Abstract
Hereditary stomatocytosis is a red cell membrane protein disorder, which results in hemolytic anemia. Some patients with hereditary stomatocytosis experience dyspnea, chest pain, and abdominal pain, particularly after splenectomy. These symptoms may represent vaso-occlusion secondary to adherence of an abnormal erythrocyte membrane to vascular endothelium. We studied three members of a family with varying clinical expression of hereditary stomatocytosis. Adherence of red cells to endothelium was quantified by measuring the shear force required to separate individual cells from endothelial monolayers using a micropipette technique. Two patients with symptoms of in situ thromboses had a higher percentage of adherent cells compared with their asymptomatic sibling and normal controls. Correlation between this in vitro phenomenon and the clinical course suggests that flow abnormalities in the microcirculation attributable to erythrocyte endothelial adherence may play an important pathogenetic role in the illness. When the proportion of adherent red cells was reduced by a chronic transfusion program in one patient and pentoxifyllin therapy in another, the vaso-occlusive complications were eliminated.
HEREDITARY stomatocytosis is a heterogeneous group of congenital hemolytic anemias, characterized by red cells that have an oval shape and slit-like central pallor on a blood film.1-3 Studies in some families have revealed a deficiency in integral membrane protein 7.2b4-10 as well as abnormalities in cation permeability and intracellular cation concentration, which alter intracellular water content and cell morphology.11 12 These changes likely contribute to the shortened in vivo survival of stomatocytes. We describe abnormal red cell endothelial adherence in three members of a family with varying clinical expression of hereditary stomatocytosis. The percent of adherent cells appears to correlate with the severity of symptoms.
CASE REPORTS
J.W., E.M., and A.M. are siblings of Swiss-German ancestry whose paternal and maternal great-great grandmothers were sisters. The pedigree spanning 6 generations previously has been reported.13 J.W. was asymptomatic until age 5 in 1962, when she required hospital admission for profound anemia, which occurred after a respiratory infection. Her physical exam revealed hepatosplenomegaly, and laboratory evaluation included a hematocrit of 19% and a reticulocyte count of 31%. Subsequent evaluations revealed: persistent hepatosplenomegaly; chronic hematocrits of 30%, reticulocyte counts of 20%; blood films with 35% stomatocytes; negative direct and indirect coombs tests; normal hemoglobin electrophoresis; and negative tests for paroxysmal nocturnal and cold hemoglobinuria. Two siblings (E.M. and A.M.) were noted to have similar hematologic findings, and all were diagnosed with hereditary stomatocytosis.13
In 1970 at age 13, J.W. had her spleen removed to improve the red cell survival, but the procedure was not helpful and her anemia was not improved. Preoperative platelet count was 430,000/μL. Nine days after her splenectomy she had a laparotomy for a subdiaphragmatic hematoma and her platelet count was 3,826,000/μL. Three weeks later she had a third laparotomy for portal vein thrombosis with a platelet count of 1,101,000/μL. She was treated with aspirin, and 1 month later her platelet count was 1,236,000/μL. Over the next 4 years she remained asymptomatic with platelet counts ranging from 518,000/μL to 1,484,000/μL with a median platelet count of 1,225,000/μL. In 1974, she developed left shoulder pain exacerbated by deep inspiration. Her hematocrit was 27% with 15% reticulocytes and a platelet count of 1,340,000/μL. Pulmonary angiogram and lower extremity venograms were negative. Symptoms resolved and she was maintained with aspirin therapy.
J.W. had one pregnancy in 1977, which was managed with hypertransfusion and prophylactic subcutaneous heparin to minimize the risk of thrombotic complications. However, in her third trimester she had three admissions for painful crises. Two crises involved left lower extremity pain, and platelet counts were 774,000/μL and 440,000/μL, respectively, and a venogram was normal. The third crisis involved left sided abdominal pain, and the platelet count was 208,000/μL and an evaluation for thrombosis was unrevealing. Two weeks after delivery her platelet count returned to her baseline of 1,100,000. J.W. had multiple admissions over the next 3 years for severe abdominal pain or flank pain. Genitourinary (GU) and gastrointestinal (GI) evaluations were negative, and the pain was attributed to possible omental infarction. Platelet counts ranged from 1,380,000/μL to 1,560,000/μL.
At age 24 in 1981, J.W. had a series of pulmonary episodes initially thought to be pulmonary emboli because of positive ventilation-perfusion (VQ) scans and pulmonary arteriograms showing diffuse thrombi in small vessels. Platelet counts ranged from 960,000/μL to 1,110,000/μL. An extensive workup for a potential source of pulmonary emboli was unrevealing except for an echocardiogram, which showed a right ventricular mass that was subsequently removed surgically. This mass was a calcified blood clot in the chordae tendineae, but subsequent events indicated that it was not the source of emboli. Despite taking aspirin and warfarin or subcutaneous heparin, she continued during the next 2 years to have episodes of pulmonary compromise that were diagnosed as in situ pulmonary thromboses, and these episodes required multiple hospital admissions. Platelet counts ranged from 260,000/μL to 928,000/μL and there was no correlation between the height of the platelet count and the onset or severity of the episodes of dyspnea. Platelet function was normal, and protein C and S were normal, and antithrombin III was normal. During this same time period, she had several hospital admissions for severe abdominal pain, similar to sickle cell crises. Platelet counts ranged from normal to elevated. GI and GU evaluations were again normal, and the patient was thought to have in situ thromboses.
Since age 27, J.W. has been hypertransfused to minimize her erythrocyte production, and since that time she has had no further documented vascular events. Her platelet count has varied from 192,000/μL to 798,000/μL and her hematocrit has varied from 31% to 41% with reticulocyte counts of 0.1% to 4.5%. She continues taking warfarin with an international normalized ratio (INR) of 2.5, and she is hypertransfused with 2 U of packed red cells every 2 to 3 weeks. Iron overload has caused mild biventricular congestive heart failure and cardiac arrhythmias and has been treated with desferoxamine since 1985.
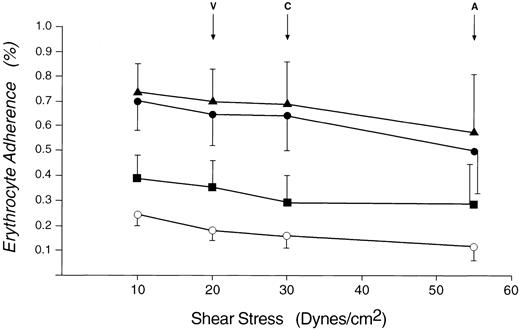
Mean percentage of erythrocytes that are adherent to cultured endothelial monolayers at various shear stresses. (▴), Patient A.M.; (•), patient J.W.; (▪), patient E.M.; (○), age- and sex-matched controls. V, maximum venule shear stress; C, maximum capillary shear stress; A, maximum arteriole shear stress.
Mean percentage of erythrocytes that are adherent to cultured endothelial monolayers at various shear stresses. (▴), Patient A.M.; (•), patient J.W.; (▪), patient E.M.; (○), age- and sex-matched controls. V, maximum venule shear stress; C, maximum capillary shear stress; A, maximum arteriole shear stress.
E.M. was admitted at age 4 in 1963 with pallor, hepatosplenomegaly, and anemia. His hematocrit was 12% and reticulocyte count 0%. He was transfused and given folic acid and recovered uneventfully. Subsequent hematological evaluation as part of a family study13 revealed a hematocrit of 27%, a reticulocyte count of 15% and blood film with 35% stomatocytes. He did well until 1992 when he noted increased fatigue after an infection. He was seen at his local hospital and given 2 U of packed red cells. Currently he is asymptomatic and working full-time. Physical examination is significant for splenomegaly with the spleen 4 cm below the left costal margin. His hematocrit is 22.5%, reticulocyte count 18.7%, and platelet count 244,000/μL.
A.M. had no childhood hospitalizations, but had intermittent episodes of pallor and icterus and had predictable fatigue with exercise. At age 7, in 1969, an enlarged spleen, 5 cm below the costal margin was noted. His hematocrit was 33%, reticulocyte count was 16.1%, and stomatocytes 21%, and he along with his siblings J.W. and E.M., was diagnosed with hereditary stomatocytosis.13
A.M. began noting progressive fatigue, shortness of breath, and arthralgias in 1991, and he has been unable to work since March 1993. In 1992, he was admitted with severe chest pain, but cardiac and pulmonary evaluations were normal. In 1993 he had increasing episodes of shortness of breath and was admitted to rule out pulmonary embolus when one of these episodes was witnessed by his primary medical doctor. The VQ scan was negative and symptoms resolved spontaneously. He also has noted intermittent episodes of abdominal pain, primarily localized to the left upper quadrant. Evaluation has been unrevealing except for persistent splenomegaly with the spleen palpable 4 cm below the left costal margin. His hematocrit has averaged 36.9% and reticulocyte count 18.9% and platelet count 226,000/μL. In March 1993 he was treated with low-dose pentoxifyllin, 400 mg/d, and although he continues to note fatigue and infrequent recurrences of abdominal discomfort, he has had no further episodes of acute shortness of breath or severe abdominal pain except on two occasions when he stopped taking the pentoxifylline. Symptoms, which persisted for 1 to 2 days, resolved when the pentoxifylline was restarted.
MATERIALS AND METHODS
Endothelial cell cultures.Veins from human umbilical cords were cannulated and infused with isotonic phosphate buffer to remove erythrocytes then filled with 15 mL of Collagenase 0.045 g/50 mL isotonic phospate buffer (Sigma, St Louis, MO) and incubated at 37°C for 10 minutes to loosen endothelial cells. The veins were flushed with phosphate buffer, and the endothelial cells collected, then mixed with Sigma medium 199 (Sigma) and 20% fetal calf serum (Sigma), E0760 endothelial cell growth supplement 30 μg/mL of culture media (Sigma) and 20 mL/L antibiotic/ antimycotic A9909 (Sigma). The cells were layered on 1-cm squares of glass. The culture medium was changed at 24- to 48-hour intervals until the endothelium formed a confluent monolayer.
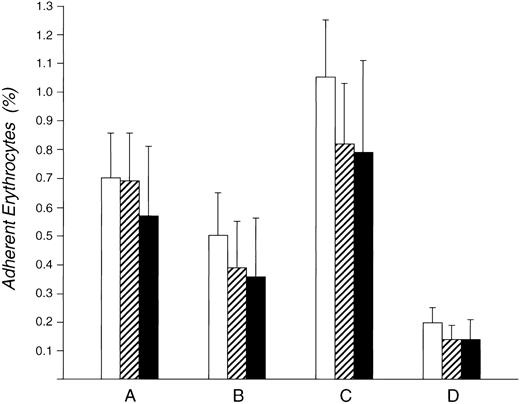
Sequential mean percent RBC adherence studies for patient AM at physiologic shear force in the microcirculation. (A) Initial 6 months corresponding to progressive symptoms. (B) While taking pentoxifylline for 2 years. (C) Two occasions when pentoxifylline was stopped. (D) Age and sex matched controls. (□), Percent adherent for shear stress of 20 dynes/cm2; (▨), percent adherent for shear stress of 30 dynes/cm2; (▪) percent adherent for shear stress of 55 dynes/cm2.
Sequential mean percent RBC adherence studies for patient AM at physiologic shear force in the microcirculation. (A) Initial 6 months corresponding to progressive symptoms. (B) While taking pentoxifylline for 2 years. (C) Two occasions when pentoxifylline was stopped. (D) Age and sex matched controls. (□), Percent adherent for shear stress of 20 dynes/cm2; (▨), percent adherent for shear stress of 30 dynes/cm2; (▪) percent adherent for shear stress of 55 dynes/cm2.
Erythrocytes.Venous blood was collected in citrate anticoagulant from J.W., E.M., and A.M. and simultaneously from five normal controls that were age and sex matched for each patient. A minimum of two samples were collected from each patient over an interval of several months. Cells were suspended in isotonic phosphate buffer plus albumin (5 g/L), for a final hematocrit of less than 1% to aid visualization.
Reticulocytes.For separation of low density or young cells, whole blood was layered on a solution consisting of 16.75 parts Tris-NaCl (5 mmol/L Tris, 16 mmol/L NaCl, 300 MOSM, pH 7.4) and 13.25 40% Hypaque (Sodium diatrizoate), then centrifuged at 4,480g for 40 minutes in a Beckman model TJ-6 centrifuge (Beckman Industries Inc, Fullerton, CA). This separated the erythrocytes into two bands: the least dense comprising less than 1% of the total volume of erythrocytes on the top and the remaining red cells beneath the Tris-Hypaque solution. Plasma and buffy coats were discarded, and the band of least dense erythrocytes was washed and suspended in isotonic Tris-NaCl plus albumin. Reticulocyte counts were performed on cells stained with methylene blue.
Quantitation of erythrocyte adherence.Erythrocytes were allowed to settle on the endothelial monolayer. Then under direct microscopic visualization, adhesion was quantitated for 7,000 cells per sample for each patient and control. Local wall shear stress was induced by flow from a 12-μ glass pipette filled with phosphate buffer. The pipette was placed adjacent to cells and fluid velocity produced a shear force, which caused unattached cells to move out of the field.13a
Calculation of shear stress is based on the Poiseuille-Hagen Law that characterizes laminar flow of a Newtonian fluid in a uniform diameter tube: ΔP = 8ηLQ/πr4; ΔP = pressure difference, L = tube length, η = fluid viscosity, r = tube radius, Q = volumetric flow rate. Poiseuille flow is characterized by a parabolic velocity profile with zero flow at the wall and maxium flow velocity at the axis. Wall shear rate (γw ) is γw = 4Q/πr3 . Wall shear stress Tw , equals the product of viscosity and wall shear rate Tw = ηγw . By substituting into the initial equation Tw = ΔPr/2L. Wall shear stress calculations for in vivo model pressure and vessel dimension measurements14 15 provided approximate ranges for arterioles, capillaries, and venules. The wall shear stress may also be calculated from the formula Tw = ηdV/dZ, V = axial velocity, and Z = radial distance from the center line of the pipette.
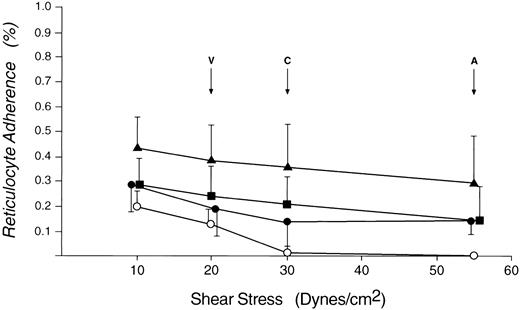
Mean percentage of reticulocytes that are adherent to cultured endothelial monolayers at various shear stresses. (▴), Patient A.M.; (▪), patient E.M.; (•), patient J.W.; (○), age- and sex-matched controls. V, maximum venule shear stress; C, maximum capillary shear stress; A, maximum arteriole shear stress.
Mean percentage of reticulocytes that are adherent to cultured endothelial monolayers at various shear stresses. (▴), Patient A.M.; (▪), patient E.M.; (•), patient J.W.; (○), age- and sex-matched controls. V, maximum venule shear stress; C, maximum capillary shear stress; A, maximum arteriole shear stress.
Calculation of shear stress on the erythrocytes resting on the endothelial surface was based on the assumption that the parabolic distribution of the velocity profile in the pipette is maintained approximately over the short interval between the pipette tip and the individual erythrocyte under observation. In this study the pipette was placed 1 μ from the erythrocyte and positive pressure was applied to the pipette to produce flow which impinged on the cell. The flow velocity, V, a function of applied pressure, was determined by observation of the velocity of small axially flowing particles in the buffer. Since the pipette axis is nearly parallel to the endothelial surface the actual force on the cell is approximately equal to the product of the wall shear stress and the projected area of the erythrocyte, F = Tw Ap . However, since the projected area or cross-section of the cell perpendicular to the direction of flow is fairly uniform due to the similarity of erythrocyte diameter and volume, the wall shear stress proportional to the force is a practical expression of the force on the cell and permits estimation of in vivo dynamics from the in vitro experiment.
Statistical analysis.Results are expressed as the mean ± SE. Statistical analysis of the data was calculated using the comparison of two Poisson distributed observations.
RESULTS
Each of the three study subjects has had a different clinical course during the past 30 years, ranging from relatively asymptomatic (E.M.), to progressive symptoms (A.M.), and life-threatening thrombotic complications post splenectomy (J.W.).
As shown in Fig 1, all three patients have an increased percentage of erythrocytes which are abnormally adherent to endothelial cells, compared with age- and sex-matched controls.
Patients with symptoms (J.W. and A.M.) have a higher percentage of adherent cells compared with their asymptomatic sibling (E.M.) and controls. The absolute numbers of adherent cells for each patient on repeated testing, as well as age and sex matched controls are depicted in Table 1. A.M. and J.W., unlike E.M., are significantly different from controls. The increased adherence seen for J.W. is particularly notable because she is hypertransfused to reduce her erythroid production, implying that a high proportion of her native cells are abnormally adherent.
Many of the bound red cells remained adherent to endothelial cells despite exposure to fluid shear force that exceeded physiologic shear force normally present in the microcirculation. Adherent red cells that separated from endothelial cells frequently reattached to adjacent endothelial cells, implying that their inherently adhesive properties do not require prolonged contact time.
A longitudinal study of patient A.M. is depicted in Fig 2. Figure 2A shows mean red cell endothelial adherence of repeated tests during several months when symptoms consisted of fatigue, arthralgias, intermittent abdominal pain, and occasional episodes of shortness of breath and severe chest pain. Because A.M. had progressive symptoms of compromised blood flow without identifiable etiology other than his abnormal erythrocyte endothelial adherence, we postulated that there may have been increased cytokine mediated erythrocyte endothelial adherence, and treated him with low dose pentoxifylline. This resulted in resolution of the acute episodes of chest and abdominal pain and, as shown in Fig 2B, a decrease in erythrocyte-endothelial adherence on repeated testing over the next 2 years. On two occasions A.M. reported decreased compliance in taking his pentoxifylline, which resulted in recurrence of his symptoms and a significant increase in red cell adherence (see Fig 2C). Table 2 lists the absolute numbers of adherent cells and P values for patient A.M. and controls. Patient A.M. had significantly greater erythrocyte adherence compared to control both before taking pentoxifylline and when the pentoxifylline was stopped.
To assess the possible contribution of reticulocytes to the adherence process, erythrocyte endothelial interaction was studied in density separated patient and control samples. As shown in Table 3, the separation procedure resulted in a high percentage of reticulocytes (78% to 87%) and these cells shown in Fig 3 were less adherent than the nonseparated cells shown in Fig 1.
DISCUSSION
The etiology of abnormal erythrocyte endothelial interaction in these patients with the dehydrated form of hereditary stomatocytosis is not clear. The most consistent structural abnormality in hydrocytic stomaotcytosis is a deficiency in the integral membrane protein band 7.2b.4-9 Protein band 7.2b is present but has not been quantitated for this family and recent studies of J.W. and E.M. using an informative polymorphic marker identified in the 7.2b gene have excluded linkage of hereditary stomatocytosis to the band 7.2b gene in these two patients.16
The clinical episodes of J.W. and A.M. resemble those seen in sickle cell anemia patients with vaso-occlusive crises. Standard clinical tests for documenting large vessel thromboses are often negative for in situ thromboses in the microcirculation, but J.W. had documented in situ pulmonary thromboses. Her thrombotic events began following splenectomy at the time of puberty and progressed with time but did not correlate with thrombocytosis. She had multiple vaso-occlusive crises at times when her platelet counts were normal and conversely, she has had no vaso-occlusive episodes since beginning hypertransfusion despite platelet counts to 800,000/μL. J.W.'s thrombotic events were not improved by antiplatelet or warfarin anticoagulation therapy but did respond to hypertransfusion, which suppressed erythroid production. A population of adherent red cells remains evident in J.W.'s blood before her transfusions. Splenectomy may have allowed circulation of a large proportion of pathologically adherent stomatocytes, which precipitated her vaso-occlusive episodes. These episodes and the proportion of adherent cells appear to be decreased by chronic transfusion. Data from this and several other kindred underscores the hazard of splenectomy in hereditary stomatocytosis because of the increased frequency of thrombotic events following splenectomy.17
Similar to patient J.W., patient A.M.'s symptoms progressed with time. A.M. was relatively asymptomatic until age 29 then had progressive symptoms of vaso-occlusion during the following 2 years. His platelet count remained normal, and his reticulocytosis and splenomegaly were constant. The potential influence of reticulocytes on the adherence measurements was studied using high reticulocyte samples from both patients and controls. Reticulocyte adherence was less than nonseparated red cell adherence making it unlikely that physiologically significant abnormal adherence could be attributed to a reticulocyte-rich population of cells.18 This conclusion also is supported clinically by the asymptomatic course of E.M. whose baseline reticulocytosis resembles that of patient A.M. and greatly exceeds the reticulocyte count of patient J.W.
Patient A.M.'s red cells were significantly more adherent to endothelium than those of his asymptomatic brother E.M. The factors resulting in this increased adherent population are unknown in A.M., but specific receptors and plasma factors that participate in erythrocte endothelial adherence may be operative.19-28 Pentoxifyllin, a pharmaceutical agent initially developed to promote improved red cell passage through the microcirculation in patients with compromised blood flow secondary to atherosclerotic vascular disease, decreases production of tumor necrosis factor-α and inhibits inflammatory cytokine mediated adherence.29-32 For patient A.M. the postulated downregulation of red cell adherence factors by pentoxifylline correlated with his improved clinical course, and on two occasions when there was poor compliance in taking medication his symptoms recurred and red cell-endothelial adherence significantly increased. However, this finding is in a single patient with a limited number of observations and there is no direct experimental evidence for therapeutic efficacy for pentoxyfylline.
The specific etiology of abnormal red cell-endothelial interaction in this family remains to be identified. Additional studies are planned in a larger number of hereditary stomatocytosis patients and the use of potential antagonists to this adherence process may further elucidate the mechanism of abnormal erythrocyte endothelial adherence.
Address reprint requests to Brian D. Smith, MD, University of Rochester, Highland Hospital, 1000 South Ave, Rochester, NY 14620.