Background: Equecabtagene autoleucel (eque-cel, CT103A), which is designed with a fully human BCMA-specific CAR structure, was recently granted NMPA approval for the treatment of adult patients (pts) with relapsed/refractory multiple myeloma (RRMM) after ≥3 prior lines of therapy (LOT). The pivotal phase 2 FUMANBA-1 study (NCT05066646) demonstrated deep and durable responses with eque-cel in heavily pretreated patients with RRMM. Recent studies have demonstrated the utility of minimal residual disease (MRD) as a prognostic biomarker for long-term outcomes of RRMM, wherein achievement of sustained MRD-negative status was associated with an improvement in PFS of pts treated by eque-cel in FUMANBA-1 study. We sought to characterize the baseline and disease characteristics of pts with sustained MRD negativity (pts who continued to remain MRD negative ≥6 mo and ≥12 mo).
Methods: FUMANBA-1 study enrolled RRMM pts who received ≥ 3 lines of prior therapies containing at least a proteasome inhibitor and an immunomodulatory agent and were refractory to their last line of treatment. All pts received a single infusion of eque-cel at the dose of 1.0 x 10 6 CAR-T cells/Kg. Pts who had progressed on previous BCMA CAR-T cell therapy were not included in this analysis. The primary endpoint was ORR. Additional endpoints included ≥CR rate (key secondary), DOR, PFS, and safety. ORR and CR were assessed per IMWG criteria; DOR and PFS were analyzed via Kaplan-Meier methods. MRD negativity was a secondary objective and was assessed on bone marrow samples at baseline; day 14, 28; and 2, 3, 6, 9, 12, 15, 18, 21 and 24 mo using EuroFlow next-generation flow, regardless of disease status. Evaluable samples passed calibration and quality control and included sufficient cells for evaluation at 10 -5 testing threshold. Characteristics were analyzed in pts who had MRD negativity <6 mo, or sustained ≥6 mo and ≥12 mo. Pts who did not achieve MRD negativity at any time point were considered to be MRD positive.
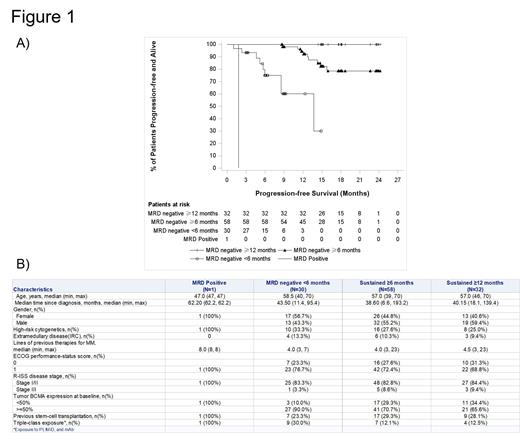
Results: Of the 88 pts who achieved MRD negativity in FUMANBA-1, 74 had at least 6 mo follow up without progression after initial MRD-negativity and 43 had at least 12 mo follow up without progression after initial MRD-negativity. MRD negativity was sustained for ≥6 mo in 78.4% (58 of 74 with at least 6 mo follow-up without progression after initial MRD-negativity) and ≥12 mo in 74.4% (32 of 43 with at least 12 mo follow-up without progression after initial MRD-negativity; 7 pts evaluable for sustained MRD at ≥6 mo but not ≥12 mo had PD). Pts with sustained MRD negativity (≥6 mo, and ≥12 mo) had longer progression free survival (PFS; Figure 1A) compared with pts who did not (MRD negative <6 mo). Key pt and disease characteristics in these different groups (Figure 1B), and potential associations with sustained MRD negativity were analyzed descriptively. Baseline R-ISS disease stage III was more common in pts with MRD sustained for ≥6 mo (8.6%) and ≥12 mo (9.4%) compared with pts who had MRD negativity <6 mo (3.3%). Baseline high tumor burden diseases were less common in pts with MRD sustained for ≥6 mo (70.7%) and ≥12 mo (65.6%) compared with pts who had MRD negativity <6 mo (90%). Triple-class exposure was also less common in pts with MRD sustained for ≥6 mo (12.1%) and ≥12 mo (12.5%) compared with pts who had MRD negativity <6 mo (30%). Pts with sustained MRD negativity had trends toward shorter median time since diagnosis (38.6 mo and 40.2 mo for pts with MRD negativity sustained ≥6 and ≥12 mo, respectively versus 43.5 mo for those with MRD negativity <6 mo). Other baseline characteristics, including presence of high-risk cytogenetics, ECOG performance status, extramedullary disease and number of prior LOT did not differ across MRD subgroups, and were similar to the overall FUMANBA-1 population.
Conclusions: Based on our descriptive analysis, pts receiving eque-cel achieved MRD negativity irrespective of their high-risk cytogenetics, extramedullary disease, number of prior LOT and performance status. Presence of high tumor burden at baseline, and prior triple-class exposure might be factors that impact achievement of sustained MRD negativity. These data suggest that while eque-cel is effective for a broad range of pts, specific pt and disease characteristics may be associated with sustained MRD negativity and better long-term outcomes. Sustained MRD negativity might be a promising prognostic indicator for RRMM pts treated by eque-cel.
Disclosures
Zhang:Nanjing IASO Biotherapeutics Ltd: Current Employment. Hu:Nanjing IASO Biotherapeutics Ltd: Current Employment. Wang:Nanjing IASO Biotherapeutics Ltd: Current Employment.