Abstract
The potential of hematopoietic stem cells (HSCs) from human immunodeficiency virus type-1 (HIV-1)–infected individuals, eg, self-renewal and multilineage differentiative capacity, might be perturbed due to the underlying disease. In this study, we assessed the HSC activity in the CD34+Thy-1+ cell population of peripheral blood stem cells (PBSCs) of three asymptomatic HIV-1–infected individuals after granulocyte colony-stimulating factor (G-CSF; 10 μg/kg/d) mobilization. On day 4 of G-CSF treatment, 0.8% to 1% of the total blood mononuclear cells were CD34+. Leukapheresis followed by a two-step cell isolation process yielded a CD34+Thy-1+ cell population of high purity (76% to 92% CD34+Thy-1+ cells). This cell population showed no evidence of HIV-1–containing cells based on a semiquantitative HIV-1 DNA polymerase chain reaction. Furthermore, the purified cells showed normal hematopoietic potential in in vitro clonogenic assays. Successful gene transfer into committed progenitor cells (colony-forming units-cells) and more primitive stem/progenitor cells (long-term culture colony-forming cells) could be shown after amphotropic retroviral transduction. These data provide evidence that the CD34+Thy-1+ stem cell compartment can be mobilized and enriched in early stage HIV-1–infected patients. Furthermore, successful transduction of this cell population as a prerequisite for stem cell-based clinical gene therapy protocols was demonstrated.
PERIPHERAL BLOOD stem cells (PBSCs) are currently being used for both autologous and allogeneic long-term hematopoietic reconstitution of cancer patients after myeloablation or chemoradiotherapy.1-4 The administration of chemotherapeutic agents and/or hematopoietic growth factors, such as granulocyte colony-stimulating factor (G-CSF ) mobilizes hematopoietic stem/progenitor cells in normal donors,5 cancer patients,6,7 and human immunodeficiency virus type-1 (HIV-1)–infected individuals.8 After G-CSF mobilization, PBSCs can then be procured by leukapheresis. Furthermore, transplantation of mobilized PBSCs is associated with shortened hematologic recovery times compared with bone marrow (BM) transplants.9,10 Within human blood mononuclear cells, a subpopulation of cells expresses the CD34 surface antigen (CD34+) exhibiting hematopoietic stem cell (HSC) characteristics.11-13 However, a more primitive HSC subset (CD34+Thy-1+Lin−) has been identified using long-term in vitro clonogenic assays and in vivo studies.14 This cell population is enriched in HSC activity capable of self-renewal and long-term multilineage differentiation15 16 and represents a subpopulation for autologous transplantation of PBSCs.
Gene therapy is a new treatment modality for a variety of genetic, neoplastic, or infectious diseases and has the potential to correct defects in all mature cells derived from gene-modified HSCs. In the case of HIV-1 infection, introduction of anti–HIV-1 gene constructs into HSCs might prevent acquired immunodeficiency syndrome (AIDS) pathogenesis17 in differentiated T lymphocytes, monocytes/macrophages, and dendritic and microglial cells. Several reports have described that BM CD34+ stem/progenitor cells are infected with HIV-1 at low frequencies in some patients.18-22 In contrast, one study concluded that, in individuals with advanced HIV-1 infection, up to 1 in 500 CD34+ cells is infected with HIV.23 Thus, hematopoietic stem/progenitor cells might be infected with HIV-1 and/or affected by the concurrent infection of BM stromal cells,24,25 resulting in the observed hematosuppression.26
The purpose of this study was to assess the in vitro clonogenic potential of mobilized PBSCs isolated from asymptomatic HIV-1–infected individuals and to assess retroviral-mediated gene transfer. Mobilization of PBSCs was achieved by G-CSF administration and the CD34+Thy-1+ subpopulation of HSCs was isolated after leukapheresis to high purity in a two-step isolation process. Our data support the notion that the CD34+Thy-1+ primitive hematopoietic cell population can be mobilized and enriched and is not adversely affected in early stage, asymptomatic HIV-1–infected patients. Furthermore, this cell population can be transduced with recombinant retroviral vectors supporting their clinical utility as autologous target cells for HSC-based gene therapies in HIV-1 disease.
MATERIALS AND METHODS
Patients.Written informed consent was obtained from all study participants as approved by the institutional review board of the City of Hope National Medical Center. Study participants were HIV-1 seropositive with CD4 counts of ≥200 cells/μL and no history of AIDS-related complex (ARC)/AIDS-defining illnesses, and two were receiving antiretroviral medication. Details on the clinical status of participants, mobilization regimen, leukapheresis procedure, and results of the mobilization and long-term follow-up will be published elsewhere (Zaia et al, manuscript in preparation).
Cell processing and fluorescence-activated cell sorting (FACS) analyses.One half of each apheresis product was shipped overnight at ambient temperature to Systemix (Palo Alto, CA). The CD34+ cell population was enriched by using a positive immunomagnetic separation device (Baxter, Santa Ana, CA) according to the manufacturer's protocol.27 Cell staining without the use of the lineage antibody panel and isolation of the CD34+Thy-1+ cell population by high-speed cell sorting (HSCS) was performed as described previously.16,28 29 During the purification process, cell samples were taken for cell count, viability testing, and FACS analysis. Cells for FACS analysis were fixed in phosphate-buffered saline/4% paraformaldehyde for 30 minutes on ice to inactivate HIV-1.
Transduction of CD34+Thy-1+ cells.The LMTNL (LTR-RevM10-TK-Neo-LTR) retroviral vector and the producer cell line PA317/LMTNL have been described previously.30,31 Retroviral titers were 3 × 106 G418-resistant colony-forming units (CFU)/mL as determined on NIH 3T3 cells. The producer cell line and vector supernatant tested negative for replication competent retrovirus (RCR) in extended S+L-assays using Mus dunni and PG-4 cells.32 Selected cells were cultured at 5 × 105/mL in Whitlock/Witte (W/W) medium (50% Iscove's modified Dulbecco's medium [IMDM], 50% RPMI-1640, 10% fetal calf serum, 4 × 10−5 mol/L 2-mercaptoethanol, 100 U/mL penicillin, 100 mg/mL streptomycin, and 4 mmol/L glutamine) supplemented with 20 ng/mL interleukin-3 (IL-3), 20 ng/mL IL-6, and 100 ng/mL stem cell factor (SCF ) at 37°C and 5% CO2 . IL-3, IL-6, and leukemia-inhibitory factor (LIF ) were provided by Sandoz Pharma (Basel, Switzerland). SCF was prepared at Systemix. Retroviral gene transfer was performed by incubating 5 × 105/mL cells in a 1:1 mixture of PA.LMTNL supernatant and W/W medium plus cytokines (IL-3, IL-6, and SCF or IL-3, IL-6, and LIF ) and 4 μg/mL of protamine sulfate for 4 hours on 3 consecutive days. The first transduction was performed after selected cells were obtained from the high-speed cell sorter. Mock transductions were performed with cells incubated in media plus growth factors (IL-3, IL-6, and LIF ) and protamine sulfate, but without retroviral supernatant. After the last supernatant inoculation, cells were washed and placed into the different assays.
Hematopoietic cell assays.For clonogenic progenitor cell analysis (colony-forming units-cells [CFU-C]), cells were resuspended in 5 mL IMDM supplemented with 10% fetal calf serum, 4 × 10−5 mol/L 2-mercaptoethanol, IL-3 (10 ng/mL), IL-6 (10 ng/mL), SCF (100 ng/mL), granulocyte-macrophage colony-stimulating factor (GM-CSF; 10 ng/mL; Immunex, Seattle, WA), erythropoietin (Epo; 2 U/mL; Amgen, Thousand Oaks, CA), 0.9% methylcellulose (MC; Stem Cell Technologies, Vancouver, British Columbia, Canada) and then plated into five bacterial-grade petri plates (750 or 2000 cells/mL/plate). After 2 weeks, colonies were counted and analyzed for the presence of transgene by neo-specific polymerase chain reaction (neo-PCR; see below). Long-term stromal cultures were used to evaluate stem cell potential and gene marking of more primitive progenitors. The long-term cobblestone area-forming cell (CAFC) assay was performed as described previously in the presence of IL-6 (10 ng/mL) and LIF (100 ng/mL).16 Cobblestone areas were counted at 5 weeks and the frequency of CAFC was calculated as described.16 Long-term culture colony-forming cell (LTC-CFC) assays were performed as follows. Briefly, 1 × 104 sorted and transduced cells were cultured in triplicate for 5 weeks on a pre-established monolayer of mouse stromal cells (Sys1)16 in media supplemented with IL-6 (10 ng/mL) and LIF (100 ng/mL). Plates were fed weekly by demi-depletion (ie, half of the medium was replaced with fresh medium). Long-term cultures were harvested at 5 weeks, and CFU-C colony assays were performed and analyzed as described above. All assays were also performed in the presence of 10 μmol/L azidothymidine (AZT; Sigma, St Louis, MO).
PCR and HIV-1 p24 analyses.For neo-PCR analysis, cell lysates were prepared from individual MC colonies. Cells were lysed in a buffer containing 50 mmol/L KCl, 10 mmol/L Tris, pH 8.3, 2.5 mmol/L MgCl2 , 1% Tween 20, 1% NP40, and 100 μg/mL proteinase K at 56°C for 2 hours. After lysis, samples were incubated for 15 minutes at 95°C to inactivate proteinase K. Neo-specific primers (N1, 5′-TCGACGTTGTCACTGAAGCG-3′; N2, 5′-GCTCTTCGTCCAGATCATCC-3′) were used to amplify the neomycin phosphotransferase gene and β-globin–specific primers (LA1, 5′-ACACAACTGTGTTCACTAGC-3′; LA2, 5′-CAACTTCATCCACGTTCACC-3′) were used to amplify the endogenous β-globin sequence as an internal control. Cells lysates were mixed with PCR buffer (Boehringer Mannheim, Indianapolis, IN), 200 mmol/L of dNTPs (Pharmacia, Piscataway, NJ), 25 pmol of Neo primers, 6.25 pmol of β-globin primers, and 1 U of Taq polymerase (Boehringer Mannheim). After denaturation (5 minutes at 94°C), the samples were submitted to 40 cycles of amplification: 30 seconds at 94°C, 30 seconds at 62°C, 1 minute at 72°C, and 10 minutes of elongation at 72°C in a thermocycler (Perkin Elmer 9600; Perkin-Elmer Cetus, Norwalk, CT). PCR products were analyzed by ethidium-bromide staining in 3% Nusieve/1% Seakam agarose gels.
For semiquantitative HIV-1 Gag DNA-PCR analysis, cell lysates were prepared from 1 × 104 (for CoH-3, 1 × 105) viable unfractionated, enriched, and sorted cells and subjected to PCR amplification as described above with the universal SK38 and SK39 Gag primers33 (Perkin Elmer) using the amplification conditions described above except for a 30-second ramp between denaturation and annealing. The annealing temperature was increased to 64°C. Defined mixtures of ACH-2 cells (containing 1 HIV-1 proviral copy)34 in the range of 1 to 1 × 104 (or 1 × 105) and CEM-SS cells (to bring the final cell number up to 1 × 104 or 1 × 105) were used to create a standard curve for the estimation of the HIV-1 proviral copy number in primary cells. PCR products were analyzed as described above.
HIV-1 p24 antigen in the apheresis sample or in tissue culture supernatant harvested at the end of the transduction period was determined using a commercially available enzyme-linked immunosorbent assay (ELISA) kit (Coulter, Hialeah, FL).
RESULTS
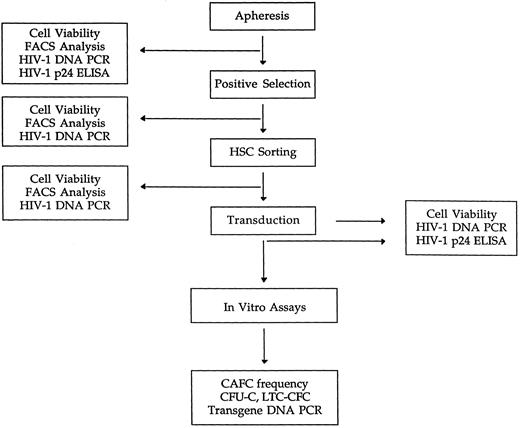
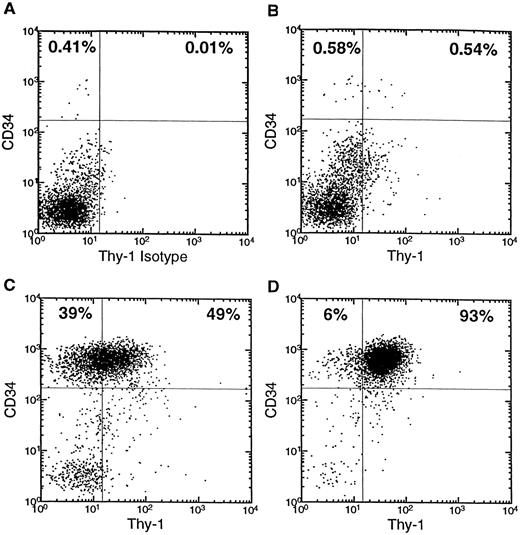
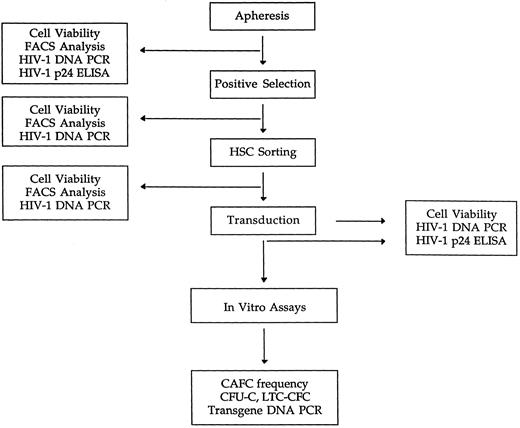
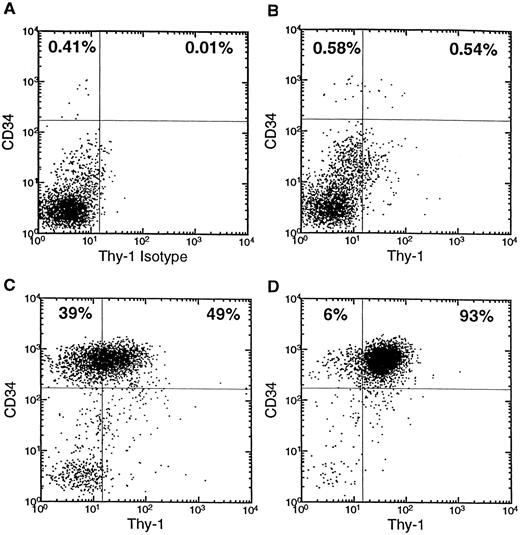
Purification of CD34+ and CD34+Thy-1+ cells from asymptomatic HIV-1 patients.Details on study participants are given in Table 1. Leukapheresis was performed on day 5 of G-CSF treatment (10 μg/kg/d). Figure 1 shows a flowchart depicting the purification steps, analyses, and assays performed with the apheresis products. The average number of viable cells in the leukapheresis samples received (n = 3) was 6.5 × 109 (range, 3.7 × 109 to 8.3 × 109) and the mean percentage of CD34+ cells in the apheresis product was 1.3% (range, 1.11% to 1.64%) compared with levels of CD34+ cells below the detection limit before G-CSF administration. The CD34+ cells were enriched using a positive immunomagnetic selection device27 and the mean percentage of CD34+ cells was 78.9% (range, 77.5% to 83.6%) after enrichment. The CD34+Thy-1+ subpopulation was 42.2% (range, 26.6% to 51.5%) of CD34+ cells. The CD34+Thy-1+ cell population was further enriched using an HSCS.29 After this step, the percentage of CD34+ cells was 90.6%, 94%, and 98.2% and the percentage of CD34+Thy-1+ cells was 76.2%, 90.1%, and 91.6% for tissue CoH-1, CoH-2, and CoH-3, respectively. The relative cell recovery after the CD34+ and CD34+Thy-1+ cell enrichment processes was 60% to 80% and 20% to 40%, respectively (data not shown). The cell viability was on average 71.6% (range, 38% to 93%) after HSCS. One tissue (CoH-1) showed low cell viability, which was most likely due to the storage and transportation conditions used. Figure 2 shows a representative FACS analysis of samples from each purification step of one tissue (CoH-3).
Flowchart depicting the sequence of purification steps, analyses, and assays performed with leukapheresis samples from asymptomatic HIV-1 –infected individuals.
Flowchart depicting the sequence of purification steps, analyses, and assays performed with leukapheresis samples from asymptomatic HIV-1 –infected individuals.
Flow cytometric analysis of cell fractions during the purification of CD34+Thy-1+ cells. CD34 versus Thy-1 expression is shown for lymphoblastoid-gated (by forward versus side scatter) cells. (A) Apheresis sample with isotype control for Thy-1. (B) Apheresis sample. (C) Reanalysis after CD34+ cell enrichment. (D) Reanalysis after HSCS. The percentage of CD34+ or CD34+Thy-1+ cells is given in the upper left or upper right quadrant of each panel, respectively.
Flow cytometric analysis of cell fractions during the purification of CD34+Thy-1+ cells. CD34 versus Thy-1 expression is shown for lymphoblastoid-gated (by forward versus side scatter) cells. (A) Apheresis sample with isotype control for Thy-1. (B) Apheresis sample. (C) Reanalysis after CD34+ cell enrichment. (D) Reanalysis after HSCS. The percentage of CD34+ or CD34+Thy-1+ cells is given in the upper left or upper right quadrant of each panel, respectively.
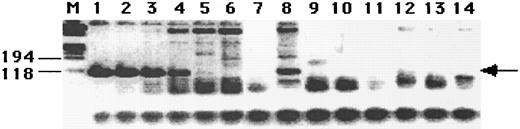
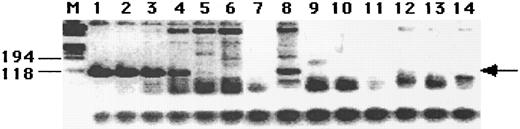
HIV-1 assays and transduction.To examine the amount of HIV-1–containing cells during this purification process, aliquots of the apheresis samples and postenrichment and post-HSCS cell fractions were PCR-amplified for HIV-1 gag-specific DNA sequences. For tissues CoH-1 and CoH-2, 1 × 104 cells were analyzed, and for tissue CoH-3, 1 × 105 cells were analyzed at each step and compared with an ACH2 (an A3.01 cell line containing 1 HIV-1 proviral copy)34 serial dilution standard. With a PCR assay sensitivity of detecting one HIV-1 proviral copy in a background of 1 × 104 or 1 × 105 uninfected cells, we detected approximately 10 proviral copies in all three apheresis samples (Fig 3 and Table 2). Figure 3 shows a representative DNA PCR analysis of CoH-1. However, we did not detect any Gag-specific signals in the immunomagnetic bead-enriched and HSCS-enriched cell fractions (Fig 3 and Table 2). Southern blot hybridization using a radiolabeled SK19 oligonucleotide probe did not increase the sensitivity of the PCR assay and did not show any additional signals (CoH-1, data not shown). The apheresis samples were also analyzed for HIV-1 p24 Gag antigen using a p24 ELISA kit. In all three tissues, p24 Gag antigen levels were below the detection limit (<5 pg/mL, Table 2).
Semiquantitative HIV-1 Gag DNA PCR analysis of cell aliquots during the purification course. Cells (1 × 104) from each purification step were PCR-amplified with the universal SK38 and SK39 Gag primers, and the signal intensity was compared with standards containing 1 × 104, 1 × 103, 1 × 102, 10, 1, and 0 ACH2 (A3.01 cell line containing one proviral copy of the HIV-1 genome) cells (lanes 1 through 6). Lane 7, negative control; lane 8, apheresis sample; lane 9, after CD34+ cell enrichment; lane 10, after HSCS; lane 11, negative control; lane 12, mock transduction; lane 13, LIF transduction; lane 14, SCF transduction; lane M, molecular weight marker (in basepairs). The arrow indicates the position of the 115-bp gag gene PCR product.
Semiquantitative HIV-1 Gag DNA PCR analysis of cell aliquots during the purification course. Cells (1 × 104) from each purification step were PCR-amplified with the universal SK38 and SK39 Gag primers, and the signal intensity was compared with standards containing 1 × 104, 1 × 103, 1 × 102, 10, 1, and 0 ACH2 (A3.01 cell line containing one proviral copy of the HIV-1 genome) cells (lanes 1 through 6). Lane 7, negative control; lane 8, apheresis sample; lane 9, after CD34+ cell enrichment; lane 10, after HSCS; lane 11, negative control; lane 12, mock transduction; lane 13, LIF transduction; lane 14, SCF transduction; lane M, molecular weight marker (in basepairs). The arrow indicates the position of the 115-bp gag gene PCR product.
Purified CD34+Thy-1+ cells were transduced on 3 consecutive days with cell-free supernatant containing the LMTNL30 retroviral vector packaged in the amphotropic packaging cell line PA31735 in the presence of IL-3, IL-6, and either LIF or SCF. To test for the possible activation of HIV-1 replication by this procedure, we analyzed cells at the end of the transduction period again by HIV-1 Gag DNA PCR. Cells from all three tissues and all transduction conditions again tested negative for the presence of the HIV-1 genome with the Gag-specific DNA PCR (Fig 3 and Table 2). HIV-1 p24 antigen levels in tissue culture supernatants harvested at the end of the transduction period were again below the detection limit of the p24 ELISA (Table 2).
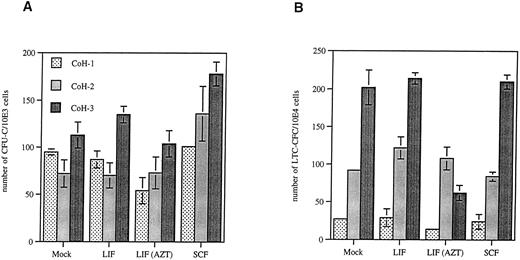
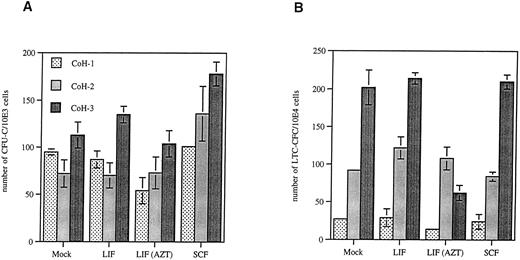
In vitro hematobiologic assays.After transduction, cells were placed into various short and long-term in vitro clonogenic assays. Enriched, transduced cells were plated into MC colony assays. CD34+Thy-1+ cells from HIV+ patients (n = 3) yielded a mean ± SD of 93 ± 21 day-14 CFU-C colonies (per 103 cells) in the mock transduction containing LIF, 97 ± 34 day-14 CFU-C colonies in the transduction containing LIF, and 138 ± 39 day-14 CFU-C colonies in the transduction containing SCF (Fig 4A). CD34+Thy-1+ cells transduced in the presence of LIF were also plated in methylcellulose containing AZT and yielded a mean ± SD of 77 ± 25 day-14 CFU-C colonies (Fig 4A).
Enumeration of colonies after cultivation of transduced CD34+Thy-1+ cells for 14 days in MC (CFU-C; A) or cultivation for 5 weeks on a mouse stromal cell line Sys1 followed by 14 days in MC (LTC-CFC; B). The number of CFU-C or LTC-CFC colonies is presented for 1 × 103 or 1 × 104 cells plated, respectively. The columns represent the mean values and the bars represent standard deviation of three independent enumerations. In some columns, the error bars cannot be plotted due to minimal data variation. Mock, transduction in the presence of IL-3, IL-6, and LIF but without viral supernatant; LIF, transduction in the presence of IL-3, IL-6, LIF, and viral supernatant; LIF (AZT), transduction in the presence of IL-3, IL-6, LIF, and viral supernatant and followed by cultivation of cells in MC or medium containing 10 μmol/L AZT; SCF, transduction in the presence of IL-3, IL-6, SCF, and viral supernatant.
Enumeration of colonies after cultivation of transduced CD34+Thy-1+ cells for 14 days in MC (CFU-C; A) or cultivation for 5 weeks on a mouse stromal cell line Sys1 followed by 14 days in MC (LTC-CFC; B). The number of CFU-C or LTC-CFC colonies is presented for 1 × 103 or 1 × 104 cells plated, respectively. The columns represent the mean values and the bars represent standard deviation of three independent enumerations. In some columns, the error bars cannot be plotted due to minimal data variation. Mock, transduction in the presence of IL-3, IL-6, and LIF but without viral supernatant; LIF, transduction in the presence of IL-3, IL-6, LIF, and viral supernatant; LIF (AZT), transduction in the presence of IL-3, IL-6, LIF, and viral supernatant and followed by cultivation of cells in MC or medium containing 10 μmol/L AZT; SCF, transduction in the presence of IL-3, IL-6, SCF, and viral supernatant.
To assess the number of long-term multipotent progenitor and stem cells, transduced CD34+Thy-1+ cells were cultured on a mouse stromal cell line Sys116 for 5 weeks, followed by plating the recovered nonadherent cells in MC for colony formation (LTC-CFC). Figure 4B shows that cells from the mock transduction containing LIF yielded a mean ± SD of 107 ± 88 day-14 LTC-CFC colonies (per 104 cells), from the transduction containing LIF 122 ± 93 colonies, and from the transduction containing SCF 106 ± 95 colonies. Cells from the transduction containing LIF were also cultured on the stromal cell line and in methylcellulose containing AZT and yielded a mean ± SD of 61 ± 47 day-14 LTC-CFC colonies (Fig 4B).
The long-term in vitro culture assay for CAFC was used to determine stem cell frequency. Mock-transduced CD34+Thy-1+ cells showed a CAFC frequency ranging from 1/20 to 1/10, whereas cells transduced in the presence of LIF or SCF ranged from 1/23 to 1/10 or 1/14 to 1/9, respectively (Table 3). Cells transduced in the presence of LIF and cultured on Sys1 stromal cells with AZT showed a CAFC frequency ranging from 1/22 to 1/11 (Table 3).
Retroviral gene marking.To determine the transduction efficiency, colonies of committed progenitor cells (CFU-C) were analyzed for the presence of the neo (neomycin phosphotransferase ) transgene by DNA PCR. On average, 4% or 5% (range, 3% to 4% or 2% to 8%) of colonies derived from transduced CD34+Thy-1+ cells in the presence of LIF or SCF, respectively, carried the neo-transgene (Table 4). CFU-C colonies grown in the presence of AZT carried the neo-transgene in 2% (range, 1% to 2%; Table 4). Long-term cultures (LTC-CFC) were used to determine the gene marking of multipotent progenitor and stem cells. On average, LTC-CFC colonies were gene marked 4% or 2% (range, 2% to 6% or 1% to 3%), depending on whether the transduction was performed in the presence of LIF or SCF, respectively (Table 4). Transduced progenitor cells cultured with mouse Sys1 stromal cells and AZT followed by MC culture containing AZT carried the neo-transgene on average in 2% (range, 2% to 3%) of colonies analyzed (Table 4).
DISCUSSION
In this study, we showed for the first time purification of a primitive CD34+Thy-1+ HSC-enriched cell population15 from cytokine-mobilized PBSCs of early stage, asymptomatic HIV-1–infected individuals. We did not detect HIV-1 proviral DNA sequences in any of the CD34+Thy-1+ cell samples using a DNA PCR assay with a sensitivity of detecting one proviral copy in the background of 1 × 104 or 1 × 105 uninfected cells. These results suggest that these cells are not infected in vivo or the infection rate is below the detection limit. Our results are in agreement with previous reports that used BM or G-CSF–mobilized CD34+ cells from HIV-1–seropositive patients at different disease stages and showed low levels of infection of CD34+ cells.8,18-22 Further evidence that only few CD34+ cells are infected by HIV-1 stems from in vitro experiments in which BM CD34+ cells were exposed to HIV-1. In this study, reselected CD34+ cells tested negative for HIV-1 infection and expression.36 CD34+Thy-1+ cells are more primitive than CD34+ cells and are highly enriched for lineage-negative cells and a better defined stem cell population. For these reasons, it is possible that this cell population is less susceptible to HIV-1 infection than CD34+ cells. Whether this also applies to HIV-1 patients with advanced disease awaits further investigation.
The hematopoietic potential of transduced CD34+Thy-1+ cells from HIV-1–infected individuals was analyzed in short-term and long-term in vitro assays. The number of clonogenic progenitors in short-term MC assays was comparable to the in vitro colony-forming potential of G-CSF –mobilized CD34+ and CD34+Thy-1+ cells obtained from healthy donors (I. Plavec and R. Tushinski, personal communication, September 1996). Previously, several reports described a decrease in the progenitor potential of BM CD34+ cells,20,21,37-41 whereas others found no evidence for suppression of the progenitor potential,42 even when CFU colonies were HIV-1 infected.43 However, most of those studies were performed with BM CD34+ cells obtained from HIV-1 patients with advanced disease (ARC/AIDS). More importantly, we also analyzed the hematopoietic potential in long-term in vitro assays. The frequency of CAFC is indicative of pluripotent stem cells and was within the range of previously reported CAFC frequencies for mobilized peripheral blood CD34+Thy-1+Lin− cells from healthy donors.29 We used an in vitro long-term culture assay (LTC-CFC) to examine the number of primitive stem/progenitor cells and obtained results comparable to the LTC-CFC potential of CD34+Thy-1+ cells from healthy donors (R. Tushinski, personal communication, September 1996). We did not find a statistical significant difference in the number of early and late progenitor colonies or the CAFC frequency of CD34+Thy-1+ cells cultured during the transduction period either with LIF or SCF. These assays were also performed in the presence of AZT, a nucleoside analogue inhibitor of the HIV-1 reverse transcriptase,44 because we wanted to suppress possible activation of latent HIV-1 infection occurring during the transduction period. However, the purified CD34+Thy-1+ cells did not contain detectable proviral HIV-1 DNA, and no HIV-1 reactivation during transduction was observed even in the absence of the antiretroviral drug. Nevertheless, the hematopoietic potential of CD34+Thy-1+ cells was not adversely affected by the concentration of AZT used in the short-term and long-term in vitro assays. Previously, it has been shown that peripheral blood CD34+Thy-1+Lin− cells can engraft and give rise to donor cells in the immunodeficient SCID-hu bone16,29 and SCID-hu thymus mouse models.16 In the future, it is important to address whether purified CD34+Thy-1+ cells from HIV-1–infected individuals still retain the T-lineage potential in the in vivo differentiation SCID-hu thymus model. In this setting, any latent HIV-1 proviruses would potentially be activated and result in detectable HIV-1 replication and destruction of the human thymic environment.45 Furthermore, a correlation of stem/progenitor cells reading out in in vitro assays and long-term SCID-repopulating cells could be studied in this model.46
Only a fraction of the leukapheresis product was available for this study and we could not address the question whether a sufficient number of CD34+Thy-1+ cells can be obtained to ensure engraftment in a clinical setting. Most likely, more gene-modified stem cells will result in higher levels of engraftment. At present, safe and effective conditioning regimens for infusion of gene-modified hematopoietic stem cells still need to be developed, in particular for HIV-1–infected individuals.
To assess retroviral gene marking in hematopoietic stem and progenitor cells, we analyzed individual colonies for the presence of retroviral vector DNA. Reproducible gene transfer was observed in progenitor cells and more primitive stem cells, varying from 1% to 8% and 1% to 6%, respectively, regardless of whether the transduction was performed in the presence of LIF or SCF (Table 4). The gene marking frequency of primitive stem/progenitor cells is not an absolutely quantitative result because the clonality of PCR-analyzed colonies was not assessed. However, detection of the neo-transgene in colonies isolated from long-term in vitro cultures is an indication that primitive hematopoietic stem/progenitor cells were transduced during the 3-day transduction period. The evaluation of gene expression in the progeny of transduced hematopoietic stem/progenitor cells was not performed in this study, but it was shown previously that transduction of cord blood derived stem/progenitor cells leads to marking and expression in progeny cells,47 resulting in inhibition of HIV-1 replication in myeloid cells.48 Another study demonstrated that CD34+ PBSCs isolated from G-CSF–mobilized HIV-1 individuals of the same study cohort studied in this report can be efficiently transduced with retroviral vectors encoding anti-HIV-1 genes.49 Furthermore, pronounced inhibition of HIV-1 replication was shown in primary monocytes derived from transduced CD34+ PBSCs after infection with clinical HIV-1 isolates.49 These results indicate that PBSCs (CD34+ and CD34+Thy-1+) from HIV-1–infected individuals perform similarly to PBSCs from healthy, normal donors, supporting the initiation of hematopoietic stem cell-based clinical trials for the treatment of HIV-1 infection.
ACKNOWLEDGMENT
We thank the staff at the Donor/Apheresis Center at City of Hope National Medical Center, in particular Dr James I. Ito for subject recruitment and Priscilla Yam for providing apheresis samples. We also thank our Systemix colleagues: Dave Adams for cell sorting, Charles Dowding for his advice with cell enrichment, Sean Forestell for providing vector supernatant, Robin Hastings for operational assistance with the FACS Vantage, Susan Nicholas for organizing sample shipments, Linda Osborne for maintenance of Sys1 cells, Ivan Plavec and Robert Tushinski for access to unpublished data, and Ben Chen and Richard J. Rigg for critical review of the manuscript. We are indebted to the patients who participated in this study. The Progenesys Program at Systemix is a Research and Development Collaboration jointly sponsored by Novartis and Systemix.
Address reprint requests to Ernst Böhnlein, PhD, Systemix Inc, 3155 Porter Dr, Palo Alto, CA 94304.