).10 These inhibitors robustly induce cell apoptosis in AML cells, but cytotoxicity concerns still remain because of their cytotoxicity to normal cells by directly targeting the mitochondrial complex.11 Although limited mechanistic evidence has been generated to understand the etiological contributors to OXPHOS, there is a lack of unique intervention strategy to selectively regulate OXPHOS in AML cells.
Posttranslational modifications (PTMs) regulate the localization, stability, protein-protein interactions, and transcription of proteins.12-14 Under pathological conditions, PTMs undergo aberrant balances that cause changes in substrates. PTMs are reversible; therefore, new approaches can be created to selectively correct abnormal PTM alterations. Here, we screened 267 PTM inhibitors and identified a palmitoylation inhibitor that can selectively inhibit OXPHOS in AML rather than hematopoietic stem cells (HSCs). Palmitoylation is essential for the function of both oncoproteins (eg, NRAS and EGFR) and tumor suppressors (eg, SCRIB).15-17 S-palmitoylation is reversible and catalyzed by palmitoyltransferases comprising the zinc finger DHHC-type–containing (ZDHHC) family.18,19 Emerging evidence shows the key role of ZDHHCs in tumorigenesis.20,21 Until now, the impact of palmitoylation on OXPHOS as well as its role in leukemogenesis is still not conclusive.
Here, we revealed that ZDHHC21 was a key factor that regulated OXPHOS hyperactivity in AML cells as well as LSCs by mediating the palmitoylation and mitochondrial localization of adenylate kinase 2 (AK2). The depletion of ZDHHC21 effectively inhibited OXPHOS activity, induced myeloid differentiation, and weakened the stemness potential of AML cells. Interestingly, FMS-like tyrosine kinase-3 internal tandem duplication (FLT3-ITD)–mutated AML cells expressed significantly higher levels of ZDHHC21 and exhibited better sensitivity to ZDHHC21 inhibition. Notably, inhibition of ZDHHC21 markedly eradicated AML blasts and enhanced chemotherapy efficacy in relapsed/refractory leukemia. Here, our study not only establishes a ZDHHC21-mediated mechanism that controls OXPHOS and survival in AML cells as well as LSCs but also indicates that ZDHHC21 is a promising drug target for patients with AML, especially relapsed/refractory leukemia.
Materials and methods
Cells and cell culture
Primary AML blasts (AML-1∼64) from the bone marrow of patients (Children’s Hospital of Zhejiang University and First Affiliated Hospital of Zhejiang University) were isolated using Ficoll-Paque PREMIUM (Cytiva). Details for cells and cell culture are provided in the supplemental Methods, available on the Blood website.
Cellular differentiation analysis
Cell differentiation was determined by assessing CD11b expression, nitro blue tetrazolium (NBT) reduction activity, and morphologic changes as described previously.22 To detect bacterial killing ability, Staphylococcus aureus colonies were first transferred into nutrient broth and shaken overnight. Then, a bacterial killing assay was performed as described previously.23 The bacterial killing activity was calculated using the following formula: killing (%) = (1 − no. tested/no. blank) × 100.
Labeling and detection of S-palmitoylation on AK2 by in-gel fluorescence
Labeling and detection of S-palmitoylation were performed as described previously.24 Briefly, cells were treated with 100 μM Alk-14 for 4 hours. The click chemistry reaction was performed in reaction buffer with 1 μM CY5.5-azide, 500 μM TBTA, 2 mM CuSO4, and 0.2 μM TCEP for 30 minutes at room temperature. The Cy5.5 fluorescence signal was recorded by Amersham Typhoon with 700 nm channel.
ATP production
Intracellular adenosine triphosphate (ATP) levels were measured using an enhanced ATP Assay Kit (Beyotime, Shanghai, China). See the supplemental Methods for details.
Seahorse Cell Mito Stress test
Oxygen consumption rate (OCR) was measured using a 96-well Seahorse Bioanalyzer XFe96, according to the manufacturer’s instructions (Agilent Technologies). Cells were plated on Cell-Tak–coated XF96 cell culture microplates. OCR was measured at basal level and after injection of oligomycin (1.5 μM), fluoro-carbonyl cyanide phenylhydrazone (0.5 μM), antimycin A, and rotenone (0.5 μM).
Identification of the substrates of ZDHHC21 using mass spectrometry
First, the TurboID technique was adopted to identify the interacting proteins of ZDHHC21, as described previously.25 Next, click chemistry was performed to identify the proteins whose palmitoylation was decreased by shZDHHC21. See the supplemental Methods for details.
RNA sequencing assay
RNA sequencing analysis was performed at Shanghai Biotechnology Corporation as described previously.26
Colony-forming cell assay
LSCs or HSCs were first treated with 2-bromopalmitate (2BP) overnight or transduced with lentivirus and then seeded into MethoCult H4434 Classic medium at 4000 cells per mL. The colonies were counted after 14 days.
Animal studies
For the orthotopic xenograft model, AML cells were injected into nonobese diabetic/severe combined immunodeficiency (NOD/SCID) or NOD/SCID gamma (NSG) mice via the tail vein, and the survival times of the mice were recorded. For the subcutaneous xenograft model, AML cells were injected subcutaneously into NSG mice, and then the mice received an intratumoral injection of short hairpin RNA (shRNA) lentivirus. Experiments were conducted as described previously.27-29 Details are available in the supplemental Methods.
Statistical analysis and reproducibility
For all parameters measured, the values for all samples in different experimental conditions were averaged, and the SD or SE was calculated. The statistical significance of differences between groups was determined with an unpaired two-tailed t test analysis, one-way analysis of variance, or log-rank test.
Additional methods are provided in the supplemental Methods.
Results
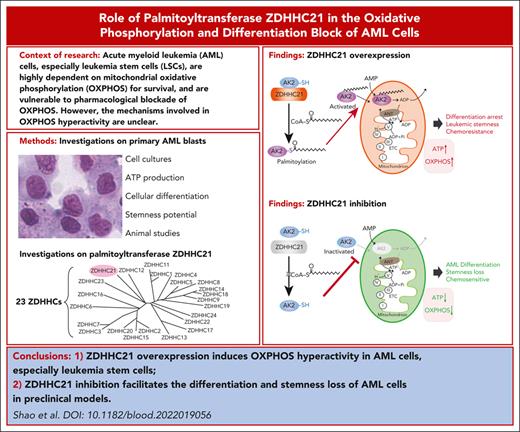
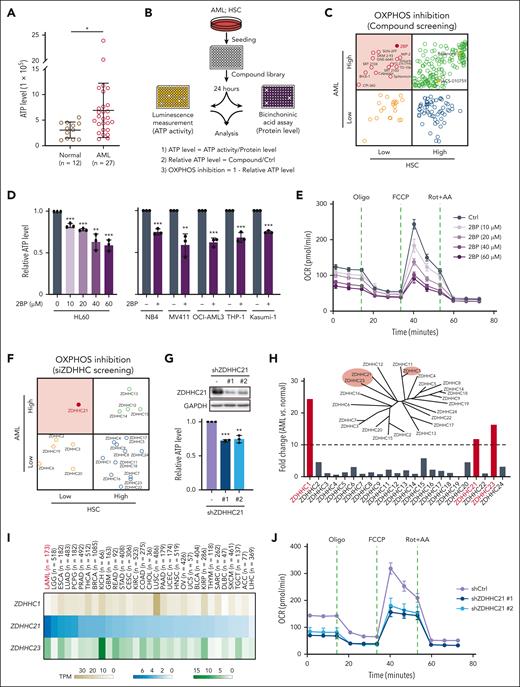
Highly expressed ZDHHC21 specifically regulates OXPHOS hyperactivity in AML cells
First, we characterized the mitochondrial ATP production of leukemic blasts to confirm the bioenergetic status of AML and found that the ATP level of leukemic blasts was much higher than that of normal bone marrow cells (Figure 1A). Then, we established an ATP-based assay to screen for signals that specifically inhibit OXPHOS in AML cells rather than HSCs (Figure 1B). As displayed in Figure 1C, inhibitors of mitochondrial complex I, rotenone and IACS-010759, indeed significantly inhibited ATP level in AML cells (HL60), but they also strongly decreased ATP level in HSCs. Excitingly, among the 267 PTM inhibitors, 16 compounds selectively inhibited OXPHOS in AML cells rather than HSCs, and 2BP, an inhibitor of the ZDHHC palmitoyltransferase family, exerted the strongest efficacy. In addition to HL60 cells, the inhibitory effect of 2BP on ATP was further verified in 5 other AML cell lines (Figure 1D). In addition, another ZDHHC inhibitor, tunicamycin (TM), also inhibited the ATP level of AML cells, whereas the serine palmitoyltransferase inhibitor myriocin did not (supplemental Figure 1A-B). The OCR assay also showed that 2BP led to a significant decrease in the OCR (Figure 1E; supplemental Figure 1C-D), whereas the extracellular acidification rate (ECAR) was unchanged (supplemental Figure 1E-F). These results suggest that ZDHHC palmitoyltransferase inhibitors would selectively regulate OXPHOS in AML cells.
Highly expressed ZDHHC21 specifically regulates OXPHOS hyperactivity in AML cells. (A) The ATP level of healthy donors and patients with AML. (B) Schematic representation of the compound screen. Cellular ATP levels were measured by an enhanced ATP Assay Kit. ATP levels were normalized to their protein concentrations. (C) Relative OXPHOS inhibition in AML cells and HSCs. HL60 cells and HSCs were treated with a collection of 267 PTM inhibitors (10 μM) for 24 hours. Compounds that selectively inhibited OXPHOS in AML cells rather than HSCs are indicated with red circles. Rotenone and IACS-010759, indicated with yellow solid circles, were the positive controls to suppress OXPHOS. (D) The inhibitory effect of 2BP on ATP production in AML cells. HL60 cells were treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM), and other cells lines were treated at a single concentration, including NB4 (60 μM), MV411 (40 μM), OCI-AML3 (60 μM), THP-1 (60 μM), and Kasumi-1 (60 μM). ATP levels were normalized to their protein concentrations. (E) Mitochondrial OCR of HL60 cells after treatment with control (DMSO) or 2BP for 24 hours. (F) Relative OXPHOS inhibition in AML cells and HSCs. HL60 cells and HSCs were transfected with small interfering RNAs targeting ZDHHCs for 72 hours. (G) Top: the protein levels of ZDHHC21 were measured by western blotting to evaluate the silencing efficiency of different shRNA (#1 and #2) against ZDHHC21 in HL60 cells for 5 days. Bottom: cellular ATP levels of shZDHHC21-transfected HL60 cells for 5 days. ATP levels were normalized to their protein concentrations. (H) Relative fold change of gene expression for 173 patients with AML and 70 normal controls obtained from the GEPIA database. The phylogenetic tree represents the sequential evolutionary relationships of a set of ZDHHC family. (I) The expression levels of ZDHHC1, ZDHHC21, and ZDHHC23 were analyzed in 31 cancer species using the GEPIA database. (J) Mitochondrial OCR of HL60 cells infected with lentivirus-shZDHCH21s for 5 days. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or one-way analysis of variance. AA, antimycin A; Ctrl, control; FCCP, fluoro-carbonyl cyanide phenylhydrazone; rot, rotenone.
Highly expressed ZDHHC21 specifically regulates OXPHOS hyperactivity in AML cells. (A) The ATP level of healthy donors and patients with AML. (B) Schematic representation of the compound screen. Cellular ATP levels were measured by an enhanced ATP Assay Kit. ATP levels were normalized to their protein concentrations. (C) Relative OXPHOS inhibition in AML cells and HSCs. HL60 cells and HSCs were treated with a collection of 267 PTM inhibitors (10 μM) for 24 hours. Compounds that selectively inhibited OXPHOS in AML cells rather than HSCs are indicated with red circles. Rotenone and IACS-010759, indicated with yellow solid circles, were the positive controls to suppress OXPHOS. (D) The inhibitory effect of 2BP on ATP production in AML cells. HL60 cells were treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM), and other cells lines were treated at a single concentration, including NB4 (60 μM), MV411 (40 μM), OCI-AML3 (60 μM), THP-1 (60 μM), and Kasumi-1 (60 μM). ATP levels were normalized to their protein concentrations. (E) Mitochondrial OCR of HL60 cells after treatment with control (DMSO) or 2BP for 24 hours. (F) Relative OXPHOS inhibition in AML cells and HSCs. HL60 cells and HSCs were transfected with small interfering RNAs targeting ZDHHCs for 72 hours. (G) Top: the protein levels of ZDHHC21 were measured by western blotting to evaluate the silencing efficiency of different shRNA (#1 and #2) against ZDHHC21 in HL60 cells for 5 days. Bottom: cellular ATP levels of shZDHHC21-transfected HL60 cells for 5 days. ATP levels were normalized to their protein concentrations. (H) Relative fold change of gene expression for 173 patients with AML and 70 normal controls obtained from the GEPIA database. The phylogenetic tree represents the sequential evolutionary relationships of a set of ZDHHC family. (I) The expression levels of ZDHHC1, ZDHHC21, and ZDHHC23 were analyzed in 31 cancer species using the GEPIA database. (J) Mitochondrial OCR of HL60 cells infected with lentivirus-shZDHCH21s for 5 days. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or one-way analysis of variance. AA, antimycin A; Ctrl, control; FCCP, fluoro-carbonyl cyanide phenylhydrazone; rot, rotenone.
To determine which ZDHHC might be involved in the regulation of OXPHOS, small interfering RNAs targeting 23 ZDHHCs were introduced. Results showed that only ZDHHC21 selectively inhibited ATP levels in AML cells but not HSCs (Figure 1F). In addition, siZDHHC21-induced ATP reduction was also phenocopied by shRNAs targeting ZDHHC21 in all 6 AML cell lines (Figure 1G; supplemental Figure 2A-C). Then, we found that the top 3 most upregulated ZDHHCs in AML cells compared with normal cells were ZDHHC1, ZDHHC21, and ZDHHC23 (Figure 1H; supplemental Figure 3A). Among all cancer species, ZDHHC21 but not ZDHHC1 or ZDHHC23 had the highest expression in AML (Figure 1I), which may facilitate the specificity of ZDHHC21 in regulating OXPHOS in AML cells. High expression of ZDHHC21, rather than ZDHHC1 or ZDHHC23, was closely associated with poor prognosis in patients with AML (supplemental Figure 3B). Furthermore, similar to 2BP, ZDHHC21-knockdown AML cells exhibited a dramatic decrease in OCR rather than ECAR (Figure 1J; supplemental Figure 4A-D). Besides, the mitochondrial membrane potential generated by OXPHOS was also decreased by shZDHHC21 (supplemental Figure 4E). Taken together, these findings suggest an essential role for ZDHHC21 in the OXPHOS regulation of AML cells.
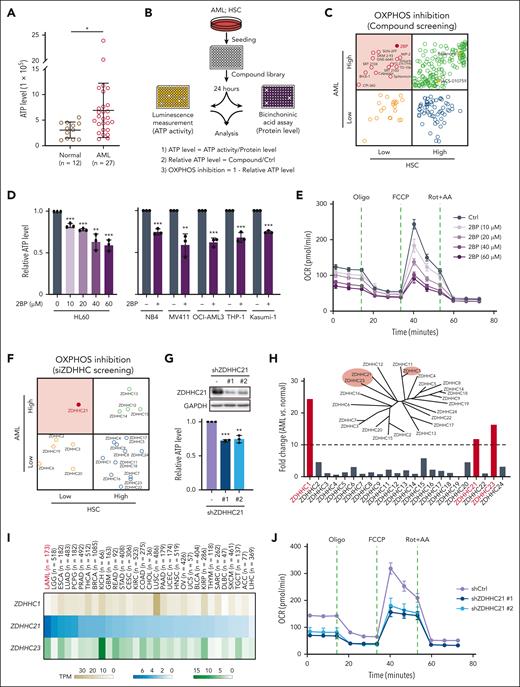
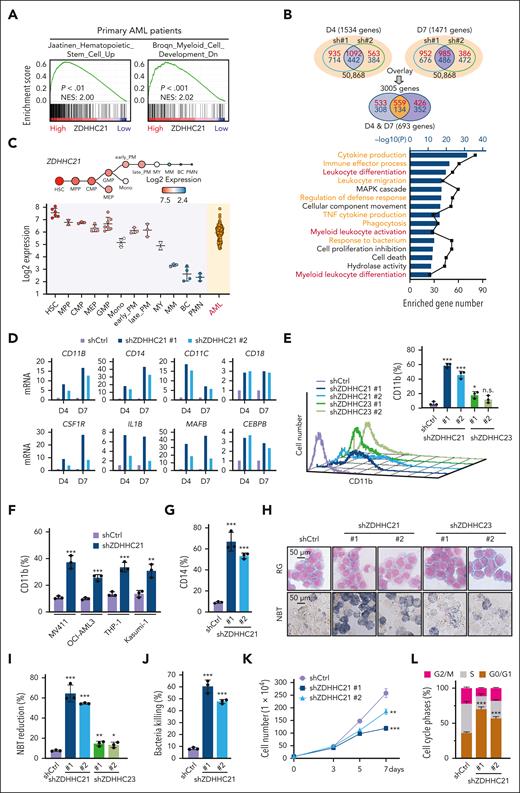
ZDHHC21 activates OXPHOS to arrest the myeloid differentiation of AML cells
To clarify the distant role of ZDHHC21 on AML progression, we performed gene set enrichment analysis and found that genes typically upregulated in HSCs and downregulated in myeloid cell development were highly enriched in patients with high ZDHHC21 expression (Figure 2A). Then, RNA sequencing in shZDHHC21-transduced AML cells showed that 693 altered genes upon shZDHHC21 at days 4 and 7 were highly enriched in differentiation-associated and maturation-related clusters (Figure 2B; supplemental Figure 5A). The differentially expressed genes in shZDHHC21 cells also matched those genes typically downregulated in HSCs and upregulated with myeloid cell development (supplemental Figure 5B). These results prompt that ZDHHC21 may play a role in myeloid differentiation. To further investigate the distant effect of OXPHOS regulated by ZDHHC21 in myeloid differentiation, we analyzed the dynamic expression of ZDHHC21 as well as OXPHOS levels in the different maturation stages of HSCs. As shown in Figure 2C, ZDHHC21 decreased gradually with the differentiation and maturation of HSCs, whereas it was continuously overexpressed in AML cells. Meanwhile, OXPHOS-related genes gradually decreased during the myeloid differentiation process of HSCs (supplemental Figure 5C). In addition, in AML cells with different French-American-British subtypes (M0∼M7), ZDHHC21 expression was also slightly correlated with the stage of differentiation block (supplemental Figure 5D). Moreover, various differentiation markers were also distinctly increased in the shZDHHC21 groups from the RNA sequencing assay (Figure 2D). Therefore, these data strongly suggest that ZDHHC21 knockdown may have an activating effect on the differentiation of AML cells.
ZDHHC21 activates OXPHOS to arrest the myeloid differentiation of AML cells. (A) Gene set enrichment analysis plots depicting enrichment of HSC up gene signature and myeloid cell development down gene signature in the transcriptional profiling of samples with high ZDHHC21 expression in TARGET database. (B) RNA sequencing analysis of HL60 cells infected with lentivirus-shZDHHC21 (#1 and #2) for 4 and 7 days. (Top) Schematic representation of comparing gene expression profiles in HL60 cells. Overlapped smaller circles reflected the shared genes induced by different lentivirus-shZDHHC21s on day 4 (left; blue) and day 7 (right; purple), respectively. Overlapped smaller oval reflect the shared 693 genes induced on both day 4 and day 7. Red numbers in circles represent upregulation, whereas blue numbers represent downregulation. (Bottom) The functional clustering analysis of the changed genes after overlapping screening using Metascape. The −log10(P) values mean the enrichment score, representing the degree of participation. The number of enriched genes is also shown. (C) The expression levels of ZDHHC21 in primary AML cells or normal hematopoietic cells of various lineages were obtained from the BloodSpot database. (D) RNA sequencing analysis showed the messenger RNA changes of differentiation marker genes (C/EBPB, CD18, IL1B, CD11C, CD18, CD14, MAFB, CSF1R, and CD11B) in HL60 cells infected with lentivirus-shZDHHC21. (E) CD11b expression of HL60 cells infected with lentivirus-shZDHHC21 or lentivirus-shZDHHC23 for 7 days. (F) CD11b expression of different AML cell lines infected with lentivirus-shZDHHC21. (G) CD14 expression of HL60 cells infected with lentivirus-shZDHHC21 for 7 days. (H) Cell differentiation of HL60 cells infected with lentivirus-shZDHHC21 or lentivirus-shZDHHC23 for 7 days. (Top row) Cell morphological analysis after Wright-Giemsa staining. (Bottom row) NBT-reducing activity. Data are representative of at least 3 individual experiments, and 1 representative image is shown. (I) Quantitative analysis of NBT-reducing activity of HL60 cells infected with lentivirus-shZDHHC21 or lentivirus-shZDHHC23 for 7 days. (J) Bacterial killing ability of HL60 infected with shZDHHC21 lentivirus for 7 days. Clearance efficiency was determined from the numbers of viable bacteria recovered from the intracellular compartment after infection. Staphylococcus aureus was used to infect AML cells. (K) The cell proliferation assay showed proliferation inhibition caused by ZDHHC21 knockdown in HL60 cells. (L) Flow cytometry analysis of cell cycle distribution in HL60 cells after silencing ZDHHC21 for 5 days. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗∗P < .001 vs shCtrl. The significance analysis was conducted by a two-tailed unpaired t test or one-way analysis of variance. BC, band cell; CMP, common myeloid progenitor; early_PM, early promyelocyte; FDR, false discovery rate; GMP, granulocyte-monocyte progenitor; HSC, hematopoietic stem cell; MEP, megakaryocyte-erythrocyte progenitor; late_PM, late promyelocyte; MM, metamyelocyte; mono, monocyte; MPP, multipotent progenitor; MY, myelocyte; NES, normalized enrichment score; PMN, polymorphonuclear cell.
ZDHHC21 activates OXPHOS to arrest the myeloid differentiation of AML cells. (A) Gene set enrichment analysis plots depicting enrichment of HSC up gene signature and myeloid cell development down gene signature in the transcriptional profiling of samples with high ZDHHC21 expression in TARGET database. (B) RNA sequencing analysis of HL60 cells infected with lentivirus-shZDHHC21 (#1 and #2) for 4 and 7 days. (Top) Schematic representation of comparing gene expression profiles in HL60 cells. Overlapped smaller circles reflected the shared genes induced by different lentivirus-shZDHHC21s on day 4 (left; blue) and day 7 (right; purple), respectively. Overlapped smaller oval reflect the shared 693 genes induced on both day 4 and day 7. Red numbers in circles represent upregulation, whereas blue numbers represent downregulation. (Bottom) The functional clustering analysis of the changed genes after overlapping screening using Metascape. The −log10(P) values mean the enrichment score, representing the degree of participation. The number of enriched genes is also shown. (C) The expression levels of ZDHHC21 in primary AML cells or normal hematopoietic cells of various lineages were obtained from the BloodSpot database. (D) RNA sequencing analysis showed the messenger RNA changes of differentiation marker genes (C/EBPB, CD18, IL1B, CD11C, CD18, CD14, MAFB, CSF1R, and CD11B) in HL60 cells infected with lentivirus-shZDHHC21. (E) CD11b expression of HL60 cells infected with lentivirus-shZDHHC21 or lentivirus-shZDHHC23 for 7 days. (F) CD11b expression of different AML cell lines infected with lentivirus-shZDHHC21. (G) CD14 expression of HL60 cells infected with lentivirus-shZDHHC21 for 7 days. (H) Cell differentiation of HL60 cells infected with lentivirus-shZDHHC21 or lentivirus-shZDHHC23 for 7 days. (Top row) Cell morphological analysis after Wright-Giemsa staining. (Bottom row) NBT-reducing activity. Data are representative of at least 3 individual experiments, and 1 representative image is shown. (I) Quantitative analysis of NBT-reducing activity of HL60 cells infected with lentivirus-shZDHHC21 or lentivirus-shZDHHC23 for 7 days. (J) Bacterial killing ability of HL60 infected with shZDHHC21 lentivirus for 7 days. Clearance efficiency was determined from the numbers of viable bacteria recovered from the intracellular compartment after infection. Staphylococcus aureus was used to infect AML cells. (K) The cell proliferation assay showed proliferation inhibition caused by ZDHHC21 knockdown in HL60 cells. (L) Flow cytometry analysis of cell cycle distribution in HL60 cells after silencing ZDHHC21 for 5 days. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗∗P < .001 vs shCtrl. The significance analysis was conducted by a two-tailed unpaired t test or one-way analysis of variance. BC, band cell; CMP, common myeloid progenitor; early_PM, early promyelocyte; FDR, false discovery rate; GMP, granulocyte-monocyte progenitor; HSC, hematopoietic stem cell; MEP, megakaryocyte-erythrocyte progenitor; late_PM, late promyelocyte; MM, metamyelocyte; mono, monocyte; MPP, multipotent progenitor; MY, myelocyte; NES, normalized enrichment score; PMN, polymorphonuclear cell.
Then, we detected the effect of shZDHHC21 on myeloid differentiation by evaluating differentiation markers, NBT reduction, nuclear morphology, and bactericidal activity. shRNAs specifically targeting ZDHHC21 or ZDHHC23 were introduced into AML cells (supplemental Figure 6). shZDHHC21 significantly increased CD11b expression in HL60 cells, whereas shZDHHC23 exerted a weak effect (Figure 2E). Similar CD11b upregulation upon shZDHHC21 was also obtained in 5 other AML cell lines (Figure 2F; supplemental Figure 7A-B). shZDHHC21 also dramatically enhanced CD14 expression (Figure 2G; supplemental Figure 7C-D). Moreover, compared with ZDHHC23, ZDHHC21-declined HL60 cells had a more mature nuclear morphology and enhanced NBT-reducing ability (Figure 2H-I). Similar results were obtained in ZDHHC21-declined NB4 cells (supplemental Figure 7E). More importantly, ZDHHC21-depleted cells displayed significant bacterial-killing ability (Figure 2J; supplemental Figure 7F). In addition, along with terminal differentiation, shZDHHC21 obviously inhibited cell proliferation (Figure 2K; supplemental Figure 7G) and induced G0/G1 cell cycle arrest (Figure 2L; supplemental Figure 7H) as well as apoptosis (supplemental Figure 8). Taken together, these results clearly demonstrate that shZDHHC21 drives myeloid differentiation and maturation in AML cells.
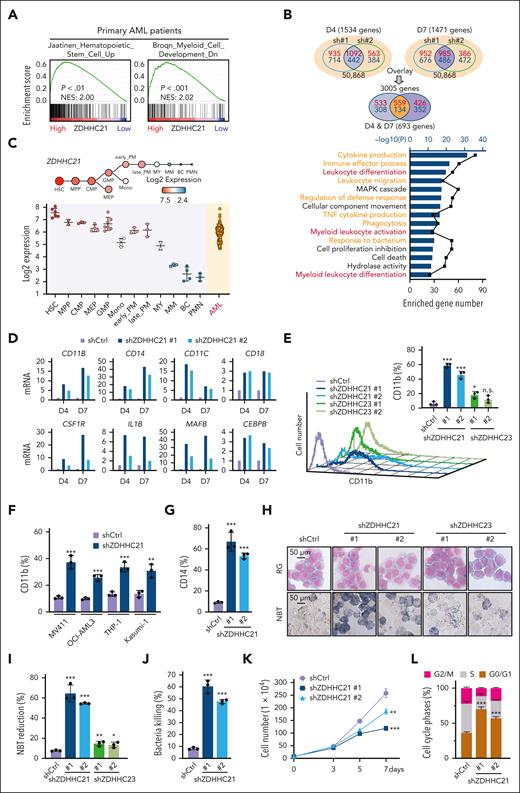
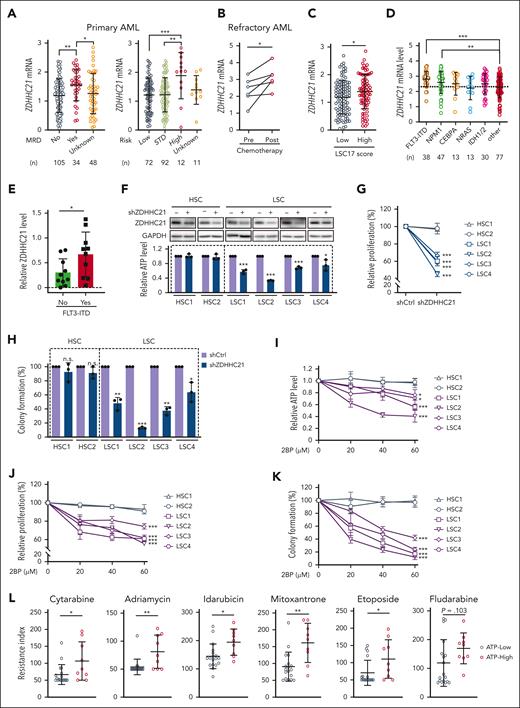
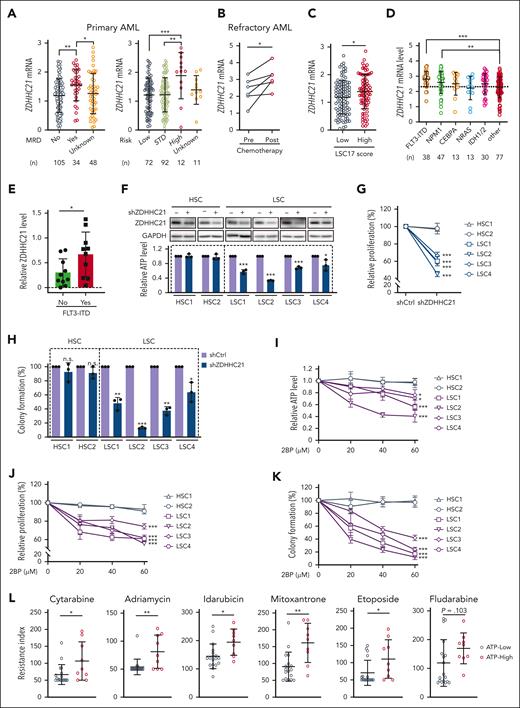
ZDHHC21 regulates the stemness potential of LSCs and chemotherapy resistance of AML cells
Studies have shown that leukemia stem cells (LSCs) as well as chemoresistant AML cells exhibit higher OXPHOS activity; thus, we analyzed the expression of ZDHHC21 in primary patients with AML with poor prognosis as well as refractory AML. As shown in Figure 3A, ZDHHC21 was significantly higher in patients with minimal residual disease as well as in high-risk patients, which may result from LSCs and/or chemoresistant blasts. Next, along with the phenomenon that LSC maintenance and the OXPHOS signature were strongly enriched in postchemotherapy AML blasts, ZDHHC21 expression increased markedly (Figure 3B; supplemental Figure 9A). Moreover, the LSC17 score is an indicator of LSC stemness as well as poor prognosis and drug resistance.30 We found that ZDHHC21 was also upregulated in patients with AML with a high LSC17 score (Figure 3C). In addition, the FLT3-ITD mutation is reported to be positively correlated with leukemia stemness and drug resistance,31 and ZDHHC21 was found to be highly expressed in patients with the FLT3-ITD mutation based on 2 AML databases (Figure 3D; supplemental Figure 9B) and our primary AML sample results (Figure 3E; supplemental Figure 9C). Therefore, these results indicate a possible correlation between high ZDHHC21 expression and LSCs.
ZDHHC21 regulates the stemness potential of LSCs and chemotherapy resistance. (A) Left: quantitative analysis of ZDHHC21 messenger RNA expression in patients with AML with (n = 34) or without (n = 105) MRD. Right: quantitative analysis of ZDHHC21 messenger RNA expression in patients with AML with low-risk stage (n = 72), standard-risk stage (n = 92), and high-risk stage (n = 12). Data are derived from the TARGET database. (B) Expression of ZDHHC21 in pre- and postchemotherapy flow-sorted AML blast populations (n = 6). The data are derived from the GSE162542 cohort. (C) Expression of ZDHHC21 in low LSC17 score and high LSC17 score from the TARGET database. (D) Expression of ZDHHC21 in different genetic subtypes of human AMLs. Data are derived from the TCGA database. (E) The correlation of ZDHHC21 protein expression with FLT3-ITD mutation in patients with AML. (F) Top: the protein levels of ZDHHC21 were measured by western blotting to evaluate the silencing efficiency of ZDHHC21 in HSCs or LSCs. HSCs from 2 healthy sources were used as controls. LSCs were sorted by CD34 marker from AML specimens. Bottom: cellular ATP levels of shZDHHC21-transfected HSCs or LSCs. ATP levels were normalized to their protein concentrations. LSC1 were sorted from patient AML28 via the CD34 marker, LSC2 were sorted from AML45, LSC3 were sorted from AML46, and LSC4 were sorted from AML33. (G) The relative proliferation of HSCs or LSCs infected with lentivirus-shZDHHC21. (H) The effect of shZDHHC21 on the colony-forming ability of HSCs and LSCs after culturing in methylcellulose medium for 2 weeks. (I) The inhibitory effect of 2BP on ATP production in HSCs and LSCs. Cells were treated with 2BP at a series of concentrations (0, 20, 40, 60 μM). (J) The relative proliferation of HSCs or LSCs treated with 2BP by a series of concentrations (0, 20, 40, 60 μM). (K) The effect of 2BP on the colony-forming ability of HSCs and LSCs after culturing in methylcellulose medium for 2 weeks. (L) Drug sensitivity analysis of primary patient cells. Primary AML cells were treated with chemotherapy drugs. The CellTiter-Glo measurement was used to determine the number of viable cells. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or a one-way analysis of variance. MRD, minimal residual disease.
ZDHHC21 regulates the stemness potential of LSCs and chemotherapy resistance. (A) Left: quantitative analysis of ZDHHC21 messenger RNA expression in patients with AML with (n = 34) or without (n = 105) MRD. Right: quantitative analysis of ZDHHC21 messenger RNA expression in patients with AML with low-risk stage (n = 72), standard-risk stage (n = 92), and high-risk stage (n = 12). Data are derived from the TARGET database. (B) Expression of ZDHHC21 in pre- and postchemotherapy flow-sorted AML blast populations (n = 6). The data are derived from the GSE162542 cohort. (C) Expression of ZDHHC21 in low LSC17 score and high LSC17 score from the TARGET database. (D) Expression of ZDHHC21 in different genetic subtypes of human AMLs. Data are derived from the TCGA database. (E) The correlation of ZDHHC21 protein expression with FLT3-ITD mutation in patients with AML. (F) Top: the protein levels of ZDHHC21 were measured by western blotting to evaluate the silencing efficiency of ZDHHC21 in HSCs or LSCs. HSCs from 2 healthy sources were used as controls. LSCs were sorted by CD34 marker from AML specimens. Bottom: cellular ATP levels of shZDHHC21-transfected HSCs or LSCs. ATP levels were normalized to their protein concentrations. LSC1 were sorted from patient AML28 via the CD34 marker, LSC2 were sorted from AML45, LSC3 were sorted from AML46, and LSC4 were sorted from AML33. (G) The relative proliferation of HSCs or LSCs infected with lentivirus-shZDHHC21. (H) The effect of shZDHHC21 on the colony-forming ability of HSCs and LSCs after culturing in methylcellulose medium for 2 weeks. (I) The inhibitory effect of 2BP on ATP production in HSCs and LSCs. Cells were treated with 2BP at a series of concentrations (0, 20, 40, 60 μM). (J) The relative proliferation of HSCs or LSCs treated with 2BP by a series of concentrations (0, 20, 40, 60 μM). (K) The effect of 2BP on the colony-forming ability of HSCs and LSCs after culturing in methylcellulose medium for 2 weeks. (L) Drug sensitivity analysis of primary patient cells. Primary AML cells were treated with chemotherapy drugs. The CellTiter-Glo measurement was used to determine the number of viable cells. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or a one-way analysis of variance. MRD, minimal residual disease.
We then examined the role of ZDHHC21 in the stemness potential of LSCs. We sorted CD34+ LSCs from 4 AML specimens with a relatively high percentage of CD34+ cells. Among them, 3 of 4 patients were diagnosed with relapsed AML. Results showed that shZDHHC21 obviously inhibited the OXPHOS activity of LSCs rather than HSCs (Figure 3F). Moreover, shZDHHC21 significantly suppressed the proliferation and colony formation of LSCs, whereas HSCs were not influenced (Figure 3G-H; supplemental Figure 9D). Similar selective inhibitory effects on OXPHOS, cell proliferation, and colony formation ability in LSCs rather than HSCs were also observed upon 2BP treatment (Figure 3I-K; supplemental Figure 9E). These results demonstrate that ZDHHC21 depletion/inhibition potently weakens the stemness potential of LSCs, and targeting ZDHHC21 has minimal toxicity on HSCs. More importantly, primary AML samples with high OXPHOS showed poorer sensitivity to chemotherapy, including the standard treatment drugs cytarabine and Adriamycin (doxorubicin) as well as other chemotherapy drugs (Figure 3L). These results indicate that the high level of OXPHOS regulated by ZDHHC21 may lead to leukemic stemness and chemoresistance in AML.
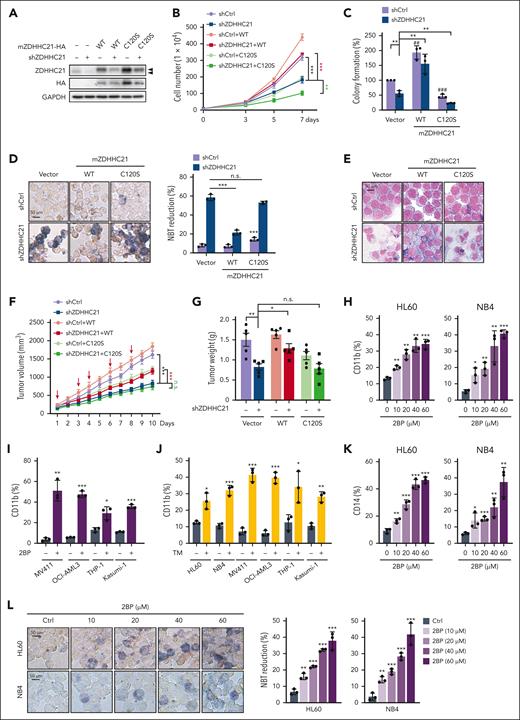
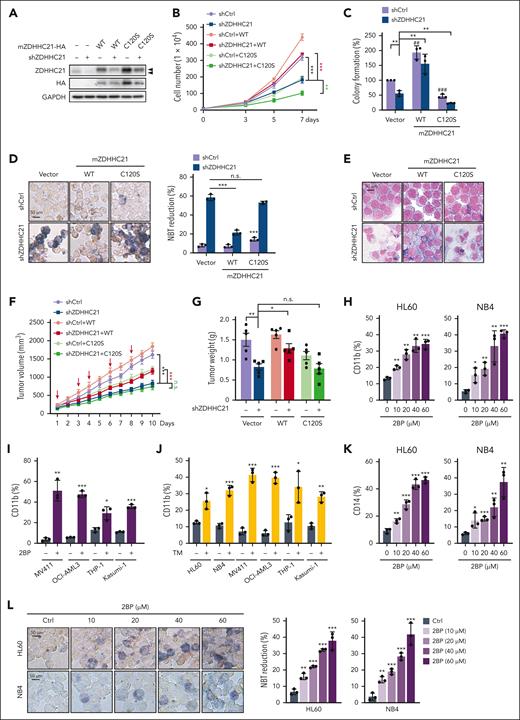
ZDHHC21-induced AML proliferation, stemness, and differentiation blockage depends on its palmitoyl acyltransferase activity
We wondered whether the regulatory effect of ZDHHC21 as a palmitoyltransferase on AML malignant progression is dependent on its enzymatic activity. First, we constructed murine ZDHHC21 (mZDHHC21) and its catalytically inactive mutant (C120S) and re-expressed them in ZDHHC21-knockdown cells (Figure 4A). As expected, shZDHHC21 obviously inhibited cell proliferation in AML cells, and mZDHHC21 overexpression but not mZDHHC21 (C120S) rescued the shZDHHC21-induced phenotype (Figure 4B; supplemental Figure 10A). Moreover, the colony formation ability in soft agar of AML cells suppressed by shZDHHC21 could be rescued by mZDHHC21 overexpression but not by mZDHHC21 (C120S) (Figure 4C; supplemental Figure 10B-C). Meanwhile, the differentiation effect induced by shZDHHC21 was obviously inhibited by reexpressing mZDHHC21 rather than mZDHHC21 (C120S) (Figure 4D-E; supplemental Figure 10D-E). More importantly, we determined the growth of these cells in vivo. Results showed that shZDHHC21 obviously inhibited tumor growth, which could be rescued by mZDHHC21 overexpression but not mZDHHC21(C120S) (Figure 4F-G). Thus, these results indicate that the palmitoyltransferase activity of ZDHHC21 is required for its regulatory function in AML cells.
ZDHHC21-induced AML proliferation, stemness, and differentiation blockage depends on its palmitoyl acyltransferase activity. (A) The protein levels of mZDHHC21 in shZDHHC21-transfected HL60 cells re-expressing mZDHHC21-HA or mZDHHC21(C120S)-HA. (B) Cell proliferation of shZDHHC21-transfected AML cells re-expressing mZDHHC21-HA or mZDHHC21(C120S)-HA in HL60 cells. (C) The colony-forming ability of HL60 cells after culturing in soft agar. (D-E) Differentiation analysis of shZDHHC21-transfected HL60 cells re-expressing mZDHHC21-HA or mZDHHC21-C120S-HA. (D) NBT-reducing activity. (E) Cell morphological analysis after Wright-Giemsa staining. (F-G) mZDHHC21 overexpression but not mZDHHC21 (C120S) rescued shZDHHC21-induced tumor growth arrest in the subcutaneous xenograft model. NB4 cells infected with vector, mZDHHC21, or mZDHHC21 (C120S) were injected subcutaneously into 4- to 5-week-old female NSG mice and then received an intratumoral injection of virus containing shCtrl or shZDHHC21. (F) Tumor growth of NB4 xenografts. Tumor volume growth curves are presented as the mean ± SE, n = 5. The red arrow indicates the time of intratumoral injection. (G) Tumor weight of each group. (H-I) Cell differentiation analysis of AML cells treated with 2BP for 3 days. (H) CD11b expression of HL60 cells and NB4 cells treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM). (I) CD11b expression of other AML cell lines treated with 2BP at a single concentration. MV411 (40 μM), OCI-AML3 (60 μM), THP-1 (60 μM), and Kasumi-1 (60 μM). (J) CD11b expression of AML cells treated with TM by a single concentration. HL60 (1 μg/mL), NB4 (0.03125 μg/mL), MV411 (0.25 μg/mL), OCI-AML3 (1 μg/mL), THP-1 (0.125 μg/mL), and Kasumi-1 (0.0625 μg/mL). (K) CD14 expression of HL60 and NB4 cells treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM). (L) NBT-reducing activity of HL60 cells and NB4 cells treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM). Data are shown as mean ± SD, n = 3. n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or a one-way analysis of variance. WT, wild-type.
ZDHHC21-induced AML proliferation, stemness, and differentiation blockage depends on its palmitoyl acyltransferase activity. (A) The protein levels of mZDHHC21 in shZDHHC21-transfected HL60 cells re-expressing mZDHHC21-HA or mZDHHC21(C120S)-HA. (B) Cell proliferation of shZDHHC21-transfected AML cells re-expressing mZDHHC21-HA or mZDHHC21(C120S)-HA in HL60 cells. (C) The colony-forming ability of HL60 cells after culturing in soft agar. (D-E) Differentiation analysis of shZDHHC21-transfected HL60 cells re-expressing mZDHHC21-HA or mZDHHC21-C120S-HA. (D) NBT-reducing activity. (E) Cell morphological analysis after Wright-Giemsa staining. (F-G) mZDHHC21 overexpression but not mZDHHC21 (C120S) rescued shZDHHC21-induced tumor growth arrest in the subcutaneous xenograft model. NB4 cells infected with vector, mZDHHC21, or mZDHHC21 (C120S) were injected subcutaneously into 4- to 5-week-old female NSG mice and then received an intratumoral injection of virus containing shCtrl or shZDHHC21. (F) Tumor growth of NB4 xenografts. Tumor volume growth curves are presented as the mean ± SE, n = 5. The red arrow indicates the time of intratumoral injection. (G) Tumor weight of each group. (H-I) Cell differentiation analysis of AML cells treated with 2BP for 3 days. (H) CD11b expression of HL60 cells and NB4 cells treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM). (I) CD11b expression of other AML cell lines treated with 2BP at a single concentration. MV411 (40 μM), OCI-AML3 (60 μM), THP-1 (60 μM), and Kasumi-1 (60 μM). (J) CD11b expression of AML cells treated with TM by a single concentration. HL60 (1 μg/mL), NB4 (0.03125 μg/mL), MV411 (0.25 μg/mL), OCI-AML3 (1 μg/mL), THP-1 (0.125 μg/mL), and Kasumi-1 (0.0625 μg/mL). (K) CD14 expression of HL60 and NB4 cells treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM). (L) NBT-reducing activity of HL60 cells and NB4 cells treated with 2BP at a series of concentrations (0, 10, 20, 40, 60 μM). Data are shown as mean ± SD, n = 3. n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or a one-way analysis of variance. WT, wild-type.
Furthermore, 2BP covalently binds ZDHHC21 to inhibit its palmitoyltransferase activity, and therefore, we treated AML cells with 2BP to detect cell differentiation. Results showed that 2BP significantly upregulated CD11b expression in all AML cell lines (Figure 4H-I). A similar increase in CD11b expression was observed with another ZDHHC inhibitor, TM, but not the serine palmitoyltransferase inhibitor myriocin (Figure 4J; supplemental Figure 11A). Meanwhile, 2BP and TM rather than myriocin also dramatically enhanced CD14 expression (Figure 4K; supplemental Figure 11B-D). AML cells treated with 2BP also showed an enhanced NBT-reducing ability in a concentration-dependent manner (Figure 4L). Altogether, these results demonstrate that the regulation of AML cell proliferation, stemness, and differentiation by ZDHHC21 is dependent on its palmitoyltransferase activity.
ZDHHC21 palmitoylates mitochondrial kinase AK2 to regulate OXPHOS and AML progression
To further explore the mechanism involved in ZDHHC21 palmitoyltransferase activity–regulated OXPHOS and AML progression, we sought to identify potential modified substrates palmitoylated by ZDHHC21 (supplemental Figure 12). In total, 45 proteins were identified that not only interacted with ZDHHC21 but also had their palmitoylation level downregulated by shZDHHC21 (Figure 5A; supplemental Table 4). We then analyzed the expression of these 45 proteins in patients with AML compared with normal bone marrow in 2 data sets (Figure 5B). Among them, AK2 was ranked in the top 5 most upregulated genes in both data sets (Figure 5C). AK2 plays a critical role in mitochondrial energy metabolism by catalyzing the reaction of adenosine 5′-monophosphate and ATP to form adenosine 5′-diphosphate.32,33 We speculate that ZDHHC21 might regulate OXPHOS by directly facilitating AK2 palmitoylation. First, the physical interaction between ZDHHC21 and AK2 was validated (Figure 5D; supplemental Figure 13A). AK2 could be palmitoylated (supplemental Figure 13B), which was inhibited when all 4 cysteines were mutated (Figure 5E), suggesting that AK2 was S-palmitoylated. Moreover, ZDHHC21 obviously increased the palmitoylation of AK2, whereas ZDHHC21 (C120S) failed (Figure 5F). In addition, 2BP also significantly decreased AK2 palmitoylation (supplemental Figure 13C). Thus, these results indicate that ZDHHC21 is the palmitoyltransferase that regulates AK2 palmitoylation.
Palmitoylation can regulate the membrane localization of substrates; thus, we investigated the effect of AK2 palmitoylation on its cellular localization. AK2 was highly colocalized in the mitochondria, whereas palmitoylation-deficient mutants (AK2-4CS) showed a significantly lower extent (Figure 5G). shZDHHC21 also inhibited the mitochondrial localization of AK2 (Figure 5H; supplemental Figure 14). As expected, OXPHOS was significantly reduced in AK2-knockdown cells (Figure 5I; supplemental Figure 15A-C), whereas glycolysis level was not influenced (supplemental Figure 15D-E). Next, similar to shZDHHC21, shAK2 strongly increased CD11b expression (Figure 5J), enhanced NBT-reducing ability (Figure 5K), and induced cell cycle arrest (supplemental Figure 16) as well as cell apoptosis (supplemental Figure 17). Meanwhile, RNA sequencing analysis showed that the genetic changes in shZDHHC21 and shAK2 were highly similar, and the OXPHOS signature was enriched in the shCtrl group, whereas myeloid differentiation genes were enriched in the shZDHHC21 and shAK2 groups (supplemental Figure 18A-B). In addition, myeloid differentiation–related transcription factors, especially those transcription factors regulating terminal differentiation (eg, MAFB, EGR2), were increased by shZDHHC21 or shAK2 (supplemental Figure 18C). More importantly, AK2 overexpression rescued the decline of OXPHOS-mediated by shZDHHC21 (Figure 5L; supplemental Figure 19), and obviously inhibited shZDHHC21-induced differentiation (Figure 5M). Taken together, these data strongly support the hypothesis that ZDHHC21 mediates the palmitoylation and mitochondrial localization of AK2, which further leads to OXPHOS hyperactivity and differentiation blockage in AML cells.
shZDHHC21 exhibits strong therapeutic effect in AML and prolongs the survival of leukemic mice
To assess whether the antileukemic effects of shZDHHC21 could be reproduced in vivo, we first intravenously transplanted HL60-shCtrl or HL60-shZDHHC21 cells into NOD/SCID mice. The overall leukemic burden (Figure 6A; supplemental Figure 20A) and body weight loss due to leukemogenesis (Figure 6B) were significantly inhibited by shZDHHC21. The overall survival was significantly longer in mice that underwent transplantation with shZDHHC21 cells than with shCtrl cells (Figure 6C). Next, we evaluated the antitumor activity of ZDHHC21 inhibition in HL60 subcutaneous xenograft mouse models. The shZDHHC21-lentivirus significantly suppressed tumor growth and reduced tumor weight (Figure 6D-E). shZDHHC21 displayed obvious therapeutic activity, and no apparent body weight loss was observed (supplemental Figure 20B-C). Moreover, CD11b and CD14 expression in HL60-shZDHHC21 cell–derived xenografts was upregulated compared with the shCtrl group (Figure 6F). Finally, we used the doxycycline (DOX)-inducible Tet-on system to confirm the therapeutic effect of shZDHHC21. DOX significantly decreased the ZDHHC21 level in HL60 cells transduced with Tet-on shZDHHC21 (Figure 6G). The overall leukemic burden in the DOX diet group was significantly decreased (Figure 6H), and body weight loss was also weakened (Figure 6I). Meanwhile, mice fed with DOX prolonged the survival time of leukemic mice (Figure 6J). Collectively, these results demonstrate that targeting ZDHHC21 exhibits a strong therapeutic effect on AML in vivo.
Then, we further evaluated the therapeutic potential of ZDHHC21 inhibition in primary AML blasts using patient-derived cells (PDC) and patient derived xenograft (PDX) models. First, AML blasts with high expression of ZDHHC21 obtained higher ATP levels (Figure 6K). Next, CD11b expression was upregulated by shZDHHC21 in all human AML specimens (Figure 6L; supplemental Figure 21), and there was a positive correlation between ZDHHC21 expression and the differentiation sensitivity of AML cells (Figure 6M). Moreover, the primary AML blasts with the FLT3-ITD mutation were slightly more sensitive to shZDHHC21-induced differentiation (Figure 6N). These results indicate that shZDHHC21 inhibits primary AML cells with multiple genotypes, and the therapeutic effect might be more obvious in patients with AML with the FLT3-ITD mutation. In addition, patients with co-high expression of ZDHHC21 and AK2 showed the worst prognoses with the lowest survival time among all groups (Figure 6O). Thus, we validated the antileukemic effects of ZDHHC21 inhibition in a PDX-AML xenograft model and found that shZDHHC21 significantly prolonged the survival of leukemic mice (Figure 6P). Taken together, these results further support that targeting ZDHHC21 to inhibit OXPHOS might be a promising therapeutic strategy for patients with AML, especially those with the FLT3-ITD mutation.
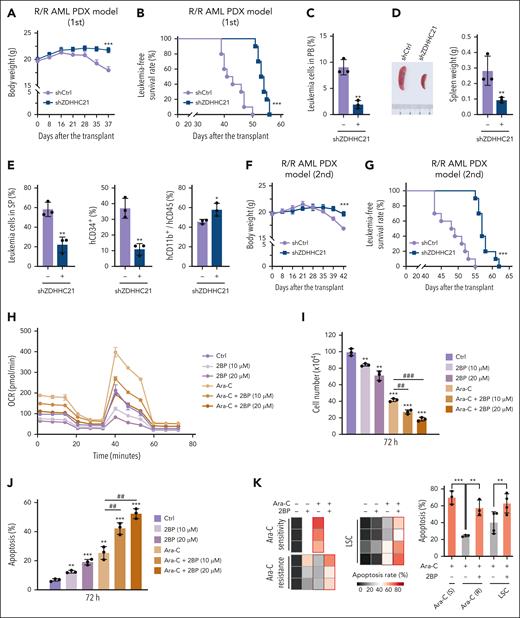
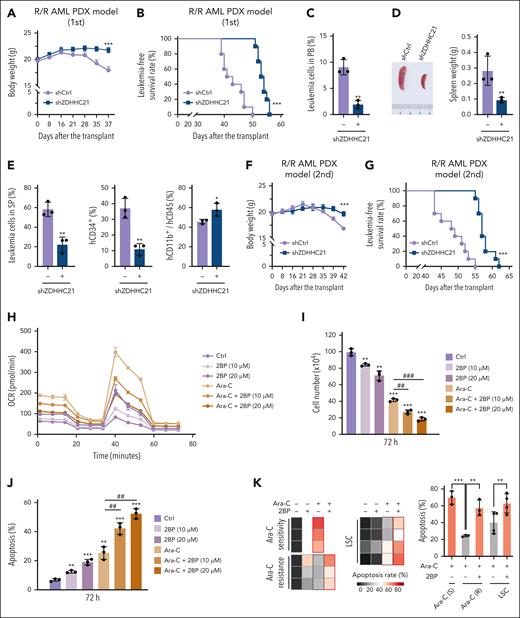
Targeting ZDHHC21 is a potential therapeutic strategy for relapsed/refractory AML
Because ZDHHC21 can regulate LSC maintenance and chemotherapy resistance, we wonder whether targeting ZDHHC21 would be able to treat relapsed/refractory AML. First, we evaluated the effect of ZDHHC21 inhibition in a relapsed/refractory PDX-AML xenograft model. AML blasts were separated from a patient with relapsed/refractory AML harboring the FLT3-ITD, and shCtrl or shZDHHC21 lentivirus–infected blasts were transplanted into NSG mice. Transplantation of blasts infected with shCtrl virus resulted in significant body weight loss after 28 days due to leukemogenesis, whereas the shZDHHC21 group did not (Figure 7A). Notably, the overall survival time was obviously prolonged in the shZDHHC21 group (Figure 7B). Consistently, the shZDHHC21 group exhibited a much lower leukemic engraftment level (Figure 7C) as well as a lower spleen weight (Figure 7D). Moreover, cells extracted from the spleen showed a decreased proportion of CD34+ cells, and CD11b expression of leukemic cells in the shZDHHC21 group was higher than that in the shCtrl group (Figure 7E). Furthermore, ZDHHC21 depletion also obviously delayed leukemia progression in the secondary recipients (Figure 7F-G), indicating that shZDHHC21 may have an inhibitory effect on AML recurrence.
Targeting ZDHHC21 is a potential therapeutic strategy for relapsed/refractory AML. (A-G) The in vivo effect of ZDHHC21 depletion on leukemogenesis in R/R PDX-AML xenograft model subjected to primary and secondary transplant. NSG mice underwent transplantation with shCtrl or shZDHHC21-transfected AML blasts. (A) Body weight of NSG mice. (B) The survival time of NSG mice. Data are presented as mean ± SD (n = 10). ∗∗∗P < .001 vs shCtrl. The significance analysis was conducted by log-rank test. (C) The population of hCD45+mCD45− leukemia cells in the peripheral blood of NSG mice. (D) Spleen weight of NSG mice on 39 days after transplantation (mean ±SD; n = 3). (E) The population of hCD45+mCD45− leukemia cells and CD34+ and CD11b+ cells in the spleen (SP) of NSG mice (mean± SD; n = 3). (F) The body weight of secondary transplant mice. (G) Kaplan-Meier survival curves of secondary transplant mice upon ZDHHC21 knockdown (n = 10). ∗∗∗P < .001 vs shCtrl. The significance analysis was conducted by log-rank test. (H) Mitochondrial OCR of HL60 cells after treatment with control, 2BP, Ara-C, or Ara-C + 2BP for 24 hours. OCR was assessed using a Seahorse analyzer. (I) The effect of 2BP, Ara-C, or Ara-C + 2BP on the proliferation of HL60 cells. HL60 cells were treated with drugs for 72 hours, followed by trypan blue exclusion test. (J) The effect of 2BP, Ara-C, or Ara-C + 2BP on the apoptosis of HL60 cells for 72 hours. The apoptosis was confirmed by PI/annexin V assay. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001 vs Ctrl. #P <.05; ##P < .01; ###P < .001 vs Ara-C. (K) The effect of Ara-C or Ara-C + 2BP on the apoptosis of primary AML blast cells and LSCs. Primary AML blast cells were directly separated from the bone marrow of patients using lymphocyte monocytes separation medium. LSCs were sorted by CD34 marker from AML specimens. The apoptosis rate of cells was detected after treatment with drug for 3 days. ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or a one-way analysis of variance.
Targeting ZDHHC21 is a potential therapeutic strategy for relapsed/refractory AML. (A-G) The in vivo effect of ZDHHC21 depletion on leukemogenesis in R/R PDX-AML xenograft model subjected to primary and secondary transplant. NSG mice underwent transplantation with shCtrl or shZDHHC21-transfected AML blasts. (A) Body weight of NSG mice. (B) The survival time of NSG mice. Data are presented as mean ± SD (n = 10). ∗∗∗P < .001 vs shCtrl. The significance analysis was conducted by log-rank test. (C) The population of hCD45+mCD45− leukemia cells in the peripheral blood of NSG mice. (D) Spleen weight of NSG mice on 39 days after transplantation (mean ±SD; n = 3). (E) The population of hCD45+mCD45− leukemia cells and CD34+ and CD11b+ cells in the spleen (SP) of NSG mice (mean± SD; n = 3). (F) The body weight of secondary transplant mice. (G) Kaplan-Meier survival curves of secondary transplant mice upon ZDHHC21 knockdown (n = 10). ∗∗∗P < .001 vs shCtrl. The significance analysis was conducted by log-rank test. (H) Mitochondrial OCR of HL60 cells after treatment with control, 2BP, Ara-C, or Ara-C + 2BP for 24 hours. OCR was assessed using a Seahorse analyzer. (I) The effect of 2BP, Ara-C, or Ara-C + 2BP on the proliferation of HL60 cells. HL60 cells were treated with drugs for 72 hours, followed by trypan blue exclusion test. (J) The effect of 2BP, Ara-C, or Ara-C + 2BP on the apoptosis of HL60 cells for 72 hours. The apoptosis was confirmed by PI/annexin V assay. Data are presented as mean ± SD (n = 3). n.s., P > .05; ∗P < .05; ∗∗P < .01; ∗∗∗P < .001 vs Ctrl. #P <.05; ##P < .01; ###P < .001 vs Ara-C. (K) The effect of Ara-C or Ara-C + 2BP on the apoptosis of primary AML blast cells and LSCs. Primary AML blast cells were directly separated from the bone marrow of patients using lymphocyte monocytes separation medium. LSCs were sorted by CD34 marker from AML specimens. The apoptosis rate of cells was detected after treatment with drug for 3 days. ∗∗P < .01; ∗∗∗P < .001. The significance analysis was conducted by a two-tailed unpaired t test or a one-way analysis of variance.
Chemotherapy-resistant AML cells, such as those resistant to cytarabine (Ara-C), exhibit metabolic features consistent with a high OXPHOS status.7 Thus, we sought to determine whether targeting ZDHHC21 could inhibit Ara-C–triggered OXPHOS hyperactivity and sensitize AML cells, especially relapsed/refractory cells, to chemotherapy. First, Ara-C induced a significant increase in OCR, whereas 2BP strongly suppressed OXPHOS in Ara-C–exposed AML cells (Figure 7H; supplemental Figure 22A). Meanwhile, no obvious apoptosis or ECAR changes were observed under this condition (supplemental Figure 22B-D). Moreover, 2BP-treated AML cells were more sensitive to Ara-C than vehicle-treated AML cells, as evidenced by the reduction of cell number (Figure 7I) and enhanced proportion of apoptotic cells (Figure 7J). To further confirm the potential sensitizing effect of 2BP on chemotherapy in the clinic, we isolated primary AML blasts from 3 drug-sensitive and 3 refractory patients. Compared with drug-sensitive samples, Ara-C failed to induce obvious apoptosis in refractory blasts. By contrast, 2BP significantly enhanced Ara-C–triggered apoptosis, promoting refractory blast resensitization to Ara-C. Moreover, 2BP also enhanced the apoptosis triggered by Ara-C in LSCs (Figure 7K). Taken together, these results strongly suggest that ZDHHC21 is a promising target for relapsed/refractory AML.
Discussion
AML is highly dependent on enhanced mitochondrion-specific OXPHOS.9,34-36 Specifically, LSCs and chemoresistant cells display increased mitochondrial mass and retain actively polarized mitochondria.7,8 Thus, more attention is being paid to the therapeutic vulnerability of OXPHOS in leukemic cells.11 However, the mechanisms promoting OXPHOS hyperactivity in AML have not been fully elucidated. Here, we first indicate that highly expressed ZDHHC21 is responsible for OXPHOS hyperactivity by palmitoylating AK2 in AML cells. In terms of clinical potential, targeting ZDHHC21 can eradicate leukemic blasts in multiple subtypes of AML and seems particularly active in patients with FLT3-ITD AML, although this requires further validation. In addition, the relatively high ZDHHC21 expression in AML cells with the NPM1 mutation may also lead to a better response, which needs further study. More importantly, ZDHHC21 is also a promising target for relapsed/refractory leukemia.
Palmitoylation has been well described to ensure the cell membrane tethering of proteins such as NRAS,15 FAS,37 STAT3,38 I-Smads,39 and PD-L1,40,41 as well as the mitochondrial localization of proteins such as BAX.42 Here, we find that AK2 is palmitoylated by ZDHHC21, which is essential for its mitochondrial localization. Moreover, our MS-based systematic analysis showed that ZDHHC21 might also have other mitochondrial proteins as its substrates, including NDUFB10, TFAM, NDUFA13, ETFB, and PGLS, all of which are linked to OXPHOS. Because the rescuing effect of AK2 overexpression was not complete, the effect of ZDHHC21 on other mitochondrial proteins warrants further investigation. In addition, ZDHHC13-dependent palmitoylation is crucial for mitochondrial fission,43 which is consistent with our results that siZDHHC13 obviously decreased OXPHOS both in AML cells and HSCs. We found that siZDHHC12, siZDHHC14, and siZDHHC15 can inhibit ATP production in AML cells and HSCs, suggesting that they may also be responsible for basic OXPHOS.
The differentiation of HSCs is driven by a switch from glycolysis to OXPHOS.44-47 Combined with our results, it seems that the role of OXPHOS in AML differentiation is different from that in HSCs. We hypothesize that OXPHOS activity is enhanced when HSCs differentiate into stem progenitor cells, whereas a decrease occurs when HSCs further differentiate into terminal myeloid cells. This phenomenon was also shown by Inoue et al.48 We also observed that ZDHHC21 was obviously decreased in the later stage rather than the early stage of myeloid differentiation. Transcription factors regulating terminal differentiation were specifically upregulated after ZDHHC21 depletion. This phenomenon suggests that the decline of OXPHOS might be an important force driving terminal myeloid differentiation. Certainly, the role of OXPHOS in different stages of the HSC differentiation process is worth further investigation. Additionally, retinoic acid receptor alpha (RARα) is a critical transcriptional factor of myeloid differentiation. Lu et al proposed that 2BP covalently binds and stabilizes RARα protein to further promote ATRA-induced differentiation.49 Thus, we wondered whether RARα participates in ZDHHC21 inhibition–induced differentiation. We found that RARα could undergo palmitoylation, but ZDHHC21 was not its palmitoyltransferase (data not shown). However, our RNA sequencing analysis showed that the target genes of RARα were upregulated by shZDHHC21. Thus, the role of RARα in ZDHHC21 inhibition–induced differentiation is very complicated and requires further investigation.
Palmitoyltransferases play important roles in various cancers. Ersoz et al demonstrated that the serine palmitoyltransferase inhibitor myriocin combined with resveratrol inhibited FLT3-ITD AML.50 We found that OXPHOS and differentiation-regulatory effects were observed with 2 ZDHHC inhibitors rather than myriocin, suggesting that the ZDHHCs play an essential role in AML. Several ZDHHCs are reported to be involved in leukemogenesis, including ZDHHC951 and ZDHHC14,52 but there is no systematic study on the relationship between ZDHHCs family and leukemia. Here, we comprehensively analyzed the potential role of all ZDHHCs in AML and identified ZDHHC21 as a key factor in regulating myeloid differentiation. Several ZDHHCs are reported to be associated with neuronal differentiation53,54 and TH17 cell differentiation.38 To our knowledge, our study is the first to provide intriguing data revealing ZDHHC21 as a regulator of AML differentiation blockage.
In summary, we have demonstrated for the first time that the energy advantage of AML cells is acquired via ZDHHC21-mediated activation of mitochondrial metabolism. Depletion of ZDHHC21 can induce myeloid differentiation in AML cells, especially FLT3-ITD–mutated leukemic cells, and eradicate leukemic blasts in relapsed/refractory AML. This study not only directs us toward the genetic landscape of OXPHOS dependency in AML but also provides fresh insights into the design of new therapies targeting differentiation in leukemia.
Acknowledgments
The authors thank Lingtao Wu at the University of Southern California for the kind donation of the NB4 cell line. The authors also thank Yueting Xing from the Core Facilities, Zhejiang University School of Medicine, and Dan Wu and Jianyang Pan from the Research and Service Center, Zhejiang University College of Pharmaceutical Sciences for their technical support.
This work was financially supported by grants from the National Natural Science Foundation of China (No. 81973354 to M.Y.), Zhejiang Provincial Natural Science Foundation of China (No. LY22H310005 to X.S.), the Natural Science Fund for Distinguished Young Scholars of Zhejiang Province (No. LR23H310001 to M.Y.), and the Fundamental Research Funds for the Central Universities.
Authorship
Contribution: M.Y. and X.S. conceived the study and analyzed data; X.S. and A.X. performed RNA sequencing and MS assay; A.X., M.C., Z.X., Y.H., J.Z., and X.Z. performed the immunofluorescence and western blotting procedure; A.X., X.S., W.D., Z.X., W.W., T.X., J.Z., and X.Z. detected the differentiation effect; X.S., A.X., W.D., Y.H., J.Z., Z.X., and M.C. performed animal studies; X.S., A.X., and Y.H. performed the OCR and ECAR assay; X.X. provided clinical AML samples and collected patient information; X.S., A.X., M.C., W.D., W.W., X.Z., and Z.X. obtained data from patients with leukemia; J.C., Q.H., and B.Y. conceived the experiments and helped organize the paper; and M.Y., X.S., and A.X. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Meidan Ying, Rm 115, Institute of Pharmacology and Toxicology, College of Pharmaceutical Sciences, Zhejiang University, Hangzhou 310058, China; e-mail: mying@zju.edu.cn.
References
Author notes
∗X.S. and A.X. contributed equally to this work.
Raw data for RNA sequencing are deposited at the National Center for Biotechnology Information Gene Expression Omnibus database (accession number GSE218229).
For more additional data related to this subject, please contact the corresponding author, Meidan Ying (mying@zju.edu.cn).
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.