Abstract
Despite complete matching of siblings for the HLA loci, after bone marrow transplantation (BMT), approximately 20% develop graft-versus-host disease (GVHD). This is presumably due to incompatibility of minor histocompatibility antigens (mHa). We investigated the polymorphisms of 14 adhesion molecules (CD2, CD28, CD31, CD34, CD36, CD42, CD44, CD48, CD49b, CD54, CD62L, CD86, CD102, and CD106) in Japanese subjects and their association with the occurrence of GVHD after allogeneic HLA identical BMT. Six molecules (CD2, CD31, CD42, CD49b, CD54, and CD62L), which were found to be polymorphic, were then examined in 118 HLA identical sibling donors and recipients who had undergone BMT. Association of the incompatibility of the polymorphic molecules with the presence or absence of GVHD was examined. In these six, we observed a significant correlation between acute GVHD and the compatibility of CD31 (codons 563/670) (Pcorrected = .018), and CD31 (codons 563/670) + CD62L (Pcorrected = .018) in patients with the HLA-B44–like superfamily. In patients with the HLA-A3–like superfamily, the compatibility of CD62L (Pcorrected= .03) and CD62L + CD49b (P = .004,Pcorrected = .078) was associated with acute GVHD. Therefore, CD31, CD49b, and CD62L might be candidates for immunodominant mHa.
© 1998 by The American Society of Hematology.
ACUTE GRAFT-VERSUS-HOST disease (GVHD) is a major cause of morbidity and mortality after bone marrow transplantation (BMT).1 Incompatibility of the major histocompatibility complex (MHC) is a primary cause of GVHD. Most recipients of marrow from HLA-mismatched donors develop GVHD.2 3
Even if the bone marrow (BM) donor and recipient have identical MHC antigens, the two major complications of allogeneic BMT, GVHD and leukemia relapse, may still occur. GVHD occurs in 10% to 35% of HLA genotypically identical BMT pairs.4-6 T-cell depletion of BM graft to prevent GVHD is associated with an increased risk of leukemia relapse, and GVHD itself is associated with the decrease of leukemia relapse after BMT. Donor-derived T lymphocytes that cause GVHD may also be effectors of GVL reactivity.7-11
In HLA-genotypically identical BMT, antihost alloreactive donor T cells are, by definition, directed against minor histocompatibility antigens (mHa) presented by the host.12-14 These antigens are recognized in the context of molecules encoded by the MHC.15-17 Snell et al18,19 were the first to observe transplantation antigens that were identified as mHas. Goulmy et al12,20 have identified certain types of mHas, such as the male-specific mHa (H-Y), and non-Y–linked mHas (HA-1 to HA-5), by isolating cytotoxic T-cell clones from lymphocyte populations in the blood of patients with severe GVHD. HA-1, -2, -4, and -5 are found only in individuals expressing HLA-A2, whereas HA-3 is restricted to HLA-A1.21 The nine amino acid peptide corresponding to HA-2 appears to be derived from a nonfilamentous class I myosin protein.22 Goulmy et al21 observed a significant relationship between GVHD and recipient/donor mismatch at HA-1 alone or at HA-1 plus one or more mismatches of HA-2, -4, and -5. They referred to clinically significant mHa as “major” mHa.
Behar et al23 reported an association between GVHD and mismatch at an amino acid polymorphism (leucine or valine at codon 125) within the adhesion molecule CD31 or platelet endothelial cell adhesion molecule-1 (PECAM-1).23 Sixty-seven percent of the recipients who had received a transplant from HLA-identical sibling donors with CD31 genotypes that were incompatible to the donor’s genotype developed GVHD, as compared with 22% of the recipients with compatible CD31 genotypes (P = .03). However, Nichols et al24 recently reported no significant association between CD31 (codon 125) mismatch and the development of severe GVHD in 301 patients who received BMT from HLA identical siblings.
We screened polymorphisms in adhesion molecules that are expressed as the sites of main injury in acute GVHD, such as vascular endothelial cells, skin, liver and lymphoid organs, and blood cells. We then examined the relationship between the compatibility of adhesion molecules and the development of acute GVHD in the case of BMT between HLA-identical siblings. We detected amino acid diversities in seven of 14 adhesion molecules: CD2 (lymphocyte function-associated antigen-2 [LFA-2], CD31 (PECAM-1), CD42 (glycoprotein [GP] Ib), CD49b (GPIa), CD54 (intracellular adhesion molecule [ICAM]-1), CD62L (leukocyte endothelial adhesion molecule-1 [LECAM-1]), and CD102 (ICAM-2). In particular, CD31 exhibited amino acid diversities not only in exon 3 at codon 125, but also at codon 80, in exon 8 and 12 at codon 563 and 670. We analyzed the association between acute GVHD and incompatibility of adhesion molecules.
MATERIALS AND METHODS
DNAs.
Forty-eight genomic DNAs were selected at random for the first screening of polymorphisms in adhesion molecules. A total of 209 genomic DNAs from unrelated healthy Japanese panels were used for detecting gene frequencies of polymorphisms in the adhesion molecules. Twenty-eight families (112 haploides) were used to determine CD31 alleles. DNAs of 118 BMT recipients and their genotypically HLA identical sibling donors were used to analyze the association between compatibility of adhesion molecules and acute GVHD. Patients’ blood was collected before transplantation.
Patients.
We studied 118 recipients of BM and their HLA identical sibling donors. The recipients were patients at Saku Central Hospital (Nagano), Japanese Red Cross Nagoya First Hospital (Nagoya), Hyogo College of Medicine Hospital (Nishinomiya), Yamaguchi University Hospital (Yamaguchi), Osaka Medical Center Hospital for Cancer and Cardiovascular Disease (Osaka), Osaka Medical Center and Research Institute for Maternal and Child Health (Osaka), Tokyo Jikei University Hospital (Tokyo), Kyoto City Hospital (Kyoto), Kyoto Prefectural Medical College Hospital (Kyoto), Kyoto University Hospital (Kyoto) and Tohoku University Hospital (Sendai). The group comprised 61 pairs of adults and 57 pairs of children under age 16. The recipients had undergone BMT between 1993 and 1997 for acute lymphocytic leukemia, acute myelocytic leukemia, chronic myelocytic leukemia, non-Hodgkin’s lymphoma, or aplastic anemia. None of the recipients had received BM depleted of T cells. As prophylaxis against GVHD, they had received methotrexate (one patient), cyclosporine (one patient), or both (116 patients). GVHD had been diagnosed and graded as a consensus of the opinions of the attending transplant physicians according to previously published standard clinical criteria.25 26
The screening of adhesion molecule polymorphisms.
Exon-specific amplifications of targeted adhesion molecules were performed using exon specific primers. Twelve DNA mixtures mixed with four genomic DNAs (48 DNAs in all) were amplified using polymerase chain reaction (PCR) with 1.25 U of Taq DNA polymerase. The reaction mixture (50 μL) contained 10 mmol/L Tris-HCl (pH 8.3), 50 mmol/L KCl, 1.5 mmol/L MgCl2, 0.2 mmol/L dNTP, and 20 pmol/L of each amplification primer. First, the reaction mixture was denatured at 95°C for 5 minutes, followed by 35 cycles of denaturation at 95°C for 1 minute, annealing at 59°C for 1 minute, and a final incubation at 72°C for an additional 5 minutes to complete the final extension step after the last cycle, using an automated PCR thermal sequencer (Gene Amp PCR system 9600; PE Applied Biosystems, Foster City, CA). PCR products were analyzed using low sonic strength–single-stranded conformation polymorphism (LIS-SSCP), which has been described.27 Briefly, 1 μL of PCR product was added to 20 μL of low ionic strength (LIS) solution (10% saccharose, 0.01% bromophenol blue, and 0.01% xylene cyanol FF). The mixture was denatured at 97°C for 2 minutes, and 4 to 10 μL of the mixture was applied to 10% polyacrylamide gel on a mini gel electrophoresis apparatus with a constant temperature control system. Electrophoresis proceeded in a buffer of 45 mmol/L Tris-borate (pH8.0)/1 mmol/L EDTA at 15 mA for 1.5 to 2.5 hours. To evaluate the optimal electrophoresis conditions, we performed electrophoresis under four different conditions by varying the running temperature between 22°C and 4°C and adding or not adding 10% glycerol to the polyacrylamide gel. The SSCP profiles in the gel were detected using silver staining. For the second screening, the PCR amplified fragments whose nucleotide mutations had been detected using LIS-SSCP were sequenced using the cycle-sequencing method with an automated DNA sequencer (Type 373A; PE Applied Biosystems). Both strands were sequenced. Nonsynonymous amino acid substitutions were selected using translation from nucleotide sequences to amino acid sequences with the DNASIS program (Hitachi Software Engineering Co, Ltd, Tokyo, Japan). To confirm mutated nucleotide sequences, PCR products that exhibited amino acid polymorphism were digested independently with each restriction enzyme. For the third screening, a population study of mutated amino acids was performed using 209 randomly selected DNAs. The 28 family studies were performed to determine the combination of mutated codons in CD31. The association between the compatibility of adhesion molecule and acute GVHD was analyzed in 118 patients who had received BM from HLA-identical siblings.
Statistical analysis.
The direct count method was used for allele frequency and linkage disequilibrium of polymorphic sites of CD31. The significance of differences between groups in Table 3 was calculated using Fisher’s exact test with the aid of JMP software (SAS Institute Inc, Cary, NC). When multiple comparisons are found to be significant, associations may arise by chance. To avoid such errorsP values were corrected with the number of characters compared (three for HLA-superfamily of A and B loci, two for CD31 of codon 125 and codons 563/670, six for combination analysis of two adhesion molecules). If the P value reached values of less than .05, then they were corrected for the total number of tests performed using the formula: Pcorrected = 1 − (1 − p)n, where p is the original P value and n is the number of tests performed. Odds ratios were computed using standard methods.28
RESULTS
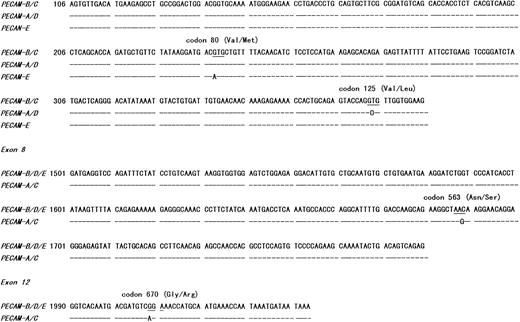
We screened for polymorphisms within the coding regions of human adhesion molecules that were mainly expressed on target tissues of GVHD or blood cells. Of 14 screened adhesion molecules, we observed amino acid mutations in seven: CD2 (LFA-2), CD31 (PECAM-1), CD42 (GPIb), CD49b (GPIa), CD54 (ICAM-1), CD62L (LECAM-1), and CD102 (ICAM-2). Amino acid mutations and their gene frequencies are shown in Table 1. CD31 is the most polymorphic adhesion molecule in the seven, in which we detected amino acid polymorphisms. CD31 had four amino acid mutations. These mutations were located in exon 3 at codon 80 (Val → Met), in exon 3 at codon 125 (Val → Leu), in exon 8 at codon 563 (Asn → Ser), and in exon 12 at codon 670 (Gly → Arg). All mutations were detected for the first time in this study, except for the mutation in exon 3 at codon 125, which has been reported by Behar et al.23 We performed 28 family studies to determine the substituted amino acids in each codon on the same haploid of CD31. We defined five CD31 alleles based on four amino acid mutations. The allele frequencies of CD31 in the Japanese population based on the data from 112 haploides are shown in Table 2. Mutation at codon 80 from valine to methionine was rare. We could detect this mutation in 209 randomly selected DNAs, but not in 28 families (113 DNAs). When the amino acid at codon 563 was serine (asparagine), the amino acid of codon 670 was always arginine (glycine). They were linked completely. The amino acid at codon 125, valine, showed a strong linkage disequilibrium with asparagine at codon 563, but did not show complete linkage. Their nucleotide sequences are shown in Fig 1.
Nucleotide sequence variations of CD31 alleles (A-E). The dashes indicate identity with PECAM-B/C or B/D/E. The alleles (A-E) were tentatively named in the present study (see Table 2). Only those alleles observed have been illustrated here.
Nucleotide sequence variations of CD31 alleles (A-E). The dashes indicate identity with PECAM-B/C or B/D/E. The alleles (A-E) were tentatively named in the present study (see Table 2). Only those alleles observed have been illustrated here.
We analyzed the relationship between the compatibility of adhesion molecules that exhibited amino acid polymorphism in the coding region, except CD102, which showed a low mutation rate (0.5%), and acute GVHD in 118 HLA-identical sibling transplants with respect to HLA restriction. The mutations of CD31 at codons 563 and 670 showed complete linkage, and thus were referred to as codons 563/670. The mutated codons 125 and 563/670 of CD31 were analyzed separately, as these showed incomplete linkage. We divided HLA antigens of patients into groups of superfamilies based on similarities of their peptide-binding motifs,29 such as HLA-A2–like, A3-like, and other for HLA-A locus antigens, and HLA-B7–like, B44-like, and other for the HLA-B locus. Patients without GVHD were compared with acute GVHD (grade 1 or above). We found that BMT pairs in the HLA-A3–like superfamily (HLA-A3, A11, A31, A33, and A*6801) showed a 100% occurrence of acute GVHD in CD49b and CD62L incompatible recipients, but showed 50% and 45% in compatible recipients, respectively. The association between the compatibility of CD62L and acute GVHD was statistically significant (P = .01,Pcorrected = .03) and odds ratio was 18.2. Even if CD49b showed a high odds ratio (7.0), there was no statistically significant correlation between incompatibility and acute GVHD (Table 3). CD49b (VLA-2, GPIa) is expressed mainly on platelets, monocytes, and endothelial cells, and amino acid substitutions were detected at codon 505, glutamic acid (gene frequency = 0.97) versus lysine (gene frequency = 0.03). This polymorphism is known as HPA-5.30 CD62L (LECAM-1) is expressed mainly by neutrophils, monocytes, natural killer (NK) cells, and subpopulations of B and T lymphocytes, and amino acid substitutions were detected at codon 213, proline (gene frequency = 0.8) versus serine (gene frequency = 0.2).
We analyzed the association between the compatibility of combination for adhesion molecules and acute GVHD in the HLA-A3–like superfamily. The definition of compatibility is as follows. It was found in the case of combination of CD49b and CD62L. In incompatible pairs, ie, pairs (n = 8) in which any CD49b or CD62L alleles found in the recipient were not repeated in the donor, GVHD occurred at a rate of 100%. On the other hand, in compatible pairs, ie, pairs (n = 39) in which the recipient had no CD49b and CD62L alleles that were foreign to those of the donor, GVHD occurred at a rate of 44%. The association between the compatibility of CD62L + CD49b and acute GVHD showed a significantP value (P = .004), but after correcting, it was not statistically significant (Pcorrected = .07), however the odds ratio was the highest (21.8) in the present test (Table 4). We did not find other significant correlations in the HLA-A3–like superfamily.
We found the correlation between the compatibility of codons 563/670 amino acid polymorphism of CD31 with acute GVHD in patients in the HLA-B44–like superfamily (HLA-B37, B41, B44, B45, B47, B49, B50, B60, and B61). The occurrence of acute GVHD in incompatible pairs (n = 16) was 88%, and in compatible pairs (n = 41), it was 44%. This difference between two groups based on compatibility was statistically significant (Pcorrected = .018, Table 4). However, the compatibility of exon 3 at codon 125 for acute GVHD was not statistically significant (Table 3). CD31 (PECAM-1) is expressed mainly on vascular endothelial cells, myeloid cells, platelets, and certain lymphocyte subsets.31 32 Moreover, we found the occurrence of acute GVHD in CD62L incompatible patients was much higher than in compatible patients, but it was not statistically significant (P = .27).
We performed the combination analysis of two adhesion molecules and acute GVHD in the HLA-B44–like superfamily. The compatibility was defined the same way as in the case of CD49b + CD62L. The association between the compatibility of CD31 codons 563/670 + CD62L and acute GVHD was significant (P = .001, Pcorrected = .018, Table 4). GVHD occurred in incompatible pairs (n = 23) at a rate of 83% and in compatible pairs (n = 34) at a rate of 38%. We found no statistically significant association with other combinations.
DISCUSSION
In this study, we screened each exon of 14 adhesion molecules using the LIS-SSCP method, and we found amino acid polymorphism within seven of them: CD2 (LFA-2), CD31 (PECAM-1), CD42 (GPIb), CD49b (GPIa), CD54 (ICAM-1), CD62L (LECAM-1), and CD102 (ICAM-2). The most polymorphic adhesion molecule was CD31, in which we detected four amino acid substitutions, which lead to five alleles, located at codons 80, 125, 563, and 670. The other adhesion molecules showed only one amino acid substitution in each of the coding regions.
We postulated that polymorphisms of adhesion molecules on target tissues or blood cells might be related to the occurrence of GVHD and/or GVL, and candidates of mHa. We analyzed the association between the compatibility of these adhesion molecules and acute GVHD in the context of HLA restriction. The effect of incompatibility of mHas on the development of GVHD is best studied in pairs of siblings who are genotypically HLA identical. In such pairs, the effect of the disparity would not be diminished by unknown mismatches of major histocompatibility antigens. Siblings discordant for mHas are possible only in families in which both parents are heterozygotes or one parent is heterozygous and the other homozygous for the mHa allele.33 An incompatible pair for development of GVHD is one in which the donor is homozygous and the recipient is heterozygous or homozygous for the mHa allele, but not identical with the donor. An mHa is of clinical interest only if it is immunogenic and has a somewhat frequent distribution in the population.
In this study, we wanted to identify candidates for mHa. Therefore, we used grade ≥1 acute GVHD as the positive biologic reaction in humans. We observed significant correlation between the compatibility of CD62L and acute GVHD in patients in the HLA-A3–like superfamily (HLA-A3, A11, A31, A33, and A*6801) and between acute GVHD and the compatibility of CD31 codons 563/670, and CD31 codons 563/670 + CD62L in patients in the HLA-B44–like superfamily (HLA-B37, B41, B44, B45, B47, B49, B50, B60, and B61). The association between the compatibility of CD62L + CD49b and acute GVHD in the HLA-A3–like superfamily was not significant (P = .004,Pcorrected = .07) because of the small number of incompatible pairs, however odds ratio was the highest (21.8). Therefore, CD49b might be a candidate for an immunodominant mHa.
For more relevant clinical correlation, we should use grade ≥2 acute GVHD. However, the aim in our study was the identification of candidates for immunodominant mHa and not actual clinical predictions. It is necessary to accumulate samples with more detailed clinical information in order to evaluate clinical applications for BMT.
We analyzed the association between the compatibility of adhesion molecule and acute GVHD in adults and children separately, and the results showed the same tendency as the total results (data not shown). We also analyzed the correlation between survival and compatibility of adhesion molecules. In the patients with the HLA-A3–like superfamily, incompatible pairs of CD49b (100%) and CD62L (86%) had slightly higher survival rates than compatible pairs (75% and 75%, respectively). In the patients with the HLA-B44–like superfamily, incompatible pairs of CD31 codons 563/670 (69%) and CD62L (66%) had slightly lower survival rates than compatible pairs (78% and 77%, respectively). The differences between the two groups were not statistically significant in either case.
There are two contradictory reports23,24 about the association between the compatibility of CD31 at codon 125 (Val/Leu) and acute GVHD. Behar et al23 reported that CD31 polymorphism is a risk factor for acute GVHD, and Nichols et al24 reported that compatibility of CD31 polymorphism is not associated with the occurrence of acute GVHD. Our results supported the results of Nichols et al. However, Nichols et al observed the effect of CD31 polymorphism at codon 125 only. Our data showed that CD31 is more polymorphic, and that polymorphism at codons 563/670 is a risk factor of acute GVHD in the HLA-B44–like superfamily of antigens. Amino acid mutation of codon 125 is incompletely linked to codons 563/670. The findings of Behar et al might be the result of linkage disequilibrium between codon 125 and codons 563/670. We could not find a statistically significant correlation between the compatibility of amino acids at codons 563/670 and acute GVHD without HLA restriction. However, in this situation, our data suggested a tendency toward increased risk of GVHD in the recipients of BM from donors whose amino acids were incompatible.
Cytotoxic T lymphocytes (CTLs) that are specific for recipient mHa trigger GVHD after BMT from donors who are genotypically HLA-identical.34 CTLs react in a classical MHC-restricted fashion.35 Sidney et al29,36-38 grouped HLA class I alleles into superfamilies based on similarities of their peptide-binding motifs. The capacity of a peptide to bind multiple MHC molecules and, consequently, to be immunogenic in the context of individuals from different MHC types has been referred to as degeneracy at the MHC or T-cell level. Recognition of cells that present the same peptide in the context of different MHC molecules has been termed promiscuous recognition. This phenomenon has been described with CTL lines specific for melanoma-associated antigens within the A2-like superfamily39 and for human immunodeficiency virus (HIV)-1–specific peptide within the A3-like superfamily.40These data validated the concept of HLA class I superfamilies. In this study, the HLA restriction of mHas was mainly analyzed using HLA class I superfamilies. Our data suggested that CD31 and CD62L, which were the candidates for immunodominant mHa based on the occurrence of acute GVHD in BMT of HLA-identical siblings, were restricted to the HLA-B44–like superfamily, and CD49b and CD62L were restricted to the HLA-A3–like superfamily.
We searched for putative peptides that were included in the polymorphic sites and were derived from these adhesion molecules (CD49b, CD31, and CD62L). Table 5 shows the supermotifs of HLA superfamilies and the putative peptides derived from these adhesion molecules. The amino acid polymorphisms within B pocket (which is normally occupied by the side-chain of the position 2 residue of bound peptides) and F pocket (which is normally occupied by the C-terminal residue of bound peptides) of the HLA class I binding groove were shared between HLA antigens of the same superfamily. The putative peptide from CD49b fit into the A3-like supermotif of bound peptides carrying somewhat hydrophobic residues at position 2 and positively charged residues in the C-terminal. Interestingly, the polymorphic amino acid of CD49b is the C-terminal residue. In CD31, the putative peptide that fit into the B44-like supermotif was found in exon 12, which is the cytoplasmic domain. In CD62L, the putative peptide that fit into the B44-like supermotif was also found. However, we could not define the putative peptide that fit into the A3-like supermotif of CD62L, even though the correlation between CD62L and acute GVHD in the HLA-A3–like superfamily was shown. This might be due to the presence of amino acid polymorphism in a position that could not be detected by our method and had complete linkage to the polymorphism of CD62L at codon 213.
In conclusion, our data demonstrate that amino acid polymorphism of adhesion molecules occurred frequently, in seven of 14 adhesion molecules. An association between compatibility of CD31 (codons 563/670), CD49b, and CD62L and acute GVHD in HLA-identical BMT in different HLA superfamilies was observed. Our results suggest that CD31 (codons 563/670), CD49b, and CD62L might be candidates for immunodominant mHa. Further studies are needed to confirm our results, such as the establishment of mHa-specific CTL clones in multiple members of a single HLA superfamily, and the extraction of mHa peptides from their restricted HLA molecules.
ACKNOWLEDGMENT
We thank Dr P.I. Terasaki (UCLA, Los Angeles, CA) and Dr K. Tokunaga (Tokyo University, Tokyo, Japan) for giving us useful discussion and suggestions, Dr H. Hiraga (Saku Central Hospital), Dr A. Sasada (Kyoto University, Kyoto), Dr M. Ohotake (Sendai City Hospital, Sendai), Dr Y. Wakazono (Kyoto Katsura Hospital, Kyoto), Dr T. Sakurai (Ishimaki Red Cross Hospital), Dr T. Shishido (Ishimaki Red Cross Hospital), Dr M. Iga (Shimane University, Shimane), Dr Y. Takahashi (Kyoto Prefectural Medical College Hospital, Kyoto), Dr H. Ohno (Kyoto University, Kyoto), Dr M. Itoh (Kyoto University, Kyoto), Dr K. Nishikawa (Tottori University Hospital, Tottori), Dr K. Tubaki (Kinki University, Osaka), Dr T. Nakao, Dr T. Egawa, Dr T. Torino (Osaka Medical Center Hospital for Cancer and Cardiovascular Disease, Osaka), Dr M. Naya, Dr M. Houjou, Dr H. Kajimoto (Kyoto City Hospital, Kyoto), Dr A. Miura (National Sendai Hospital, Sendai), Dr M. Minegishi (Tohoku University, Sendai), Dr Y. Akiyama (Kyoto University, Kyoto), Dr H. Nakagawa (Kyoto Red Cross First Hospital, Kyoto), and Dr I. Kawamura (Kurashiki Central Hospital, Kurashiki) for providing the patient samples.
Address reprint requests to Etsuko Maruya, BS, 644 Sanjusangendo Mawarimachi, Higashiyamaku, Kyoto 605, Japan; e-mail:maruya@mbox.kyoto-inet.or.jp or emaruya@hla.cbc.jrc.or.jp.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.