Abstract
A mutation in the γ-glutamyl carboxylase gene leading to a combined congenital deficiency of all vitamin K-dependent coagulation factors was identified in a Lebanese boy. He is the first offspring of consanguineous parents and was homozygous for a unique point mutation in exon 11, resulting in the conversion of a tryptophan codon (TGG) to a serine codon (TCG) at amino acid residue 501. Oral vitamin K1 administration resulted in resolution of the clinical symptoms. Screening of several family members on this mutation with an RFLP technique revealed 10 asymptomatic members who were heterozygous for the mutation, confirming the autosomal recessive pattern of inheritance of this disease. In 50 nonrelated normal subjects, the mutation was not found. This is the second time a missense mutation in the γ-glutamyl carboxylase gene is described that has serious impact on normal hemostasis.
Introduction
Vitamin K functions as a cofactor for the endoplasmic enzyme γ-glutamyl carboxylase, which catalyzes the posttranslational modification of glutamate residues (Glu) into γ-carboxy glutamate residues (Gla).1 Gla residues form calcium-binding groups in proteins and are essential for their biologic activity.2 The human γ-glutamyl carboxylase gene was recently cloned by Wu et al,3 who also succeeded in the purification of the corresponding recombinant protein. The enzyme (94 kd) consists of 758 amino acids. Its cDNA has an open reading frame of 2277 nucleotides and is encoded by the 15 exons of the carboxylase gene.4
Besides vitamin K deficiency, there may be several other reasons for under carboxylation of all Gla-containing proteins. First, the recycling of vitamin K may be impaired by a blockade of KO-reductase as a result of coumarin ingestion, which may lead to exhaustion of the available vitamin K stores. Second, malfunction of the precursor protein caused by mutation(s) in the propeptide region may result in either poor substrate recognition by carboxylase5 or impairment of propeptide cleavage from the mature Gla protein.6 Third, the γ-glutamyl carboxylase gene itself may be mutated.
Hereditary combined deficiency of all vitamin K-dependent procoagulants and anticoagulants is a rare bleeding disorder reported only by a few authors.7-11 Until now, only one report of hereditary deficiency of all vitamin K-dependent proteins was linked to a defective γ-glutamyl carboxylase.12 These authors showed a missense mutation in exon 9 of the γ-glutamyl carboxylase gene, leading to the conversion of an arginine to a leucine at residue 394 in the γ-glutamyl carboxylase enzyme (L394R).
In the current study, we report a missense mutation in the γ-glutamyl carboxylase gene from a G to C, resulting in the substitution of a tryptophan for a serine, leading to a deficiency of all vitamin K-dependent proteins. The mutation is held responsible for the associated bleeding symptoms.
Study design
Case report
Patient 4 (Figure 1D) is a full-term, breast-fed boy from Baalbeck, Lebanon, who was brought for treatment at age 7 days for severe bleeding from the umbilicus. He is the first offspring of consanguineous asymptomatic parents (patients 30 and 2). There was no family history of bleeding disorders and no history of drug intake during pregnancy. Laboratory evaluation showed markedly prolonged prothrombin time and partial thromboplastin time values. Renal and liver functions were normal. After a diagnosis of deficiency of all vitamin K-dependent factors, he was given 5 mg/d of vitamin K1 orally (Roche, Basel, Switzerland).
Identification of W501S mutation.
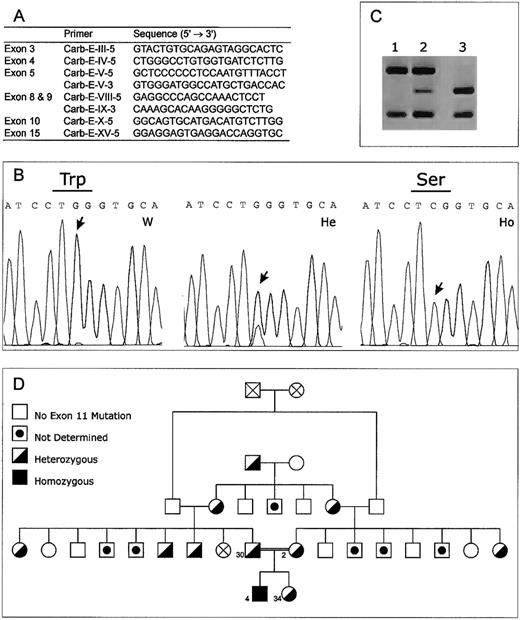
(A) Primers used for sequencing of the γ-glutamyl carboxylase gene. Only primers that are different from those reported by Brenner et al12 are indicated. (B) Sequence analysis of genomic DNA from a normal control subject (W), a heterozygous patient (He), and the homozygous patient (Ho). (C) RFLP analysis of the W501S mutation, which results in loss of a BstNI site in the amplified exon 11 DNA. Lane 1, patient's DNA homozygous for the mutation; lane 2, heterozygous pattern; lane 3, normal, control. (D) Pedigree of the Lebanese family showing the segregation of the W501S mutation in the γ-glutamyl carboxylase gene.
Identification of W501S mutation.
(A) Primers used for sequencing of the γ-glutamyl carboxylase gene. Only primers that are different from those reported by Brenner et al12 are indicated. (B) Sequence analysis of genomic DNA from a normal control subject (W), a heterozygous patient (He), and the homozygous patient (Ho). (C) RFLP analysis of the W501S mutation, which results in loss of a BstNI site in the amplified exon 11 DNA. Lane 1, patient's DNA homozygous for the mutation; lane 2, heterozygous pattern; lane 3, normal, control. (D) Pedigree of the Lebanese family showing the segregation of the W501S mutation in the γ-glutamyl carboxylase gene.
Genomic DNA samples
Genomic DNA was extracted from leukocytes by means of the QIAamp Blood Kit (Qiagen GmbH, Hilden, Germany). The 15 exons of the γ-glutamyl carboxylase gene were screened for mutations by polymerase chain reaction amplification and subsequent sequencing of both strands by using an automated ABI Prism 310 DNA sequencer (PE Biosystems, Nieuwerkerk aan de ijssel, The Netherlands). Primers were as described,12 except for the primers shown in Figure 1A. For simple analysis of the W501S mutation, exon 11 was amplified, the subsequent fragments were digested with BstNI (New England BioLabs, Beverly, MA), and restriction enzyme fragments were analyzed by agarose gel electrophoresis. The study was approved by the local medical ethics committee, and informed consent was obtained from all participants, according to the Declaration of Helsinki.
Results and discussion
Repeated tests showed that all blood coagulation factors were normal except for the vitamin K-dependent factors II (4.8%), VII (less than 1%), IX (6.4%), and X (less than 1%) (Table1). No abnormality was found when the patient's DNA was screened for the L394R mutation in exon 9, reported by Brenner et al.12 Therefore, sequence analysis of all 15 exons, including intron–exon borders, was necessary to identify a potential new mutation in the carboxylase gene. It appeared that the patient was homozygous for a unique point mutation in exon 11, resulting in the conversion of a tryptophan codon (TGG) to a serine codon (TCG) at residue 501 (W501S; Figure 1B; GenBank accession numberAF253530). No other mutations were found in the exons or in the intron–exon regions. The asymptomatic parents were both heterozygous for the W501S mutation (Figure 1D, subjects 30 and 2). We designed a simple RFLP technique for the detection of the mutation based on the presence of 3 BstNI sites in the unaffected allele and 2BstNI sites in the affected allele (Figure 1C). The rapid diagnosis of the W501S mutation makes it possible to identify the defect in the γ-glutamyl carboxylase gene in these and other families and to predict associated bleeding disorders. With this technique, we analyzed 50 normal white control subjects and most members of the patient's pedigree. The mutation was not found in any of the control subjects (data not shown), but it was found in 8 heterozygous family members (Figure 1D). Procoagulant activi-ties were not affected in any of the heterozygous family members, confirming the autosomal recessive pattern of inheritance of this disease.
This is the second case in which a missense mutation in the γ-glutamyl carboxylase gene is responsible for low procoagulant activity. The mutation may affect either the vitamin K binding site or the propeptide binding site. In both cases the efficacy of vitamin K1 supplements may be explained by the fact that under physiological conditions the concentration of the cofactor is near or below its Km. The effect of vitamin K administration may lead to an increase in the carboxylation rate, resulting in a partial correction of the deficiency. In preliminary expression studies, W501A (tryptophan changed to alanine)-mutated recombinant carboxylase was expressed in High 5 insect cells. In vitro experiments indicated that the activity of the mutated carboxylase was considerably decreased (D. Stafford, personal communication). This suggests that the Trp501 is critical for carboxylase activity, and it is to be expected that the W501S γ-glutamyl carboxylase mutation reported here has a similar impact on the enzyme activity. Sugiura et al13 already described that point mutations at the charged residues 513/515 resulted in a carboxylase enzyme with reduced affinity for the propeptide. Earlier, we reported14 a defective carboxylase in Devon Rex cats resulting in a bleeding tendency. We have identified the nature of this abnormality as a possible mutation in the carboxylase substrate binding site, leading to an increased dissociation constant for reduced vitamin K1 and consequently to an increased requirement for vitamin K1. The clinical phenotype in the Devon Rex cats is similar to the phenotype found in the carboxylase W501S mutant of the patient, which suggests that both mutations are located in a corresponding sequence of the carboxylase gene.
In the patient's plasma, descarboxy–osteocalcin was also demonstrated in high concentrations, indicating that not only hepatic proteins but also extrahepatic proteins are affected by the carboxylase mutation. This is consistent with the current view that only one gene encodes the γ-glutamyl carboxylase in all tissues in which it is found. Because Gla proteins are not only involved in blood coagulation but also in preventing (soft) tissue calcification, the reported mutation may lead to bone malformation, increased risk for arterial calcification, or both.
Acknowledgments
We thank Dr Rony Sayad, Dr Myrna Germanos, and Mrs Amale Richa for their contributions. We also thank Dr Darrel Stafford for sharing with us unpublished data, Dr Guillaume van Eys for helpful discussion, and Mrs Kitty Linssen for excellent technical assistance.
H.M.H.S. and R.A.F. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Berry A. M. Soute, Department of Biochemistry, Maastricht University, PO Box 616, 6200 MD Maastricht, The Netherlands.