We have previously shown that leukemia-specific cytotoxic T cells (CTL) can be generated from the bone marrow of most patients with B-cell precursor acute leukemias. If these antileukemia CTL are to be used for adoptive immunotherapy, they must have the capability to circulate, migrate through endothelium, home to the bone marrow, and, most importantly, lyse the leukemic cells in a leukemia-permissive bone marrow microenvironment. We demonstrate here that such antileukemia T-cell lines are overwhelmingly CD8+ and exhibit an activated phenotype. Using a transendothelial chemotaxis assay with human endothelial cells, we observed that these T cells can be recruited and transmigrate through vascular and bone marrow endothelium and that these transmigrated cells preserve their capacity to lyse leukemic cells. Additionally, these antileukemia T-cell lines are capable of adhering to autologous stromal cell layers. Finally, autologous antileukemia CTL specifically lyse leukemic cells even in the presence of autologous marrow stroma. Importantly, these antileukemia T-cell lines do not lyse autologous stromal cells. Thus, the capacity to generate anti–leukemia-specific T-cell lines coupled with the present findings that such cells can migrate, adhere, and function in the presence of the marrow microenvironment enable the development of clinical studies of adoptive transfer of antileukemia CTL for the treatment of ALL.
DESPITE THE SUBSTANTIAL successes observed in the treatment of childhood acute lymphoblastic leukemia (ALL), treatment of adults with ALL and treatment of children who have either failed to enter remission or who have relapsed presents a significant obstacle to the cure for this disease. Moreover, curative chemotherapeutic strategies are accompanied by severe long-term adverse complications that significantly compromise the quality of life of long-term survivors. Because presently available treatment modalities for these patients have approached their therapeutic limit, the challenge is to develop new therapeutic strategies with nonoverlapping toxicities. Novel strategies could be used either at the attainment of minimal residual disease, at the quantitative increase in minimal residual disease, or at the time of clinical relapse. One such novel therapeutic approach is the induction of anti–ALL-specific immunity.
We and others have failed to detect clinically significant anti–leukemia-specific immunity in patients with B-cell ALL. Moreover, a defective cytolytic activity has been observed in leukemia patients.1-4 The generation of cytolytic cells capable of lysing leukemia cells has been attempted by several groups. For example, lymphokine-activated killer (LAK) cells have been generated from the peripheral blood and bone marrow of ALL patients.4-10 However, this strategy is based on the overall expansion of cytolytic cells and can also result in significant cytotoxicity of nonmalignant cells.5 In another approach, TCRγδ T-cell clones capable of lysing leukemia cells were generated.11 12 Despite some recent methodological advances, the generation and expansion of T-cell clones is a lengthy process and is not easily translatable to the clinic, unless the epitope determinant recognized by the antigen-specific T cells is known.
Therefore, a system that facilitates the generation of leukemia-specific cytotoxic T cells (CTL) offers obvious advantages for the development of an immunotherapeutic strategy that can be translated into clinical practice. We have previously shown that human B-cell precursor leukemia cells are either inefficient or ineffective allogeneic antigen-presenting cells (APC) but that they can be modified to become efficient APC by cross-linking the CD40 molecule expressed on their cell surface.13 In fact, cross-linking of CD40 results in the induction and/or upregulation of adhesion, major histocompatibility complex (MHC), and, more importantly, B7-family molecules.13 By using the CD40-stimulation strategy, we have developed a methodology that allows for the generation and/or expansion of anti–leukemia-specific autologous T-cell lines from the bone marrow of patients with B-cell leukemias.14 Generation of such CTL requires both improvement of the antigen-presenting capacity of the leukemia cells as well as culture conditions favorable for the stimulation and expansion of anti–leukemia-specific T cells.14
Although autologous anti–leukemia-specific CTL have been generated from more than half of the B-cell precursor ALL patients tested, it is not known whether these cells can function when adoptively transferred. To be successful in adoptive immunotherapy, antileukemia T cells must be able to circulate, migrate through endothelium, home to the bone marrow microenvironment, and, most importantly, lyse the leukemia cells in a microenvironment that favors tumor cell survival and proliferation. In the present study, we demonstrate that antileukemia T cells exhibit an activated phenotype and are capable of transendothelial migration through both venous and bone marrow endothelium and that these migrated cells preserve their cytolytic capacity. Moreover, these antileukemia T cells are capable of adhering to autologous bone marrow stroma. Finally, and most importantly, these antileukemia T cells are capable of lysing the leukemia cells in the presence of autologous bone marrow stroma without significant damage to the stromal cells.
MATERIALS AND METHODS
B-cell leukemia samples.
B-cell precursor ALL cells were obtained from the bone marrow and/or peripheral blood of patients with high leukemia involvement (>90%; except ALL-83: 72%). The ALL patients’ characteristics are shown in Table 1. Appropriate informed consent and Institutional Review Board approval was obtained for all sample collections. Samples were enriched by density centrifugation over Ficoll-Hypaque and then washed twice in RPMI-1640 supplemented with 10% (vol/vol) fetal bovine serum (FBS) and 2 mmol/L L-glutamine (further referred to as RPMI-10 media).
Generation of anti–leukemia-specific T-cell lines.
Autologous anti–leukemia-specific T-cell lines were generated and expanded as previously described.14 Briefly, high-density bulk cultures of bone marrow were initiated in the presence of 25% to 40% (vol/vol) soluble CD40L (sCD40L) in RPMI supplemented with 2% human AB serum (further referred to as RPMI-HS2; human serum was obtained from NABI, Miami, FL) and incubated at 37°C, 5% CO2. After 4 days, cells were harvested and dead cells were eliminated by density centrifugation over Ficoll-Hypaque. Live cells were then cultured at 2 × 106/mL in Iscove’s modified Dulbecco’s medium (IMDM; Mediatech, Herndon, VA) supplemented with 4% human AB serum (further referred to IMDM-HS4) and recombinant human interleukin-2 (rhu-IL-2; 20 U/mL) and were incubated at 37°C, 5% CO2. On day 7, fresh IMDM-HS4 media and IL-2 were added. On day 10, cells were harvested, dead cells were removed, and the live cells were restimulated with syngeneic CD40-stimulated leukemia cells. The same sequence of expansion and restimulation was repeated twice.14 For the T-cell restimulation, B-cell precursor ALL cells were stimulated by CD40-cross-linking using NIH3T3 cells stably transfected with the CD40L coding region (t-CD40L), as previously described.13 sCD40L was then used during the initial step (priming) of the generation of antileukemia T-cell lines, whereas tCD40L was used to obtain the CD40-stimulated leukemia cells (CD40-ALL) necessary for the restimulation of the antileukemia T-cell lines.
Endothelial cells and bone marrow stroma.
The bone marrow endothelial cell line BMEC15was used as human bone marrow endothelium. This cell line was kindly provided by Dr J. Ascensão (University of Nevada, Reno, NV) and was cultured in IMDM supplemented with 5% (vol/vol) FBS. Pooled human umbilical vein endothelial cells (HUVEC) in early passages were used as vascular endothelium. These HUVEC were obtained from Clonetics (San Diego, CA) and were cultured in EGM-2-MV media (Clonetics).
Human bone marrow stroma was generated either from the bone marrow of patients (when possible) or healthy donors. Bone marrow mononuclear cells were separated and resuspended at 2 × 106cells/mL (allogeneic donor) or 5 to 10 × 106 cells/mL (ALL patients) in RPMI supplemented with 12.5% (vol/vol) FBS, 12.5% (vol/vol) horse serum, 0.1 mg/mL deionized bovine serum albumin (BSA), 50 μg/mL iron-saturated transferrin, 10−4 mol/L 2-mercaptoethanol, 0.2 mmol/L i-inositol, 20 μmol/L folic acid, and 1 μmol/L hydrocortisone sodium succinate (further referred to as BMS media). Bone marrow stroma was expanded and maintained as described16 17 using either BMS media or MyeloCult media (Stem Cell Technologies, Vancouver, British Columbia, Canada).
Monoclonal antibodies (MoAbs) and fusion proteins.
MoAbs were used as purified Ig. The anti-CD11a (clone TS1/22) and anti-CD18 (clone TS1/18) antibodies were purified in our laboratory and produced from hybridomas obtained from ATCC (Manassas, VA). The anti-CD54 MoAb (clone R6.5) was kindly provided by Dr T. Springer (Boston, MA). The blocking antibodies CD29 (clone 4B4), anti-CD49d/VLA-4 (clone HP2/1), and anti-CD106/VCAM-1 (clone 1G11) were obtained from Immunotech/Coulter (Marseille, France). Fluorochrome-conjugated MoAbs anti-CD3 (clone UCHT1), anti-CD4 (clone 13B8.2), anti-CD8 (clone B9.11), and anti-CD29 (clone 4B4) were kindly provided by Coulter (Miami, FL). Fluorochrome-conjugated MoAbs anti-CD95 (clone UB2), anti-CD45RO (clone UCHL1), anti-CD26 (clone BA5), and anti-TCRαβ (clone BMA031) were kindly provided by Immunotech-Coulter. Fluorochrome-conjugated MoAb anti-4-1BB/CD137 (clone 4B4-1) was obtained from Ancell (Bayport, MN). Fluorochrome-conjugated MoAbs anti-CD100 (clone A8) and anti-CD40L/CD154 (clone TRAP1). The soluble CD40L (sCD40L), a fusion protein of CD40L and CD8α chain,18 was kindly provided by Dr P. Lane (Basel, Switzerland).
Chemokines and supernatants with chemoattractant activity.
RANTES and MIP-1α were obtained from R&D Systems (Minneapolis, MN) and were used at 100 to 500 ng/mL for the chemotaxis assays. Supernatants from mixed cultures (ratio 1:2) of syngeneic leukemia cells and antileukemia T-cell lines (from day 30 of the CTL generation system) were collected after 48 hours of culture at 37°C, 5% CO2, in serum-free AIM V (Life Technologies, Grand Island, NY) or Complete media (Mediatech, Herndon, VA).
Phenotypic analysis.
Expression of cell surface molecules was determined by direct labeling using standard methodology. Fc receptors were blocked by incubation with mouse Ig before the addition of the specific MoAbs. The MoAbs used were fluorescein isothiocyanate (FITC)-conjugates anti-CD3, anti-CD95, anti-CD100, and anti-4-1BB and phycoerythrin (PE)-conjugates anti-CD4, anti-CD8, anti-TCRαβ, anti-CD26, anti-CD29, anti-CD45RO, and anti-CD40L. Irrelevant isotype-matched antibodies (species and IgG subclasses) were used as negative controls. Appropriate controls were used to determine optimal voltage settings and electronic subtraction for the spectral fluorescence overlap correction. Samples were analyzed in a Coulter Elite or XL flow cytometer, and data were acquired in listmode files. At least 5,000 positive events were measured for each sample.
Transendothelial chemotaxis assay.
The transendothelial chemotaxis assay was performed as previously described.19 20 The migration through endothelium was performed using HUVEC or BMEC. Briefly, 1 × 105endothelial cells (HUVEC or the BMEC cells) were seeded on 6.5- or 24-mm diameter microporous collagen-I–coated Transwell inserts (Costar, Cambridge, MA) and cultured at 37°C to establish the endothelial layers (4 to 7 days or until monolayer confluence was reached). To assess endothelial cell confluence and the establishment of monolayers, sample inserts were stained with May-Grunwald-Giemsa and visualized by microscopy. For the chemotaxis assay, the assay media consisted of 1:1 mixture of AIM V media and IMDM. Chemokines (RANTES, MIP-1α, or the combination) or supernatants (50% vol/vol) were added to the assay media, distributed on cluster plates (lower compartment of chemotaxis system), and warmed for 15 minutes at 37°C. After the removal of culture media, the Transwell inserts covered with the endothelial monolayer were transferred to the prewarmed cluster plates. Antileukemia T cells (1 to 2 × 105 cells for 6.5-mm inserts; 1 to 2 × 106 cells for 24-mm inserts) were placed into the Transwell inserts (upper compartment of the chemotaxis system). The plates were incubated for 6 hours at 37°C, 5% CO2. Peripheral blood and/or bone marrow T cells purified by negative selection (by elimination of cells expressing CD19, CD14, CD11a, CD56, and MHC II) were used as controls. A control condition without chemokines or supernatant was also included. For the blocking experiments, T cells were incubated with the MoAbs for 30 minutes before the assay, and the endothelial cell monolayers were incubated for 30 minutes with the MoAb recognizing endothelial structures. The MoAbs were kept in the media for the entire period of the assay.
After the 6-hour chemotaxis, the Transwell inserts were removed and all of the liquid that accumulated directly beneath the filter (lower surface of insert) was gently recovered, because it contains an important number of migrated cells. After careful resuspension, all migrated cells were collected and counted by flow cytometry. The flow cytometer settings were determined before the acquisition of the migrated cells using samples of the input population. The migration percentage was calculated by dividing the number of migrated cells by the total number of input cells. When possible, the migrated cells were used for flow cytometry and functional studies.
Cytotoxic assay.
Cell-mediated toxicity was determined using either a standard51Cr-release assay or a fluorescence cytotoxicity assay.
The 51Cr-release assay was performed as described.21 Unstimulated and CD40-stimulated leukemia cells and bone marrow stromal cells were used as targets. Target cells were incubated with 0.1 mCi of 51Cr per 106cells at 37°C for 4 hours (leukemia cells) or 2 hours (stromal cells), followed by 5 washes in RPMI-HS4 media. Labeled target cells were then plated in 96-well U-bottom plates at 5,000 cells/well. T-cell lines generated from the patient’s bone marrow were used as effector cells and were plated at different effector/target ratios (5:1 to 40:1). All of the experiments were performed in triplicate. The plates were centrifuged for 3 minutes and incubated for 4 hours at 37°C. After the incubation period, the supernatants were harvested using the Skatron filters (Skatron Instruments, Sterling, VA) and radioactivity was measured in an automatic gamma counter (LKB Wallac, Turku, Finland). Specific lysis was determined for each individual experiment as follows: specific lysis (%) = ([experimental 51Cr release − spontaneous 51Cr release]/[maximum51Cr release − spontaneous 51Cr release] × 100). Maximum (Mx.) release was determined by the addition of 2% sodium dodecyl sulfate (SDS) to the target cells. In most of the patients shown, the spontaneous (Sp.) release from target leukemia cells was not greater than 20% and in no patient exceeded 30% of the Mx. release.
The fluorescence-based cell-mediated cytotoxicity assay was performed using the Live/Dead cytotoxicity kit (Molecular Probes, Eugene, OR) as described.22 23 Briefly, target cells were incubated with DiOC18(3) staining solution (10 μL for 1 × 106 cells) for 20 to 30 minutes at 37°C. After 2 washes, cells were resuspended in RPMI-HS4 media. Autologous T-cell lines (day 30) were used as effector cells and mixed with labeled target cells to yield the desired effector/target ratios (5:1 to 40:1). The counterstaining solution containing propidium iodide (PI) was then added to the cells. The cells were then mixed, pelleted by centrifugation, and incubated for 4 hours at 37°C. After the incubation period, the cells were resuspended and analyzed by flow cytometry. Live cells are detected as DiO+PI−, and dead (membrane-compromised) cells are detected as DiO+ PI+. Target cell lysis was determined for each individual experiment as follows: % lysis = ([DiO+ PI+ cells]/[total of DiO+cells] × 100). Control samples consisting of effector cells alone or target cells alone as well as target cells fixed with 0.1% formaldehyde to mimic membrane-compromised cells were prepared.
For the cytotoxic assays in the presence of bone marrow microenvironment, a stromal cell layer was established in the plates to be used for the cytotoxic assay by incubation of the stromal cells in MyeloCult media for 48 hours at 37°C, 5% CO2. Cell-mediated cytotoxicity was measured by the 51Cr-release assay performed as described above.
Adhesion assays.
For the adhesion assays, human bone marrow stroma layers were established in 96-well flat-bottom plates using stromal cells expanded as described above. The cell adhesion assay was performed as previously described.24,25 Antileukemia T cells (day 30 of CTL generation system) were labeled by incubation with the fluorescent dye BCECF-AM (Molecular Probes) for 30 minutes at 37°C. After 2 washes in phosphate-buffered saline (PBS), cells were resuspended in RPMI supplemented with 0.1% heat-inactivated BSA. Labeled cells (5 × 104 cells/well) were then added to the wells covered with the BM stroma layer and incubated for 30 minutes at 37°C, 5% CO2. Wells coated with BSA (0.1% in PBS) were used as a control. All of the conditions were tested in triplicate. After incubation, plates were gently washed 3 times with RPMI containing 10 mmol/L HEPES to remove unbound cells. The plates were then analyzed in a fluorescence analyzer (Cytofluor 2300; Millipore Corp, Bedford, MA). After subtraction of background cell binding to BSA-coated wells, the number of cells bound per square millimeter was calculated as described.26
Statistical analysis.
The statistical significance between the treatment groups was determined using the Wilcoxon test for matched pairs.
RESULTS
Autologous antileukemia T cells are mostly CD8+ T cells and exhibit an activated phenotype.
We have previously developed a culture system that allows for the generation and/or expansion of autologous antileukemia CTL.14 This system takes advantage of the expression of CD40 by the ALL cells (Table 2) and is based on our previous demonstration that cross-linking of this molecule results in significant increase in the APC capability of ALL cells.13 14 Using this culture system, T-cell lines were generated from the bone marrow of 14 of 19 B-cell precursor leukemia patients (Table 2). Note that significant CD40 expression is also observed in patients in which we failed to generate antileukemia T-cell lines using this system. As shown in Table 2, the median expansion of T cells observed was 29-± 14-fold (range, 6- to 50-fold), and these T cells are capable of killing autologous leukemia cells with specific lysis ranging from 28% to 63%.
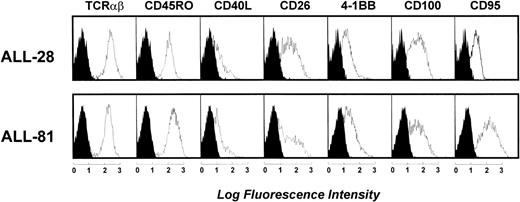
In all patients studied, these antileukemia cell lines are predominantly CD8+ T cells (Table 2). We then sought to further characterize the autologous T-cell lines generated in this culture system. These T-cell lines are TCRαβ-positive T cells and in their majority are CD45RO+ T cells (Table 2). Moreover, these T-cell lines exhibit an activated phenotype as demonstrated by the profile of expression of CD45RO, CD40L, CD26, 4-1BB/CD137, CD100, and CD95 (Fig 1). Finally, analyses of the production of IL-2, IL-4, IFNγ, and TNFα by these antileukemia T-cell lines showed that, although the levels of these cytokines varied between T-cell lines, they did not exhibit an exclusive (TH1-like or TH2-like) cytokine profile (data not shown).
Phenotypic characterization of autologous antileukemia T-cell lines generated from the bone marrow of patients with B-cell precursor ALL. The histograms shown are from 2 representative patients (of 10 studied). Open areas represent fluorescence distribution of the MoAbs tested and solid areas represent that of isotype-matched control antibodies. The cell number is shown on the y-axis. The expression of these molecules was CD45RO (72% to 95%), CD40L (12% to 47%), CD26 (36% to 70%), 4-1BB/CD137 (59% to 86%), CD100 (68% to 97%), and CD95 (73% to 100%). These autologous antileukemia T-cell lines produce both TH1- and TH2-type cytokines (data not shown).
Phenotypic characterization of autologous antileukemia T-cell lines generated from the bone marrow of patients with B-cell precursor ALL. The histograms shown are from 2 representative patients (of 10 studied). Open areas represent fluorescence distribution of the MoAbs tested and solid areas represent that of isotype-matched control antibodies. The cell number is shown on the y-axis. The expression of these molecules was CD45RO (72% to 95%), CD40L (12% to 47%), CD26 (36% to 70%), 4-1BB/CD137 (59% to 86%), CD100 (68% to 97%), and CD95 (73% to 100%). These autologous antileukemia T-cell lines produce both TH1- and TH2-type cytokines (data not shown).
Antileukemia CTL are capable of transendothelial migration in response to chemokines.
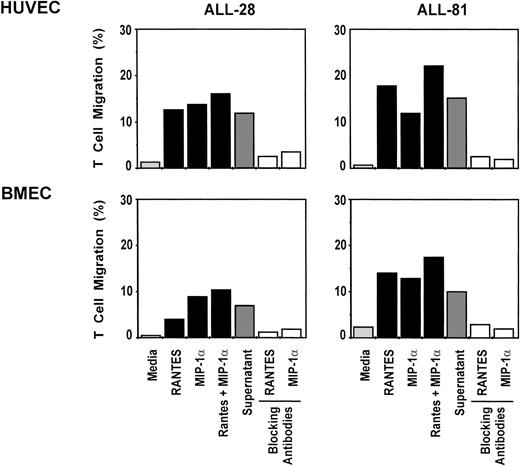
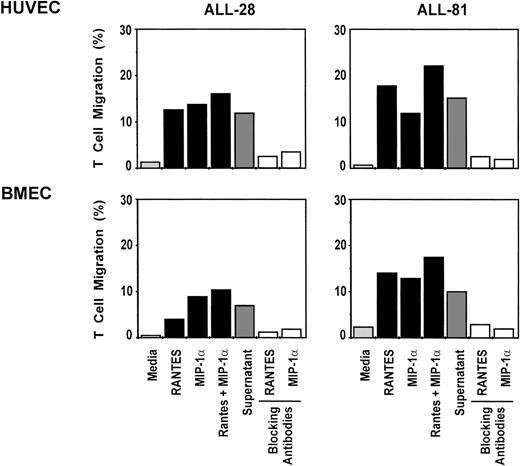
The first requirement for the potential use of these antileukemia T-cell lines for adoptive immunotherapy is that these cells are capable of migrating through endothelium. To determine whether the antileukemia CTL were capable of transendothelial migration, we used a chemotaxis assay using human endothelial cell layers established on microporous membranes. The endothelial cell layers were established using a human bone marrow endothelial cell line (BMEC) or HUVEC cells. Antileukemia T-cell lines were placed in the Transwell insert and their capacity to migrate through the endothelium in response to chemokines added to the lower compartment was assessed. As shown in Fig 2, T cells are capable of transendothelial migration in response to both MIP-1α and RANTES as well as in response to supernatants from the culture of autologous T-cell lines restimulated by irradiated leukemia cells. This migration is observed both through the HUVEC layer (Fig 2, upper panels) and the BMEC layer (Fig 2, lower panels), although the migration through the bone marrow endothelium is consistently lower. The transendothelial migration is observed in response to RANTES (13.8% ± 3.7% of the input cells migrated through the HUVEC layer v 7.3% ± 3.5% through the BMEC layer), MIP-1α (12.6% ± 1.1% with HUVEC layer v 9.7% ± 2.1% with BMEC layer), or a combination of both chemokines (17.7% ± 3.9% with HUVEC layer v 12.3% ± 3.2% with BMEC layer). The supernatants from the coculture of autologous antileukemia T-cell lines and leukemia cells also induced chemotaxis of the input T cells through both the HUVEC layer (12.4% ± 2.5%) and the BMEC layer (6.7% ± 2.5%). No significant migration of control purified T cells was observed in response to these chemokines (<2.5% through HUVEC and <2% through BMEC). As shown, in the absence of chemokines, the T cells are not capable of migrating through the endothelium (Fig 2, upper and lower panels). Moreover, no significant migration is observed when a checkerboard analysis was performed by also placing chemokines in the top compartment of the assay (data not shown). These results support the conclusion that significant migration occurs only when a gradient existed between the 2 compartments, demonstrating that this migration is directional (chemotaxis) and not random (chemokinesis). The transendothelial migration in response to both RANTES and MIP-1α is inhibited by the addition of a combination of the antiadhesion antibodies anti-CD11a/LFA-1, anti-CD54/ICAM-1, and anti-CD18 (Fig 2; RANTES,P < .01 with HUVEC and P < .01 for BMEC; MIP-1α,P < .01 with HUVEC and P < .05 with BMEC).
Transendothelial migration of antileukemia T-cell lines in response to recombinant chemokines or supernatants containing chemoattractants. Migration was assayed through Transwell inserts covered with the HUVEC cells (upper panel) or the bone marrow endothelial cell line BMEC (lower panel). The bars represent the percentage of input T cells migrated over the 6-hour chemotaxis assay. RANTES and MIP-1 were used at 100 ng/mL. The supernatant is from the culture of autologous T-cell lines (day 30) restimulated for 48 hours by irradiated CD40-stimulated leukemia cells (2:1 ratio). The combination of anti–LFA-1 (5 μg/mL), anti–ICAM-1 (5 μg/mL), and anti-CD18 (5 μg/mL) was used as blocking antibodies. Peripheral blood and/or bone marrow T cells purified by negative selection were used as negative controls; no significant transendothelial migration was observed through either HUVEC (<3%) or BMEC (<2%). The results shown are from 1 experiment (2 patients) and are representative of 3 different patients studied using the HUVEC and the BMEC layers.
Transendothelial migration of antileukemia T-cell lines in response to recombinant chemokines or supernatants containing chemoattractants. Migration was assayed through Transwell inserts covered with the HUVEC cells (upper panel) or the bone marrow endothelial cell line BMEC (lower panel). The bars represent the percentage of input T cells migrated over the 6-hour chemotaxis assay. RANTES and MIP-1 were used at 100 ng/mL. The supernatant is from the culture of autologous T-cell lines (day 30) restimulated for 48 hours by irradiated CD40-stimulated leukemia cells (2:1 ratio). The combination of anti–LFA-1 (5 μg/mL), anti–ICAM-1 (5 μg/mL), and anti-CD18 (5 μg/mL) was used as blocking antibodies. Peripheral blood and/or bone marrow T cells purified by negative selection were used as negative controls; no significant transendothelial migration was observed through either HUVEC (<3%) or BMEC (<2%). The results shown are from 1 experiment (2 patients) and are representative of 3 different patients studied using the HUVEC and the BMEC layers.
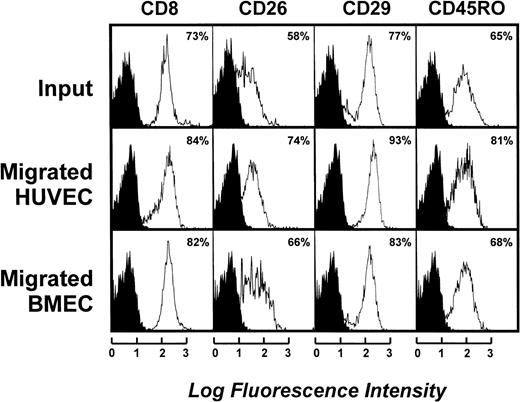
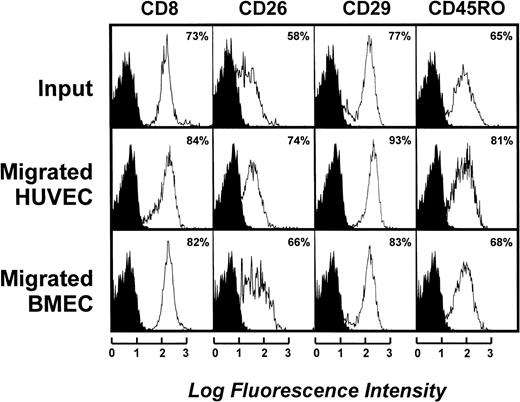
To determine the characteristics of the cells migrating through the endothelium, flow cytometric analysis of both the input and the migrated cells was performed. As shown in Fig 3, the phenotypic profile of the migrated cells is not significantly different from that of the input population. In fact, only a slight increase in the proportion of CD8+ T cells occurs with the transmigration through both the HUVEC and BMEC layers (Fig 3; 1 representative case of 3 studied). Furthermore, the proportion of cells expressing activation markers or a memory-type phenotype is slightly increased in the migrated populations as compared with the input population (Fig 3). Moreover, no significant differences are observed in the phenotypic profile of the cells that migrated through the HUVEC layer or the BMEC layer (Fig 3).
Phenotypic characterization of transmigrated antileukemia T-cell lines. Data represent both input (upper section) and migrated cell populations after the 6-hour chemotaxis assay through HUVEC endothelial cell layer (middle section) or the BMEC endothelial cell layer (lower section). The results are from a single patient and are representative of 3 different patients. Open areas represent fluorescence distribution of the molecules indicated and solid areas represent that of isotype-matched control antibodies. The cell number is shown on the y-axis.
Phenotypic characterization of transmigrated antileukemia T-cell lines. Data represent both input (upper section) and migrated cell populations after the 6-hour chemotaxis assay through HUVEC endothelial cell layer (middle section) or the BMEC endothelial cell layer (lower section). The results are from a single patient and are representative of 3 different patients. Open areas represent fluorescence distribution of the molecules indicated and solid areas represent that of isotype-matched control antibodies. The cell number is shown on the y-axis.
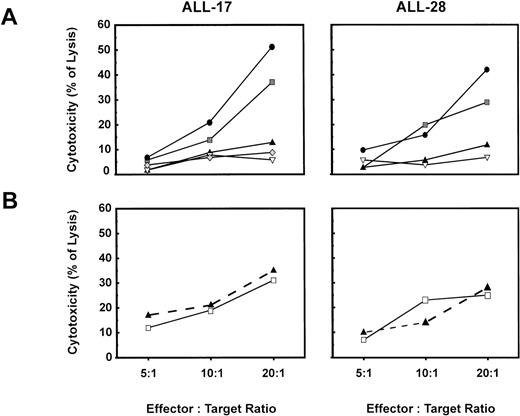
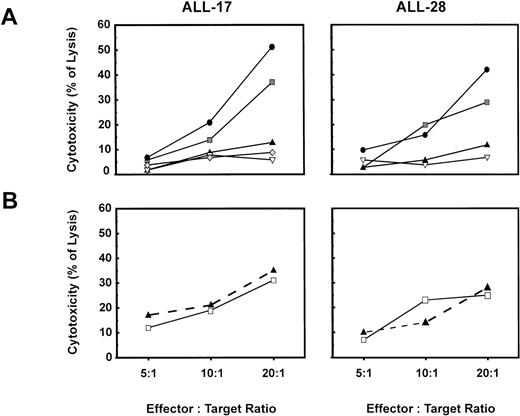
To determine the effect of the migration through bone marrow endothelium on the cytolytic capacity of the antileukemia T-cell lines, cytotoxic assays were performed using the autologous leukemia cells as targets and either the input T cells or the migrated T cells as effectors. As shown in Fig 4B, the T cells that migrated through the BMEC layer (□) were capable of lysing the autologous leukemia cells, and their cytolytic efficiency was not significantly different from that of the input T cells (▴). Because of limitations of the cell numbers available to perform the experiments with migrated T cells, no other cell targets could be used to confirm specificity. Nevertheless, cytolytic assays performed with the input T-cell populations clearly confirmed the anti–leukemia-specificity of these autologous T-cell lines (Fig 4A and Cardoso et al14).
T cells that migrated through endothelium are capable of lysing autologous leukemia cells. (A) Anti–leukemia-specificity of input cells was assessed by using as targets primary autologous leukemia cells (▩), autologous CD40-stimulated leukemia cells (•), autologous PHA blasts (▴), allogeneic CD40-stimulated leukemia cells (▵), and K562 cells (⧫). Target cells were labeled with DiOC18(3) and used at the effector/target ratios displayed. (B) Migrated T cells were recovered after the 6-hour chemotaxis assay and used for the cytotoxicity assay. Primary leukemia cells were labeled with DiOC18(3) and used as targets at the effector/target ratios displayed. Input cells (▴) and T cells that migrated through BMEC (□) were compared as effectors. Cell-mediated cytotoxicity was measured by flow cytometry as described in Materials and Methods.
T cells that migrated through endothelium are capable of lysing autologous leukemia cells. (A) Anti–leukemia-specificity of input cells was assessed by using as targets primary autologous leukemia cells (▩), autologous CD40-stimulated leukemia cells (•), autologous PHA blasts (▴), allogeneic CD40-stimulated leukemia cells (▵), and K562 cells (⧫). Target cells were labeled with DiOC18(3) and used at the effector/target ratios displayed. (B) Migrated T cells were recovered after the 6-hour chemotaxis assay and used for the cytotoxicity assay. Primary leukemia cells were labeled with DiOC18(3) and used as targets at the effector/target ratios displayed. Input cells (▴) and T cells that migrated through BMEC (□) were compared as effectors. Cell-mediated cytotoxicity was measured by flow cytometry as described in Materials and Methods.
These findings demonstrate that the antileukemia CTL generated in this system are capable of migrating through endothelium without significant alteration of their phenotype or cytolytic capacity.
Antileukemia CTL are capable of adhering to human bone marrow stroma.
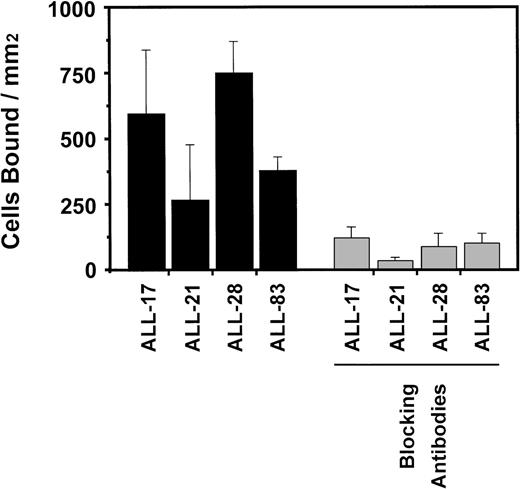
In light of the capacity of the antileukemia T cells to migrate through endothelium, we next sought to determine whether these T-cell lines were capable of adhering to the bone marrow microenvironment. Although it does not prove that the T cells will home to the bone marrow in vivo, adherence to autologous bone marrow stroma in vitro is an indication of the functionality of the antileukemia T-cell lines generated in our system. To assess their adhesive properties, antileukemia T cells were labeled with the dye BCECF-AM and plated on a layer of autologous bone marrow stroma. As shown in Fig 5, antileukemia T cells are capable of adhering to autologous bone marrow stroma, with this adhesion ranging from 172 to 885 cells bound/mm2. This assay shows that 19% to 67% of the plated T cells could adhere to the autologous stroma (data not shown). This adhesion to the autologous bone marrow stroma could be significantly inhibited (P < .01) by the addition of a cocktail of anti-integrins antibodies anti-CD29 (β1 integrin), anti-CD49d/VLA-4 (α4 integrin), and anti-CD106/VCAM-1 (Fig 5).
Autologous antileukemia T-cell lines adhere to autologous bone marrow stroma. Results indicate the mean ± SD number of cells bound per surface area from 1 representative experiment (3 independent experiments with T-cell lines from 6 patients). Background adherence was determined by the binding of these cells to BSA-coated wells. Stromal cell layers were established in 96-well plates as described in Materials and Methods. The blocking antibodies anti-CD29, anti-CD49d/VLA-4, and anti-CD106/VCAM-1 were used at 5 μg/mL.
Autologous antileukemia T-cell lines adhere to autologous bone marrow stroma. Results indicate the mean ± SD number of cells bound per surface area from 1 representative experiment (3 independent experiments with T-cell lines from 6 patients). Background adherence was determined by the binding of these cells to BSA-coated wells. Stromal cell layers were established in 96-well plates as described in Materials and Methods. The blocking antibodies anti-CD29, anti-CD49d/VLA-4, and anti-CD106/VCAM-1 were used at 5 μg/mL.
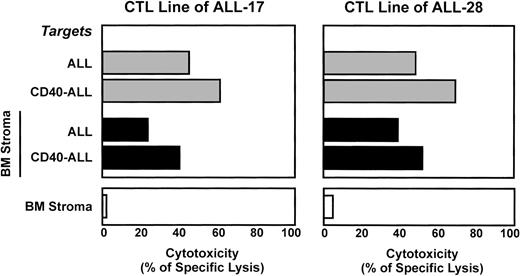
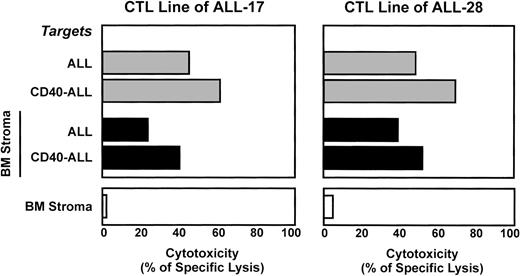
Antileukemia CTL lyse leukemia cells in the presence of bone marrow microenvironment but do not damage the stromal cells.
A final requirement necessary before undertaking a clinical adoptive immunotherapy trial is to demonstrate that antileukemia T cells are capable of lysing the leukemia cells in their bone marrow tumor-permissive microenvironment. Cytolytic assays were thus performed to assess the capacity of autologous antileukemia T-cell lines to lyse leukemia cells in the presence of stroma derived from the patient’s bone marrow (autologous stroma). As shown in Fig 6, T-cell lines (day 30) are capable of lysing both unstimulated and CD40-stimulated autologous leukemia cells in the presence of the autologous bone marrow stroma, although the tumor cell lysis was consistently inferior to that observed in the absence of stroma. Stromal cells were also labeled and used as targets to assess whether the T-cell lines are capable of lysing the stroma. Importantly, the autologous T cells generated in our system did not lyse autologous bone marrow stroma (Fig 6). These studies demonstrate that the antileukemia T cells are capable of lysing the leukemia cells in the presence of autologous bone marrow stroma without significant cytolysis of the stroma.
Antileukemia T-cell lines are capable of lysing syngeneic leukemia cells in the presence of bone marrow stroma. Stromal cell layers were established as described in Materials and Methods. Cell-mediated cytotoxicity was measured using the 51Cr release assay and is represented as a percentage of specific lysis. The results shown are from 2 patients representative of 4 independent experiments (4 different patients) and correspond to an effector:target ratio of 40:1. On the lower panel, stromal cells were labeled with51Cr and used as target cells.
Antileukemia T-cell lines are capable of lysing syngeneic leukemia cells in the presence of bone marrow stroma. Stromal cell layers were established as described in Materials and Methods. Cell-mediated cytotoxicity was measured using the 51Cr release assay and is represented as a percentage of specific lysis. The results shown are from 2 patients representative of 4 independent experiments (4 different patients) and correspond to an effector:target ratio of 40:1. On the lower panel, stromal cells were labeled with51Cr and used as target cells.
DISCUSSION
Our previous studies demonstrating that leukemia-specific CTL could be consistently generated from the bone marrow of patients with B-cell precursor leukemias have suggested a potential use of these cells for adoptive T-cell immunotherapy. However, to be used in such strategies, the antileukemia CTL must have the capability to circulate, migrate through endothelium, home to the bone marrow, and, most importantly, lyse the leukemia cells in a leukemia-permissive bone marrow microenvironment. In the present study, we analyzed the functional properties of autologous antileukemia T-cell lines to assess whether these cells are appropriate for adoptive immunotherapy. Our findings show that these cells are capable of migrating through the endothelium and that this migration does not affect their capacity to lyse tumor cells. Moreover, we observed that these autologous antileukemia T cells can adhere to an autologous bone marrow stroma and are capable of lysing the leukemic cells in the presence of that stroma.
Because conventional treatment of ALL is frequently accompanied by long-term adverse complications that significantly compromise the quality of life of survivors,27-29 future antileukemia treatment strategies must attempt to reduce the intensity and/or duration of conventional therapy while increasing the cure rate. To achieve these goals, novel anti-ALL therapeutic strategies must ideally induce specific lysis of residual leukemia cells or, at least, induce a state of long-term tumor latency. To this end, we and others have developed methodologies to improve the APC capacity of leukemia cells13,30 and to generate autologous antileukemia CTL.14 31 These studies support the notion that cell-mediated immunotherapy might be an important anti-ALL therapeutic strategy. However, translation of these studies to the clinic can take several forms, including (1) the administration of modified, APC-competent leukemia cells as a tumor vaccine; (2) the adoptive transfer of antileukemia CTL generated ex vivo; or (3) strategies using both T-cell adoptive therapy and leukemia cell vaccination. Regardless of which strategy is tested first, a number of well-founded concerns must be addressed. First, successful vaccination strategies are dependent on the existence and frequency of antileukemia reactive T cells in the patient’s T-cell repertoire, as well as the capacity of modified tumor cells to migrate to sites where these T cells are located. Both these questions remain to be answered and will require extensive study. Although antileukemia T cells can be expanded ex vivo, several preclinical and clinical issues must be addressed for adoptive T-cell immunotherapy to be successful, including the number of T cells that can be generated and the capability of the infused CTL to migrate, home to the bone marrow, and lyse leukemia cells in leukemia-permissive microenvironments.
It is well established that T lymphocytes undergo targeted transmigration and that antigen-reactive memory T cells migrate predominantly through tissue endothelium, in particular through the tissue where specific antigen exposure initially occurred.32-34 Moreover, the influx of CD8+ CTL from the blood has been documented during antigen challenge.35-37 In this context, our findings that antileukemia T-cell lines can fulfill some of the requirements necessary to be used in adoptive immunotherapeutic strategies is important. First, we observed that the autologous T-cell lines are capable of adhering to both vascular and bone marrow endothelium (data not shown), which is the first critical step for the migration of lymphocytes from circulation into the tissues.38,39 Second, these T cells are capable of migrating through vascular endothelium and also through bone marrow endothelium. To our knowledge, this is the first demonstration that bone marrow-derived, ex vivo-generated, antileukemia T cells can migrate through bone marrow endothelium. Third, an increased proportion of CD45RO+ cells was observed in the migrated population, which is in agreement with the observation that the CD8+ T cells expressing CD45RO migrate preferentially through the HUVEC endothelium.40 Fourth, the transmigration through endothelium did not result in significant loss of the antileukemia cytolytic properties of these T-cell lines. Lastly, no significant differences were observed in the phenotype and functional characteristics of the cells that migrated through the HUVEC as well as those that migrated through the BMEC.
Although the percentage of T cells migrating across the endothelium varied between patient specimens, the migratory properties of these antileukemia T cells are clear. The relatively high proportion of cells capable of transendothelial migration is likely due to the fact that these T cells were generated through multiple cycles of restimulation with activated leukemia cells as well as long-term exposure to IL-2. It has been shown that the proportion of LAK cells capable of migrating through endothelium increases with the length of exposure to IL-2.41 Moreover, because it has been reported that LAK cells are capable of lysing endothelial cells,41-44 we performed the migration assays at a low T-cell/endothelial cell ratio to avoid endothelial cell injury. No significant damage of either the HUVEC or the BMEC endothelial layers was observed when the autologous antileukemia T-cell lines were tested for transendothelial chemotaxis (data not shown).
The acquisition of privileged interactions with their microenvironment is a crucial requirement for the establishment of tumors. Direct contact with bone marrow stroma facilitates the in vitro adhesion-dependent survival of leukemic B cells45,46 and results in a selective survival and proliferative advantage for the leukemia. Moreover, leukemia-associated stromal cells produce cytokines that have inhibitory effects on immune responses (A. Cardoso, unpublished results). Therefore, successful adoptive immunotherapy with autologous antileukemia T-cell lines will require them to lyse the leukemic cells in the presence of a marrow microenvironment that favors tumor cell survival. We show here that antileukemia T cells can successfully lyse their targets even in the context of an autologous stroma microenvironment. However, it should be noted that the efficacy of these CTL is consistently reduced when compared with the cytolysis evaluated in the absence of stroma. Whether this partial inhibition of antileukemia cytolysis will require the use of larger numbers of CTL in an adoptive transfer protocol remains to be determined. Finally, because others have observed that cytotoxic lymphocytes can lyse cells that constitute the microenvironment, such as fibroblasts and endothelial cells,42-44,47,48 our finding that the antileukemia T cells generated in our system did not lyse the autologous bone marrow stromal cells is important. This observation supports our previous findings that the antileukemia T cells lines generated in this system did not lyse other autologous targets such as mitogen-activated T cells or a bone marrow cell population of non-T non-B cells.14 Therefore, these results support the hypothesis that the bone marrow microenvironment that is essential for hematopoietic reconstitution after myeloablative therapy might not be affected by the adoptively transferred antileukemia T-cell lines.
Increasing evidence suggests that adoptive T-cell immunotherapy may be a successful modality to treat viral infections and cancer. Striking results have been observed in the treatment of patients with viral infections such as cytomegalovirus (CMV), Epstein-Barr virus (EBV), and human immunodeficiency virus (HIV-1).49-56 In these studies, antiviral antigen-specific CTL and T-cell clones have been generated ex vivo and adoptively transferred to patients with active infections with, in some cases, dramatic clinical resolution. Similar results have been observed in patients with malignancies, such as chronic myelogenous leukemia (CML), melanoma, and non-Hodgkin’s lymphoma.56-59
Novel strategies for the isolation of antigen-specific T cells14 could facilitate the development of clinical protocols for the adoptive transfer of highly effective antigen-specific T-cell clones.55 However, the use of this approach will be restricted to instances in which the antigens recognized by the CTL are known, and reagents to identify these CTL are available. This is certainly not the case for ALL, for which there is little evidence for spontaneous antileukemia T-cell immunity and no universal or broadly expressed antigens have yet been identified. Until these leukemia-associated antigens are known, clinical protocols of adoptive T-cell therapy in ALL will require the use of polyclonal or oligoconal T-cell lines generated against leukemia cells. In this study, we have shown that such T-cell lines can specifically lyse the leukemia cells in their permissive microenvironment, providing a rationale basis for clinical translation.
Supported by National Institutes of Health Grants No. P01-CA68484-02 and P01-CA66996-01 to L.M.N. J.P.V. is a recipient of a fellowship from Fundação para a Ciência e para a Tecnologia (Portugal). P.G. received support from the American-Italian Cancer Foundation; Toby S. Meyerson, Esq. of Paul, Weiss, Rifkind, Wharton & Garrison; and Jerry I. Speyer, President of Tishman Speyer Properties Inc. H.M.A. is supported by a joint program of Protech (Private Industry Council, Boston, MA) and the Dana-Farber Cancer Institute.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Angelo A. Cardoso, MD, PhD, Dana-Farber Cancer Institute, D-538, 44 Binney St, Boston, MA 02115; e-mail:cardoso@mbcrr.harvard.edu.