Abstract
We have genetically engineered CD4+ and CD8+ T cells with human immunodeficiency virus (HIV) specificity by inserting a gene, CD4ζ, containing the extracellular domain of human CD4 (which binds HIV env) linked to the zeta (ζ) chain of the T-cell receptor (which mediates T-cell activation). Twenty-four HIV-positive subjects received a single infusion of 2 to 3 × 1010 autologous CD4ζ-modified CD4+and CD8+ T cells administered with (n = 11) or without (n = 13) interleukin-2 (IL-2). Subjects had CD4 counts greater than 50/μL and viral loads of at least 1000 copies/mL at entry. T cells were costimulated ex vivo through CD3 and CD28 and expanded for approximately 2 weeks. CD4ζ was detected in 1% to 3% of blood mononuclear cells at 8 weeks and 0.1% at 1 year after infusion, and survival was not enhanced by IL-2. Trafficking of gene-modified T cells to bulk rectal tissue and/or isolated lamina propria lymphocytes was documented in a subset of 5 of 5 patients at 14 days and 2 of 3 at 1 year. A greater than 0.5 log mean decrease in rectal tissue–associated HIV RNA was observed for at least 14 days, suggesting compartmental antiviral activity of CD4ζ T cells. CD4+ counts increased by 73/μL at 8 weeks in the group receiving IL-2. There was no significant mean change in plasma HIV RNA or blood proviral DNA in either treatment arm. This sustained, high-level persistence of gene-modified T cells demonstrates the feasibility of ex vivo T-cell gene therapy in HIV-infected adults and suggests the importance of providing HIV-specific T-helper function.
Much experimental and observational data suggest that the T-cell immune response plays a major role in containment of human immunodeficiency virus (HIV) during acute and chronic infection. The emergence of HIV-specific CD8+ cytotoxic T lymphocytes (CTLs) coincides with the rapid decrease in plasma viremia during acute infection, and the frequency of HIV env–specific CTLs is inversely correlated with plasma viral load and the rate of decline in CD4+ T-cell counts.1,2 Furthermore, a decline in HIV-specific CD8+ T cells occurs in patients as they progress to later stages of the disease.3 Most HIV-1–infected long-term nonprogressors have high circulating levels of HIV-1–specific CTL precursors,4,5 and increased HIV-specific CTLs as well as high HIV-specific CD4+ T-cell proliferative responses have been demonstrated in HIV-exposed seronegative subjects.6,7 The most direct evidence of the role of CD8+ T cells in HIV infection comes from recent studies of CD8+ T-cell depletion in acute and chronically infected macaques with simian immunodeficiency virus (SIV). In the setting of chronic SIV infection, CD8+ T-cell depletion led to a rapid 1- to 4-log increase in plasma viral load, which returned to baseline coincident with recovery of CD8+ T cells in the blood.8 Following acute SIV infection, CD8+T-cell depletion led to longer persistence of high-level viremia and a more rapidly progressive disease course compared with nondepleted monkeys.9
Animal and human experiments in chronic viral infection have demonstrated that antigen-specific CD4+ T-cell responses are critical for maintenance of CTLs and eradication of viral infection.10,11 Most studies have shown HIV-specific CD4+ T-cell proliferative responses to be absent or low in patients with chronic, progressive HIV infection.12,13Following initiation of combination highly active antiretroviral therapy (HAART), the recovery of HIV-specific CD4+ T–helper cell responses has been observed only in patients treated very early after acute infection.14Vigorous HIV-specific CD4+ responses have been associated with control of viremia in the absence of drug therapy and clinical long-term nonprogression.14 Although recent flow cytometry–based studies have demonstrated the presence of HIV-specific CD4+ T cells in the majority of actively infected individuals, functional enhancement is still likely to be necessary for optimal defense against HIV.15 In total, these data suggest that both arms of the host cellular immune response are necessary for containment of HIV.
Immunotherapy of viral infection with the use of antigen-specific T cells has been studied in the setting of cytomegalovirus (CMV), Epstein-Barr virus (EBV), and HIV. Adoptive transfer of allogeneic CMV-specific10,16 or EBV-specific17-19 T cells in bone marrow transplant recipients has resulted in recovery of virus-specific CTL activity, reduction of viremia, and effective prophylaxis or treatment of CMV- and EBV-induced disease. Endogenous recovery or adoptive transfer of antigen-specific CD4+ T cells was required for long-term maintenance of transferred CMV- or EBV-specific CTLs.19 20 Thus, adoptive immunotherapy with antigen-specific T cells is likely to require co-infusion of CD4+ and CD8+ T cells to achieve optimal in vivo survival and activity.
Adoptive transfer of HIV-specific T cells has potential as immunotherapy for HIV infection. Strategies to date have focused on ex vivo–expanded autologous HIV-specific CD8+ monoclonal or polyclonal T cells.21-24 Rather than isolating and expanding rare T-cell clones with major histocompatibility complex (MHC)-restricted antigenic specificity, a method has been developed to generate large numbers of HIV-specific primary T cells rapidly using retroviral-mediated gene transfer to insert an HIV-targeting gene (CD4ζ).25 CD4ζ is a genetically engineered, MHC-unrestricted, chimeric immune receptor composed of the zeta (ζ) subunit of the CD3 T-cell receptor (the cytoplasmic domain involved in signal transduction) fused to the transmembrane and extracellular domains of human CD4 (which targets HIV env expressed on the surface of infected cells). The MHC-unrestricted nature of this chimeric receptor allows HIV-specific targeting of both CD4+ and CD8+ T cells. This may also circumvent the potential ability of HIV to evade the T-cell immune response through down-regulation of HLA molecules on the surface of infected cells.26-28
Preclinical studies of CD4ζ gene-modified CD8+ T cells have demonstrated antigen-specific proliferation and cytokine production, cytolytic activity against HIV-infected T cells, and inhibition of viral replication in HIV-infected macrophages equivalent to that seen with naturally occurring HIV-specific CTL clones.25,29 Preliminary studies of adoptive transfer of ex vivo–expanded CD4ζ-modified syngeneic CD8+ T cells in HIV-infected twin pairs demonstrated a rapid decline in gene-marked cells in the blood, suggesting a lack of HIV-specific CD4+T-cell help to maintain the transferred CTLs.30 Recent advances in ex vivo culture methods have allowed us to develop an efficient ex vivo T-cell stimulation and gene transfer system that yields mixed populations of gene-modified CD4+ and CD8+ T cells.31 We now report the data from a phase II clinical trial of co-infusion of autologous CD4ζ-modified CD4+ and CD8+ T cells administered with or without exogenous interleukin-2 (IL-2) in 24 HIV-infected patients with detectable viral loads.
Patients and methods
Subjects
HIV-seropositive individuals over the age of 13 years on stable antiretroviral therapy for more than 8 weeks with viral loads of 1000 to 100 000 copies/mL and CD4 counts greater than 50/μL were enrolled in this study between May and December 1997. Informed consent was obtained in accordance with institutional review board guidelines. Patients were excluded for significant comorbid illness, active opportunistic infection or malignancy, or recent history of treatment with immunomodulatory agents.
Vector production
The CD4ζ retroviral vector rkat4.2SVGF3e− is a variant of the previously described rkat43.3F3 vector and was constructed using the pBR322 plasmid and a murine maloney leukemia virus (MMLV) backbone.32 This vector codes for a chimeric receptor gene composed of the extracellular and transmembrane domains of human CD4 linked to the cytoplasmic domain of the CD3 T-cell receptor ζ chain. The vector titer on NIH 3T3 cells ranged from 2 to 15 × 106 viruses/mL. Master and working cell banks and vector lots all tested negative for replication competent retrovirus (RCR) by supernatant amplification and cocultivation onMus dunni cells.33
T-cell processing
Lymphapheresis was performed locally using an automated cell separator (Cobe Spectra or CS-3000, Lakewood, CO) with processing of 6 to 10 L of blood to achieve a minimum of 5 × 109peripheral blood mononuclear cells (PBMCs). Apheresis products were shipped to Cell Genesys, Foster City, CA, at room temperature and processed within 24 hours of receipt. PBMCs were isolated by density gradient separation using a Stericell device (Haemonetics, Braintree, MA). Recovered cells were stimulated using magnetic beads (Dynal, Oslo, Norway) coated with anti-CD3 (OKT3) and anti-CD28 (monoclonal antibody 9.3), at a bead to cell ratio of 3:1, in serum-free AIM-V medium (Gibco, Long Island, NY) containing IL-2 (200 IU/mL; Chiron, Emeryville, CA) and antiretroviral agents (1 μmol/L zidovudine, Burroughs Wellcome, Research Triangle, NC; 10 μmol/L didanosine, Bristol Myers Squibb, Princeton, NJ; and 500 μmol/L ritonavir, Abbott Laboratories, Chicago, IL). On day 3, the beads were removed using a Maxsep magnetic bead separator (Baxter, Roundlake, IL) and resuspended in AIM-V medium with IL-2 and ritonavir. Transduction with CD4ζ retroviral supernatant at a multiplicity of infection of 2 viral particles per cell was performed on days 5 and 7 in AIM-V medium containing IL-2, ritonavir, and polybrene (Aldrich, St Louis, MO). Supernatant was removed by centrifugation using a SteriCell harvester, and cell expansion in AIM-V medium with IL-2, zidovudine, didanosine, and ritonavir continued until the target cell dose of 3 × 1010 was obtained (days 10-17). The final T-cell products were cryopreserved in 50-mL bags containing 6 × 109 cells/bag in Plasmalyte-A (Baxter IV Systems, Roundlake, IL) with 10% dimethylsulfoxide (Sigma, St Louis, MO), 1% dextran-40 (Baxter IV Systems), and 5% human serum albumin (Alpha Therapeutics, Los Angeles, CA), and stored in liquid nitrogen. Final T-cell products were tested for viability (by trypan blue exclusion), sterility, Mycoplasma, transduction efficiency (CD4ζ presence by polymerase chain reaction [PCR]), HIV replication (p24 enzyme-linked immunosorbent assay; NEN Life Sciences, Boston, MA), RCR (cocultivation on M dunni cells), and HIV-specific CTL activity. Cytolytic activity was assessed in a standard cytotoxic T-lymphocyte assay with 293 cells (human embryonic kidney line) expressing HIV env as cytolytic targets.25Phenotypic analysis was performed using antibodies to CD3, CD4, CD8, CD28 (Coulter, Miami, FL), CD25 (Caltag, Burlingame, CA), and CD62L (Pharmingen, San Diego, CA). Cryopreserved T cells were thawed in a 37°C water bath at the patient's bedside and infused directly through a peripheral intravenous catheter over 5 to 10 minutes per bag.
Treatment, toxicity, and response evaluation
Subjects were randomized to receive a single intravenous infusion of 2 to 3 × 1010 CD4ζ gene-modified T cells administered with or without exogenous IL-2. IL-2 was administered as a 5-day continuous intravenous infusion at a dose of 6 million IU/24 hours, beginning 4 hours before the T-cell infusion. All subjects were followed for at least 8 weeks after the T-cell infusion and monitored for toxicity, changes in plasma HIV viral load (ultrasensitive Roche Amplicor kit, sensitivity 40 copies/mL), HIV proviral DNA (HIV DNA PCR; Specialty Labs, Los Angeles, CA), CD4+ T-cell count, and gene-modified T-cell persistence in peripheral blood (CD4ζ DNA PCR; Specialty Labs). A subset of 5 patients was monitored for rectal mucosa–associated viral burden and tissue trafficking of CD4ζ T cells. Follow-up was extended to 1 year in 18 of 24 subjects.
CD4ζ T-cell survival and gene expression
CD4ζ DNA PCR.
PBMCs were isolated by standard Ficoll gradient separation. In a subset of patients, immunoselection for CD4+ and CD8+Tcells was performed before PCR analysis. Immunoselection of CD8+ T cells from whole blood was performed by first depleting monocytes using anti-CD14–coated beads (Dynal) followed by positive selection with anti-CD8–coated beads (> 95% purity). Immunoselection for CD4+ T cells was performed by first depleting monocytes and CD8+ T cells from the samples using anti-CD14– and anti-CD8–coated beads followed by positive selection with anti-CD4–coated beads (> 95% purity). DNA was recovered by phenol–chloroform extraction and ethanol precipitation. Quantitation of globin and CD4ζ copy number was performed by real-time PCR on an ABI Prizm 7700 instrument (Taqman PCR; Perkin-Elmer Applied Biosystems, Foster City, CA). Primers for CD4ζ PCR amplify a region spanning ζ and the 3′ untranslated region and are as follows: forward primer, 5′-ACC CGG TTC ACT CTT CTC AG-3′; reverse primer, 5′-ACA GGT GGG GTC TTT CAT TC-3′; and internal probe, 5′-(FAM) CAC AGA CTG TTG TCC CTG CAC TCT (TAMRA)-3′. PCR reactions were carried out with the Taqman PCR reagent kit (Perkin-Elmer Applied Biosystems). Amplification was performed for 45 cycles (initial activation: 94°C, 10 minutes; cycling: 94°C, 15 seconds, 57.5°C, 45 seconds). Copy number was determined using normal PBMC DNA as a beta-globin standard and CD4ζ PCR product as the standard for CD4ζ quantitation. Assay sensitivity was 117 copies/106 cells.
CD4ζ RNA reverse transcriptase (RT)-PCR.
Total RNA was isolated from PBMC pellets using TriReagent (Molecular Research Center, Cincinnati, OH) following the manufacturer's protocol; cDNA was prepared using Superscript II reverse transcriptase (Life Technologies, Long Island, NY). Samples were incubated at 48°C for 90 minutes and then digested with RNase H at 37°C. RNA isolated from PBMC pellets from HIV-negative human donors was used as a control. PCR amplifications were performed using TaqMan technology, as described earlier. CD4ζ PCR product was used to generate a CD4ζ standard curve. To normalize results for the efficiency of mRNA isolation, we amplified reduced glyceraldehyde-3-phosphate dehydrogenase (GAPDH) in a separate Taqman PCR reaction and used it to generate a standard reference series. Data analyses for CD4ζ and GAPDH amplifications were performed using the Sequence Detection System software (version 1.6.3) default settings.
HIV proviral DNA assay
DNA was isolated from PBMCs, and quantification of globin and HIV-1 proviral DNA copy number was performed by Taqman PCR, as described for CD4ζ DNA PCR. Primers sequences recognized HIV gag and were as follows: forward primer, 5′-CTC TAA GAG CCG AGC AAG CTT C-3′; reverse primer, 5′-GGT CCT CCT ACT CCC TGA CAT-3′; and internal probe, 5′-(FAM)-AAG CAT TGG GAC CAG CGG CTA CAC T-(TAMRA)-3′. Amplification was performed for 50 cycles with the same cycling conditions as for CD4ζ DNA PCR. Plasmid BH1034 was used as a standard for HIV-1 DNA copy number quantification. BH10 contains a replication-defective copy of the HIV-1 subtype B isolate HxB2. Assay sensitivity was 35 copies/106 cells.
Replication-competent retrovirus (RCR) testing in patients
Analysis for RCR was performed using Taqman PCR. Genomic DNA was isolated from PBMCs using the Puregene kit (Gentra Systems, Minneapolis, MN) following the manufacturer's protocol. PCR primers S-RCR-F1 (5′-GGG ACA CGG GAT GCT CTA AA) and S-RCR-R1 (5′-GGA AGG AAT TGG ATA CTT TGG AGA) amplify a 70-bp sequence in the envelope region of the amphotropic murine leukemia virus. AmpErase (UNG. 0.5U) was included in the PCR reaction. PCR amplifications were performed in an ABI Prizm 7700 instrument using the following cycling conditions: 50°C × 2 minutes, 95°C × 10 minutes, 95°C × 15 seconds, and 60°C × 1 minute (40 cycles). Data analysis was performed using the Sequence Detection System software, as described previously. A 466-bp PCR product derived from the MMLV plasmid pkat2Ampac.Utd was used to generate a standard curve in triplicate (1-1000 template copies) for assay quantitation. Assay sensitivity was 7 copies/106 cells.
Rectal biopsy substudy
Patients enrolled at the University of California, Los Angeles were eligible for a substudy to analyze serial biopsies of rectal mucosa for viral burden and the presence of CD4ζ-modified T cells.
Biopsy acquisition.
Flexible sigmoidoscopy was performed 1 week before T-cell infusion and at days 3, 7, and 14 after infusion. At each procedure, 10 biopsies (large-cup, 3.3 OD, 8 mm span; Microvasive) were obtained circumferentially at a standard level of 30 cm. Each biopsy was approximately 2 to 3 μL. Six biopsy specimens were immediately frozen in liquid nitrogen and stored at −80°C. Four specimens were placed in RPMI medium for subsequent isolation of mucosal mononuclear cells.
Isolation of mucosal mononuclear cells for CD4ζ analysis.
Four biopsy specimens in RPMI 1640 medium were transferred into a sterile petri dish containing Ca2+/Mg2+-free phosphate-buffered saline (PBS) supplemented with 50 μmol/L 2-mercaptoethanol and 100 mmol/L EDTA, and teased apart using two 18G needles. The dispersed tissue was incubated at 37°C in a shaking water bath for 20 minutes, washed twice with PBS, resuspended in 0.1 mg/mL of collagenase/dispase (Boehringer Mannheim, Indianapolis, IN) in RPMI 1640, and further incubated at 37°C with shaking for 60 minutes. The digested tissue was repeatedly aspirated through an 18G followed by a 20G needle and filtered through a 70-μ cell strainer to yield a single cell suspension. Mononuclear cells were enumerated visually, and viability was assessed by trypan blue exclusion. Absolute cell numbers were confirmed by flow cytometry with the use of Trucount beads (Becton Dickinson, San Jose, CA). These techniques yielded an average of 0.2 to 5.0 × 105 CD45+mononuclear cells, 1.0 to 4.0 × 104CD4+ T cells, and 1.0 to 8.0 × 104CD8+ T cells per 4 biopsies.35
HIV RNA analysis of bulk rectal tissue.
Biopsies from each patient were homogenized (Powergen homogenizer; Fisher Scientific, Pittsburgh, PA) and Trizol-extracted (Gibco), with separation of RNA and DNA phases to ensure that RNA for viral load assays and DNA for CD4ζ analysis were from the same biopsy. RNA was further extracted with the Rneasy kit (Qiagen, Valencia, CA). All analyses were performed on 2 biopsy specimens extracted independently and run in duplicate.36,37 RT-PCR for HIV RNA was performed using the Thermostable rTth Reverse Transcriptase RNA PCR kit (Perkin-Elmer) with oligonucleotide primer pairs 667/AA55 specific for the R/U5 region of HIV LTR RNA and was designed to capture both unspliced and multiply spliced HIV RNA.38Primer 667 was radiolabeled using T4 kinase with32P. A linear standard curve was generated by amplifying the in vitro synthesized HIV LTR RNA sequences diluted in seronegative tissue RNA. Percentage RNA recovery was estimated using seronegative frozen biopsies with known quantities of a synthesized 140-bp sequence recognized by the 667/AA55 primers and was greater than 95%. PCR products were quantified using the Ambis Image Analysis System. Sensitivity was 10 copies/μg RNA.
CD4ζ PCR assay.
DNA was extracted from frozen rectal biopsies and mucosal mononuclear cells using Trizol reagent, as described earlier, with DNA subsequently isolated by ethanol precipitation with 2 washes in 0.1 mol/L sodium citrate/10% ethanol buffer. Isolated DNA was transferred to Cell Genesys for amplification of CD4ζ DNA.
Statistical analysis
Treatment groups were compared for differences in absolute levels and changes from baseline for each efficacy end point with a 2-sample Student t test and a 2-sample Wilcoxon test, and adjustment was made for multiple correlated comparisons. Undetectable values for efficacy end points were set to 50% of the detection limit for the purposes of analysis. For change from baseline analyses, an average of 2 preinfusion values (week −1 and week 0) was used to calculate the baseline. Adverse events were coded using the fifth edition of the Coding Symbols for Thesaurus of Adverse Reaction Terms (COSTART).
Results
Patient characteristics and treatment
Twenty-five patients were enrolled in the study between May 29, 1997, and December 3, 1997. One patient was removed from the study before cell infusion because of failure of T-cell processing. Twenty-four patients received cell infusions and completed 8 weeks of follow-up. Eleven patients were randomized to receive a single infusion of 2 to 3 × 1010 CD4ζ-modified T cells plus IL-2 (6 million IU/24 hours by continuous intravenous infusion × 5 days), and 13 were randomized to receive CD4ζ-modified T cells alone. Table 1 lists the patient demographics and baseline laboratory data for the 24 treated patients. The majority of patients were male, white, and 30 to 50 years of age, and had an excellent performance status. Twenty (83%) had been diagnosed with HIV infection more than 3 years before enrollment. Mean viral load at enrollment was 20 137 copies/mL and mean CD4+ T-cell count was 332/μL. There were no statistically significant differences between the treatment groups for any screening covariates. One patient was taking no antiretroviral drugs and 23 (96%) were taking stable antiretroviral medications from at least 8 weeks before cell infusion through 8 weeks of follow-up, with 1 exception (switch from lamivudine/indinavir to saquinavir/nelfinavir 36 days after infusion). Twenty (83%) were taking protease inhibitors, 6 (25%) were taking non-nucleoside reverse transcriptase inhibitors, and 7 (29%) were taking hydroxyurea.
Characteristics of CD4ζ T-cell products
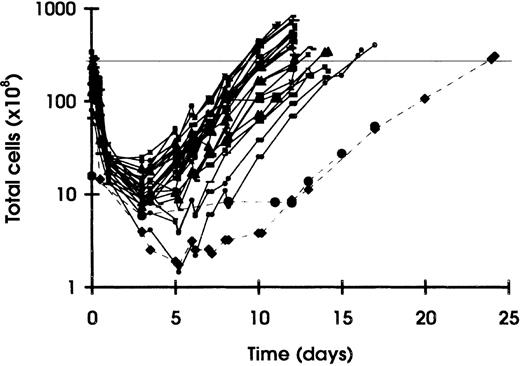
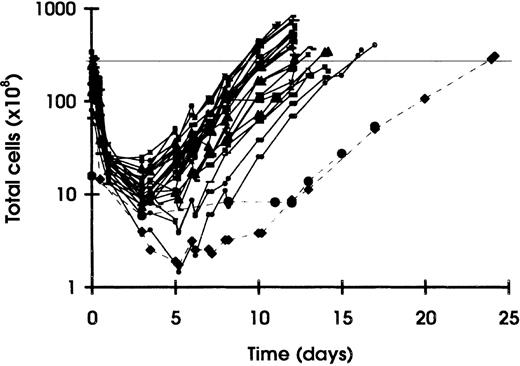
CD4ζ-modified T cells were successfully processed and released in 24 of 25 patients. A total of 27 lymphapheresis products were processed, and the T-cell growth curves are shown in Figure1. Two patients underwent repeat apheresis because of initial culture failure, and 1 was successfully processed the second time. A common feature of the 3 failed cultures was a low lymphocyte content of the incoming apheresis products.
T-cell growth curves of 27 autologous CD4ζ-modified CD4+ and CD8+ T-cell products in 25 enrolled subjects.
The minimum starting cell count was 5 × 109. Transduction with CD4ζ retroviral supernatant occurred on days 5 and 7, followed by expansion in serum-free medium containing IL-2 (200 IU/mL) and antiretroviral agents until reaching the target cell dose of 3 × 1010 cells (horizontal line on chart). Cell processing was successful in 24 of 25 subjects (the 2 failed cultures are depicted with the dashed lines). Both patients underwent repeat lymphapheresis, and 1 was successfully processed the second time.
T-cell growth curves of 27 autologous CD4ζ-modified CD4+ and CD8+ T-cell products in 25 enrolled subjects.
The minimum starting cell count was 5 × 109. Transduction with CD4ζ retroviral supernatant occurred on days 5 and 7, followed by expansion in serum-free medium containing IL-2 (200 IU/mL) and antiretroviral agents until reaching the target cell dose of 3 × 1010 cells (horizontal line on chart). Cell processing was successful in 24 of 25 subjects (the 2 failed cultures are depicted with the dashed lines). Both patients underwent repeat lymphapheresis, and 1 was successfully processed the second time.
Characteristics of the 24 successful T-cell products are shown in Table2. Cells were expanded ex vivo for an average of 13 days, and all cultures were completed within 17 days. This yielded a mean of 4.2 × 1010 cells (range, 1.9-6.8 × 1010 cells). Average transduction efficiency as measured by PCR for CD4ζ was 19% and ranged from 5% to 57%. The average composition of the final T-cell products yielded a ratio of CD8 to CD4 T cells of approximately 3:1. Similar expansion of T cells from HIV-uninfected donors yields a higher proportion of CD4+ T cells with a ratio of approximately 1:1 (data not shown). Phenotypic analysis by flow cytometry revealed a high proportion of cells expressing CD62L and CD28, with intermediate expression of CD25. There was no clear association between the proportion of CD4+ T cells in the final product or transduction efficiency and patterns of in vivo survival of the gene-modified cells.
Toxicity
There were no serious adverse events reported, and T-cell infusions overall were associated with minimal toxicity (Table3). Grade 3 or 4 adverse events were predominantly associated with IL-2 infusion. The most common toxicities of grade 2 or higher seen in the cells-only arm were fever, chills, rash, and sinusitis (each seen in 2 patients). Shift-table analyses of safety laboratory parameters demonstrated an increase in white blood cells and eosinophils in all patients in the cells + IL-2 group and in 8 of 11 in the cells-only group during the first week following infusion. Cholesterol decreased in 20 of 22 patients and lactate dehydrogenase increased in 16 of 17 in both groups combined. All 24 subjects tested negative for RCR by PCR analysis for MLV env up to 1 year after infusion.
CD4ζ-modified T-cell survival in peripheral blood
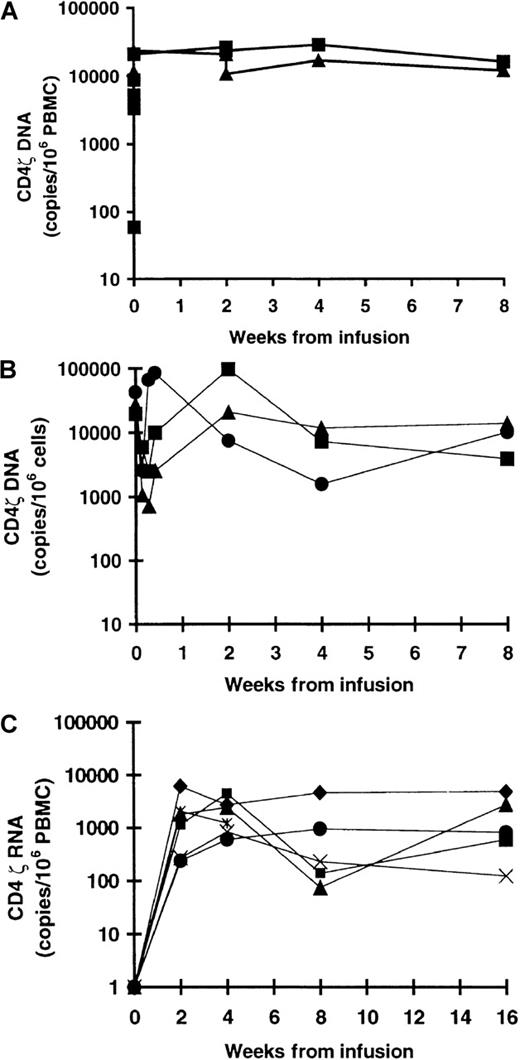
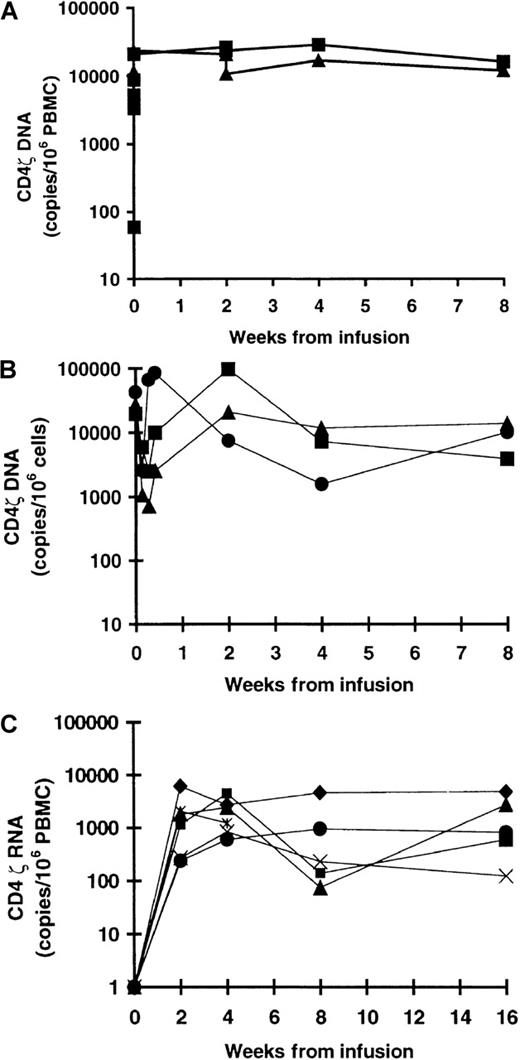
CD4ζ-modified T cells were detected by DNA PCR for the CD4ζ gene in the peripheral blood of all patients following infusion. Sustained mean levels of 4.0 to 4.4 log copies/106 cells (1% to 3% of PBMCs) were detected at all time points after infusion from day 3 through week 8 in both treatment arms (Figure2A). Extended follow-up through 12 months in 18 patients demonstrated sustained persistence of CD4ζ-modified T cells in the blood of 17 of 18, with mean values of 3.8 log copies (cells + IL-2) and 3.1 log copies (cells only) at 6 months, and 3.1 log copies (cells + IL-2) and 2.9 log copies (cells only) at 12 months. There were no statistically significant differences in survival of gene-modified T cells between the treatment arms. Fractionation of blood T cells was performed in 6 patients and demonstrated survival of both gene-modified CD4+ and CD8+ T cells in all patients analyzed (Figure 2B). In addition, CD4ζ RNA RT-PCR analysis was performed in 6 patients and confirmed relatively stable gene expression for at least 16 weeks (Figure 2C).
CD4ζ-modified T-cell survival and gene expression in peripheral blood mononuclear cells (PBMCs).
Gene-modified T-cell infusion was administered at week 0, and patients were followed for at least 8 weeks after infusion. (A) Survival of CD4ζ-modified T cells in peripheral blood as measured by quantitative DNA PCR analysis for CD4ζ in the cells only (▴) and cells + IL-2 (▪) treatment cohorts through 8 weeks of follow-up. There were no statistically significant differences between cohorts at any time point after infusion (P = .35, week 2; P = .49, week 4;P = .93, week 8). (B) Immunoselected populations of CD4+ (▪) and CD8+ (•) T cells in peripheral blood were analyzed for the presence of CD4ζ by DNA PCR and compared with the presence of CD4ζ in the bulk population (▴). The results confirmed the persistence of both gene-modified CD4+ and CD8+ T cells in 6 of 6 patients analyzed for at least 8 weeks. Results of 1 representative patient (J233) out of a total of 6 analyzed are shown. (C) Persistent, relatively stable expression of the CD4ζ gene was confirmed for at least 16 weeks by CD4ζ RNA RT-PCR analysis of PBMCs in 6 patients (G251, T253, Y254, Q202, Y292, and J233).
CD4ζ-modified T-cell survival and gene expression in peripheral blood mononuclear cells (PBMCs).
Gene-modified T-cell infusion was administered at week 0, and patients were followed for at least 8 weeks after infusion. (A) Survival of CD4ζ-modified T cells in peripheral blood as measured by quantitative DNA PCR analysis for CD4ζ in the cells only (▴) and cells + IL-2 (▪) treatment cohorts through 8 weeks of follow-up. There were no statistically significant differences between cohorts at any time point after infusion (P = .35, week 2; P = .49, week 4;P = .93, week 8). (B) Immunoselected populations of CD4+ (▪) and CD8+ (•) T cells in peripheral blood were analyzed for the presence of CD4ζ by DNA PCR and compared with the presence of CD4ζ in the bulk population (▴). The results confirmed the persistence of both gene-modified CD4+ and CD8+ T cells in 6 of 6 patients analyzed for at least 8 weeks. Results of 1 representative patient (J233) out of a total of 6 analyzed are shown. (C) Persistent, relatively stable expression of the CD4ζ gene was confirmed for at least 16 weeks by CD4ζ RNA RT-PCR analysis of PBMCs in 6 patients (G251, T253, Y254, Q202, Y292, and J233).
Antiviral activity of CD4ζ T cells
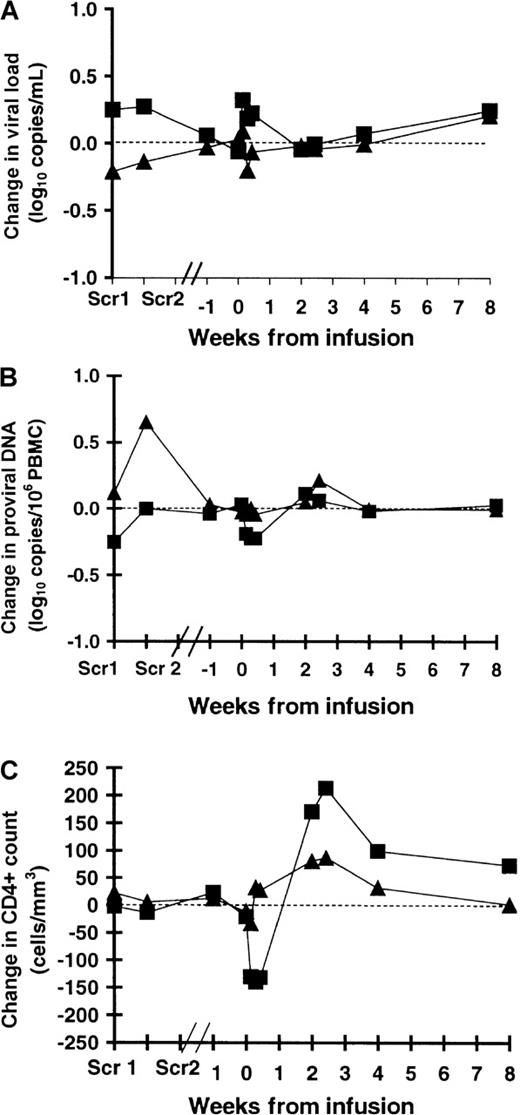
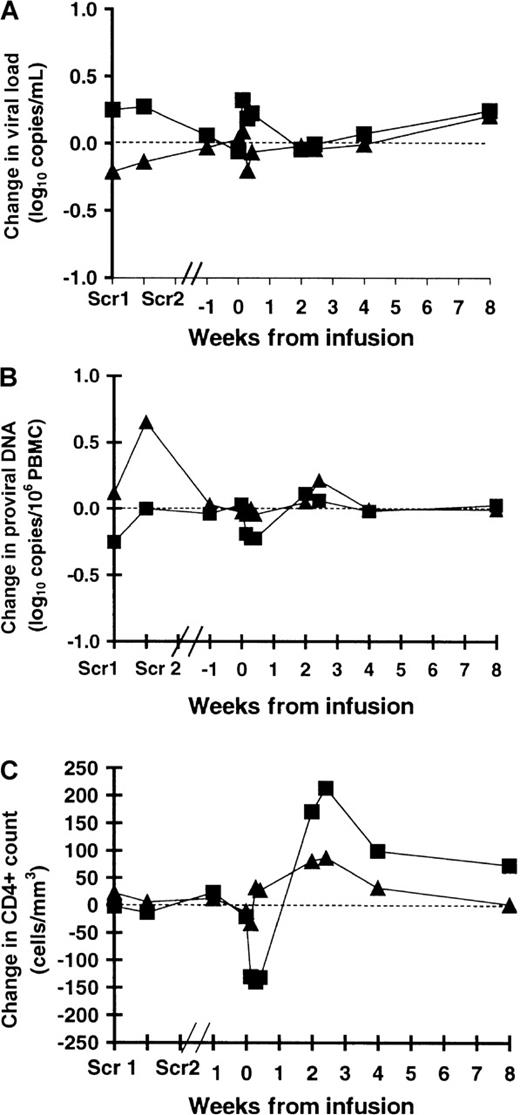
Antiviral activity of CD4ζ T-cell infusions administered with or without IL-2 was assessed through monitoring of plasma HIV viral load, blood HIV proviral DNA, CD4+ T-cell counts, and analysis of HIV reservoirs in rectal mucosa. A change in plasma viral load of greater than 0.5 log is unlikely to be explained by inherent biologic or assay variability and is accepted as a clinically relevant change in the level of plasma HIV RNA.39 There was no change in mean plasma viral load greater than 0.5 log at any time point after infusion in either treatment arm, and differences between arms were not statistically significant (Figure 3A). Two patients (8%; 95% confidence interval [CI], 1% to 27%) experienced a viral load decrease of 0.5 log or greater at week 2, 3 patients (23%; 95% CI, 3% to 34%) at week 4, and 1 patient (4%; 95% CI, 0 to 21%) at week 8, suggesting a transient antiviral effect of gene-modified T cells in a subset of patients. There was no statistically significant difference in the proportion of patients experiencing a 0.5 log or greater decrease in viral load between the treatment groups.
Antiviral activity and change in CD4+T-cell count following CD4ζ-modified T-cell infusion.
Baseline values represent an average of those at week −1 and week 0. T-cell infusion occurred at week 0, and postinfusion analyses were performed on days 1, 2, and 3 and weeks 2, 4, and 8. Scr1 and 2 represent the 2 screening values performed approximately 8 weeks before cell infusion. (A) Mean change from baseline in plasma HIV RNA (Roche Amplicor kit; sensitivity 40 copies/mL). There were no statistically significant differences between the cells only (▴) and cells + IL-2 (▪) cohorts at any time point after infusion (P = .87, week 2; P = .70, week 4; P = .86, week 8). (B) Mean change from baseline in blood HIV proviral DNA (DNA PCR for HIVgag, Specialty Labs; sensitivity 35 copies/106cells). There were no statistically significant differences between the cells only (▴) and cells + IL-2 (▪) cohorts at any time point after infusion (P = .84, week 2; P = .94, week 4; P = .89, week 8). (C) Mean change from baseline in CD4+ T-cell count. There was a trend toward a greater increase in CD4+ T-cell counts after infusion in the cells + IL-2 arm (▪) compared with the cells-only arm (▴) (P = .04, week 2; P = .14, week 4;P = .10, week 8).
Antiviral activity and change in CD4+T-cell count following CD4ζ-modified T-cell infusion.
Baseline values represent an average of those at week −1 and week 0. T-cell infusion occurred at week 0, and postinfusion analyses were performed on days 1, 2, and 3 and weeks 2, 4, and 8. Scr1 and 2 represent the 2 screening values performed approximately 8 weeks before cell infusion. (A) Mean change from baseline in plasma HIV RNA (Roche Amplicor kit; sensitivity 40 copies/mL). There were no statistically significant differences between the cells only (▴) and cells + IL-2 (▪) cohorts at any time point after infusion (P = .87, week 2; P = .70, week 4; P = .86, week 8). (B) Mean change from baseline in blood HIV proviral DNA (DNA PCR for HIVgag, Specialty Labs; sensitivity 35 copies/106cells). There were no statistically significant differences between the cells only (▴) and cells + IL-2 (▪) cohorts at any time point after infusion (P = .84, week 2; P = .94, week 4; P = .89, week 8). (C) Mean change from baseline in CD4+ T-cell count. There was a trend toward a greater increase in CD4+ T-cell counts after infusion in the cells + IL-2 arm (▪) compared with the cells-only arm (▴) (P = .04, week 2; P = .14, week 4;P = .10, week 8).
The mean change from baseline in blood HIV proviral DNA did not exceed 0.10 log in either treatment arm during the 8-week observation (Figure3B). However, the HIV proviral DNA assay used in this trial measures total HIV DNA including integrated, unintegrated, and replication-incompetent copies and may not, therefore, accurately reflect changes in replication-competent HIV proviral DNA.
Figure 3C shows the mean change from baseline in the CD4+cell counts in the 2 treatment arms. CD4+ counts decreased transiently in the cells + IL-2 arm during the first 3 days following T-cell infusion (concomitant with IL-2 infusion), which is consistent with transient lymphopenia induced by IL-2 (C. Lane, personal communication). There was an increase in CD4+ counts in both treatment arms at week 2; however, this increase was sustained only in the cells + IL-2 arm at week 8, with a mean increase of 73 cells/μL (95% CI, 19-127). This is consistent with the expected effect of IL-2 alone.40 The difference between treatment arms at week 8 was of borderline statistical significance (P = .10, nontransformed CD4+ cell count;P = .07, log-transformed CD4+ cell count).
CD4ζ T-cell trafficking and activity against gut-associated HIV reservoirs
The gut-associated lymphoid tissue (GALT) serves as an important and accessible tissue reservoir of HIV-infected cells. Five of 6 eligible patients (3 receiving cells only; 2 receiving cells + IL-2) participated in a substudy to investigate the trafficking and antiviral activity of CD4ζ-modified T cells against rectal tissue reservoirs of HIV. All 5 completed the planned rectal biopsy procedures (week −1; days 3, 7, and 14), and there were no procedure-related adverse events.
CD4ζ signal was measured in PBMCs, bulk tissue, and isolated lamina propria lymphocytes (LPLs) by PCR (Table4). CD4ζ signal was consistently detected in whole biopsy tissue samples in all patients at all time points (mean 2.6 log copies/106 tissue cells). The mean CD4ζ signal in blood for these 5 subjects over the 14-day observation period was 4.1 log copies/106 PBMCs. Long-term follow-up demonstrated persistent CD4ζ signal in rectal tissue in 2 of 3 subjects at 1 year. CD4ζ signal in the rectal biopsy specimens was consistently lower than that in peripheral blood. This could reflect the difference in the denominator (fractionated lymphocytes versus bulk tissue), the kinetics of trafficking to the gut mucosa, or loss of signal associated with sample processing. All subjects showed an increase in CD4ζ signal in bulk rectal tissue from day 3 to day 7. Detection of CD4ζ in isolated LPLs was less reproducible; however, signal was detected in LPLs from every patient at 1 or more time points after infusion. These data are consistent with the trafficking of gene-modified T cells to rectal lymphoid tissue in all 5 patients with maintenance of CD4ζ signal for at least 14 days.
Rectal tissue–associated HIV RNA load was measured by HIV RNA RT-PCR analysis (Table 4). The mean tissue viral load decreased from the preinfusion value by at least 0.5 log copies/μg RNA at all time points after infusion. Four of 5 patients showed a 0.5 log or greater decrease at 2 of 3 time points, and 2 of 5 showed a 0.5 log or greater decrease at all measured time points. Three patients had a 1.0 log or greater decrease in tissue HIV RNA at 1 or more time points after infusion. These preliminary data suggest antiviral activity of CD4ζ-modified T cells against gut-associated reservoirs of HIV. There were too few patients to assess the impact of concomitant IL-2 administration; however, both tissue trafficking and antiviral activity were demonstrated in patients in both treatment arms. The duration of this effect and verification of these results will require further study.
Measurement of plasma-associated HIV RNA did not follow the same trend as seen in HIV RNA in the gut tissue in these 5 patients (Table 4). There was no significant mean change (> 0.5 log copies/mL) in plasma viral load during the 14-day observation period; however, 1 of 5 patients showed an isolated decrease in plasma viral load of at least 0.5 log at day 7.
Discussion
We have developed a rapid T-cell manufacturing process that reliably yields 2 to 3 × 1010 gene-modified T cells within 2 weeks. This process was successful in 24 of 25 enrolled patients and yielded a mixed population of CD4+ and CD8+ T cells with an activated cell phenotype (high expression of CD28, CD25, and CD62L). Bulk transduction efficiency in this trial was approximately 20% and, with further processing improvements, has been increased to 40%.41 This high-level transduction eliminates the need for posttransduction purification of gene-modified cells, allowing for the brief period of ex vivo expansion.
CD4ζ-modified CD4+ and CD8+ T cells persisted in the blood of all patients at high levels (1% to 3% of PBMCs) throughout the 8-week observation period, and extended follow-up demonstrated maintained survival for at least 1 year in 17 of 18 subjects (0.1% of PBMCs). This long-term persistence is in marked contrast to our previous experience with infusion of syngeneic CD4ζ-modified CD8+ T cells in HIV-infected twin pairs as well as the previously published experience with adoptive T-cell therapy in HIV infection reported by other groups. In the syngeneic twin study, gene-modified CD8+ T cells were purified and expanded in IL-2 for a mean of 62 days. Peak circulating levels of CD4ζ-modified T cells of 1% to 10% of PBMCs were observed at 48 hours, followed by a 2- to 3-log decrease within 8 weeks of adoptive transfer (manuscript submitted). Infusion of autologousneo-marked HIV gag-specific CD8+ T cells by another group showed similarly poor survival patterns, withneo-marked cells constituting 2% to 3.5% of CD8+T cells in blood 1 day after infusion (3.3 × 109cells/m2), and with a rapid decline to fewer than 5 cells per 106 PBMCs by 3 weeks.24 The most likely explanation for the improved T-cell survival, independent of exogenous IL-2, seen in this trial is a helper effect conferred by CD4ζ-modified CD4+ T cells. However, changes in ex vivo T-cell stimulation and/or the shorter total duration of ex vivo cell culture (mean of 13 versus 62 days) may also have played a role. This high-level, sustained, IL-2–independent survival of gene-modified autologous T cells validates this approach as a platform technology for gene delivery.
The T-cell culture method used in this study provided costimulation of CD4+ and CD8+ T cells by antibodies to CD3 and CD28 co-immobilized on magnetic beads. This differs from the original twin study in which single signal T-cell stimulation of purified CD8+ T cells with anti-CD3 and high-dose IL-2 was employed. This new cell culture method allows ex vivo proliferation of CD4+ T cells and renders CD4+ T cells resistant to infection with M-tropic strains of HIV through down-regulation of the HIV fusion coreceptor CCR5.31,42 In preclinical experiments at Cell Genesys, this method generated T cells that were resistant to antigen-induced apoptosis, whereas CD3/IL-2–stimulated cells died rapidly following repeated rounds of stimulation through the CD4ζ receptor. Furthermore, this new process generated CD4+ T cells capable of proliferation and IL-2 secretion upon CD4ζ receptor engagement. Gene-modified CD4+ and CD8+ T cells showed equivalent cytolytic activity against HIV env–bearing targets and equivalent potency in suppression of HIV replication in infected T-cell cultures as CD8+ T cells alone cultured using anti-CD3/IL-2.43 The markedly improved, sustained, high-level in vivo survival of both gene-modified CD4+ and CD8+ T cells in this trial is consistent with these preclinical observations and suggests that mixed CD4+and CD8+ T-cell populations provide HIV-specific T-helper function.
Preliminary evidence of antiviral activity of CD4ζ-modified CD4+ and CD8+ T cells was observed in this trial. Although there was no significant mean change, several patients experienced a plasma viral load decrease of greater than 0.5 log on at least 1 occasion, suggesting a transient antiviral effect in a subset of patients. Furthermore, a greater than 0.5 log mean decrease in rectal mucosa–associated HIV RNA was detected from days 3 through 14 in a subset of 5 patients who underwent serial rectal biopsies, suggesting antiviral activity against this important tissue reservoir of HIV. This antiviral effect correlated with detection of CD4ζ-modified T cells in the rectal tissue of all 5 patients throughout the 14-day monitoring period, with increasing signal from day 3 to day 7. Possible explanations for the discordance between changes in gut and plasma viral loads include true compartment differences in the activity of gene-modified T cells, differences in the kinetics of activity between the compartments, or insufficient magnitude of effect in the gut compartment to be reflected in plasma viral load. Expression of the β7 integrin subfamily of adhesion molecules has been shown to be critically important for lymphocyte trafficking to GALT, and the formation of GALT is severely impaired in mice deficient for this receptor family.44 Subsequent experiments have confirmed the expression of α4β7 on CD4ζ-modified T cells at the end of ex vivo cell culture (unpublished data). The gastrointestinal tract contains most of the lymphoid tissue in the body and has been shown to be a major target for SIV replication and CD4+ T-cell loss in early SIV replication following intravenous inoculation in Rhesus macaques.45 Therefore, demonstration of antiviral activity against this tissue reservoir of HIV is likely to be important in the evaluation of novel agents. We did not investigate lymph node trafficking of CD4ζ-modified T cells in this study; however, another group has demonstrated accumulation ofneo-marked HIV-specific CD8+ T cells adjacent to infected CD4+ T cells in lymph nodes, confirming the ability of adoptively transferred lymphocytes to migrate to this lymphoid reservoir.24
The results of this clinical trial validate the feasibility of adoptive immunotherapy of HIV infection with genetically modified, MHC-unrestricted, polyclonal T cells bearing chimeric HIVenv–specific immune receptors and provide preliminary evidence of tissue homing and antiviral activity against tissue reservoirs of HIV. Our belief, based on the experience in adoptive T-cell immunotherapy of cancer, is that this therapy is most likely to demonstrate convincing clinical efficacy in subjects with minimal viral burden. Among patients receiving donor lymphocyte infusions for relapsed chronic myelogenous leukemia following bone marrow transplantation, remissions are most frequent in patients with cytogenetic or early hematologic relapse and less common in patients with advanced disease.46 We have therefore initiated a randomized controlled clinical trial of CD4ζ-modified versus -unmodified T cells in 40 HIV-infected subjects with undetectable plasma viral loads taking combination antiretroviral therapy to measure the efficacy of this gene therapy against residual blood and tissue reservoirs of HIV.
Acknowledgments
We would like to acknowledge the following people for their contributions to this study: Judith Carden, Alison Leiblein, Julie Elliott, Dorie Heeren, Walter Howard, Kathleen Shea, Virginia Waite, Janet Wittes, Lynne Fitch, and David Broad.
Supported by Cell Genesys Inc in collaboration with Hoechst Marion Roussel. P.A.A. was supported in part by Mucosal Immunology CORE Grant no. AI28697, University of California, Los Angeles. This work was carried out in part in the General Clinical Research Centers at the following institutions: University of California, Los Angeles (RR-00865), San Francisco General Hospital (5-MO1-RR00083-37), and University of Colorado Health Science Center (RR-00051).
Reprints:Kristen M. Hege, Cell Genesys, Inc, 342 Lakeside Dr, Foster City, CA 94404; e-mail: kristenh@cellgenesys.com.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.