Abstract
The human multidrug resistance-1 (MDR1) gene product, P-glycoprotein (P-gp), is well known for its ability to confer drug resistance; however, recent evidence suggests that P-gp expression can have more general effects on cellular development. In support of this idea, it was previously shown that retroviral-mediated MDR1 expression in murine bone marrow cells resulted in the expansion of stem cells in culture and in the development of a myeloproliferative syndrome in transplanted mice. It is now reported that MDR1-mediated stem cell expansion is associated with an increase in side population (SP) stem cells, defined by Hoechst dye staining. Transduction of murine bone marrow cells with an MDR1 retroviral vector resulted in an almost 2 log increase in SP cell numbers over 12 days in culture, whereas there was a rapid loss of SP cells from control cultures. Stem cell amplification was not limited to ex vivo expansion cultures but was also evident when MDR1-transduced cells were directly transplanted into irradiated mice. In these cases, stem cell expansion was associated with relatively high vector copy numbers in stem cell clones. As previously reported, some cases were associated with a characteristic myeloproliferative syndrome. A functionally inactive MDR1 mutant cDNA was used to show that P-gp pump function was required both for amplification of phenotypically defined SP cells and functionally defined repopulating cells. These studies further support the concept that ABC transporter function can have important effects on hematopoietic stem cell development.
The human MDR1 gene and its murine homologs were originally identified based on the ability of their expressed products, collectively referred to as P-glycoproteins (P-gp), to extrude various cytotoxic drugs from the cell interior.1,2 It is now known that the MDR1 gene belongs to a superfamily of transport proteins that contain ATP-binding cassette (ABC) regions necessary for pump function. Many studies have clearly shown that P-gp expression plays an important role in the resistance of human tumor cells to cancer chemotherapy.3 Considering that P-gp is also expressed in numerous normal tissues, more recent studies have examined the normal physiologic functions of MDR1-like genes. Murine gene disruption experiments have demonstrated that P-gp expression is necessary for biliary excretion,4 maintenance of the blood–brain barrier,5 and elimination of drugs.6 P-gp can also mediate more general cellular functions, including the translocation of lipids across the cell membrane7and the modulation of specific apoptosis pathways.8 9
P-gp is expressed in many hematopoietic cell types,10including human CD34+ stem cells11 and murine c-kit+ stem cells.12 Several lines of evidence suggest that P-gp expression is functionally conserved in hematopoietic stem cells. Hematopoietic stem cells can be identified based on their ability to efflux fluorescent dyes that are substrates for P-gp, such as rhodamine (Rho) 12313-16 and Hoechst 33342.17-19 One particular approach for purifying stem cells is based on Hoechst dye staining of bone marrow cells to identify a minor fraction of side population (SP) cells highly enriched for repopulating activity.20 This SP phenotype identifies a primitive subset of stem cells in multiple mammalian species21 that, based on verapamil inhibition studies, may result from the expression of P-gp or another ABC transporter.20
Transport activity in hematopoietic stem cells suggests the possibility that ABC transporters such as MDR1 could have a functional role in stem cell regulation. Further support of this hypothesis is derived from our previous studies of MDR1 overexpression in murine hematopoietic stem cells. These studies show that enforced expression of the MDR1 gene, achieved using a retroviral vector, resulted in marked expansion of repopulating stem cells during 12 days of culture in cytokine-containing media.22 Some mice transplanted with these cells developed a myeloproliferative syndrome phenotypically resembling chronic myelogenous leukemia, demonstrating that dysregulated P-gp expression can adversely affect hematopoietic development.
The goal of the current study was to further explore the effect of MDR1 gene expression on stem cell development. Considering the link between SP stem cells and transporter function, we first asked whether MDR1-mediated stem cell expansion was associated with an increase in SP stem cells in expansion cultures. We also determined whether stem cell expansion was limited to ex vivo culture conditions. For instance, the mechanism of stem cell expansion could result from the efflux of some media component that had negative effects on stem cell proliferation. An alternative and more interesting possibility is that MDR1 gene expression could be acting at a more global level independent of ex vivo culture conditions. To distinguish between these possibilities, we tested whether freshly transduced stem cells would have a direct proliferative advantage in vivo after transplantation. Lastly, experiments were performed to determine whether these stem cell effects required the efflux-pump activity of P-gp or whether the effects could be caused by other properties of the experimental system. A vector encoding an expressed but functionally dead P-gp was tested in both the SP cell expansion assay and in vivo competitive repopulation assays. Together, these studies provide further evidence that enforced ABC transporter function can alter the proliferative and developmental fate of hematopoietic stem cells.
Materials and methods
Vector constructs and producer cell lines
The HaMDR1 retroviral vector was constructed using the Harvey (Ha) murine sarcoma virus backbone, as has been previously described.22 Note that this MDR1 cDNA differs from an earlier vector23 in that the sequence for codon 185 has been changed to encode for a glycine residue, and aberrant splicing sites12 have been modified by 2 point substitutions in the wobble positions of codons 139 and 733.24 All ecotropic producer cell lines were generated in the GP+E86 packaging cell line25 using previously described methods26 and were shown to be free of replication-competent retrovirus by both polymerase chain reaction and marker rescue assays. The biologic titer of the HaMDR1 ecotropic retrovirus was 2 × 105particles/mL supernatant as determined by infection of the 3T3 cells and quantitation of the MDR1 transduction by Rho 123 efflux and by antibody staining (see below). The HaDHFRL22Y vector was used as a control and expressed an antifolate-resistant variant of the human dihydrofolate reductase gene, as has been previously described.27
The “pump dead” MDR1 vector (HaMDR1Δ34) used a mutant MDR1 cDNA encoding a 34-amino acid deletion in the linker region between the 2 ABC regions28 (a gift from Dr M. M. Gottesman, Bethesda, MD). This mutant cDNA was modified to eliminate potential aberrant mRNA splicing and to encode for glycine at codon 185, as described above, and then inserted into the Harvey murine sarcoma vector backbone. A polyclonal population of ecotropic producer cells was derived by transducing GP+E86 cells with a transient supernatant derived from transfected 293T cells. Vector-transduced producer cells were then isolated by cell sorting for surface P-gp expression, as described below. The 4E3 antibody staining procedure was also used to titer the polyclonal HaMDR1Δ34 vector supernatants on 3T3 cells, and it showed a titer of 2 × 105 particles/mL.
4E3 antibody and rhodamine 123 staining
Producer cells were analyzed for P-gp expression by staining with a monoclonal mouse antihuman P-glycoprotein antibody (clone 4E3; DAKO, Carpinteria, CA). Adherent cells were trypsinized and resuspended in 50 μL phosphate-buffered saline (PBS) containing 2% bovine serum albumin (BSA) and 0.1% NaN3. Then 5 μL 4E3 antibody was added, incubated at room temperature for 30 minutes, washed twice with PBS, and resuspended in 50 μL PBS containing 2% BSA and 0.1% NaN3. After the primary antibody staining, 5 μL phycoerythrin-conjugated, rabbit antimouse antibody (DAKO) was added as a secondary stain. The cells were then incubated at room temperature for 30 minutes, washed twice with PBS, and resuspended in PBS for FACS analysis.
Rho 123 staining was achieved by trypsinizing cells, resuspending the cells in Dulbecco's modified Eagle's medium (DMEM) medium containing 10% fetal calf serum at a concentration of 1 × 106cells mL, and adding Rho123 (Sigma) at a final concentration of 1 μg/mL. The cells were then incubated at 37°C for 1 hour in the dark, washed once with 10 mL PBS, and resuspended in DMEM/10% fetal calf serum. Then they were incubated at 37°C for 1 hour to allow for efflux, spun down, and then resuspended in 1 mL PBS for FACS analysis.
Retroviral-mediated gene transfer into murine hematopoietic stem cells
Bone marrow cells were harvested from C57BL/6 or B6.Ch-1<b>/By (referred to as HW80) congenic mouse strains (Jackson Laboratories, Bar Harbor, ME) by standard methods. After isolation, cells were placed in liquid suspension culture in DMEM (BioWhittaker, Walkersville, MD) with 1% penicillin/streptomycin (Gibco/BRL, Grand Island, NY), 15% fetal bovine serum (FBS; Hyclone, Logan, UT), 20 ng/mL murine interleukin (IL)-3 (R & D Systems, Minneapolis, MN), 50 ng/mL human IL-6 (Amgen, Thousand Oaks, CA), and 50 ng/mL murine stem cell factor (R & D Systems). The cells were initially plated at 1 × 106cells/mL in 10 mL medium. After prestimulation for 48 hours, cells were replated onto confluent monolayers of irradiated ecotropic producer cell lines. The bone marrow cells were plated at the same density used in the prestimulation phase and in the same medium with 6 μg/mL polybrene added. Coculture with producer cells was continued for 48 hours and was followed by the harvesting of bone marrow cells. A small sample of bone marrow cells was plated into methylcellulose to score drug-resistant myeloid progenitors. Using the HaDHFRL22Yvector, 68% to 71% of progenitors were resistant to trimetrexate, and using the HaMDR1 vector, 47% to 62% of progenitors were resistant to Taxol (n = 2 for both vectors), at drug concentrations that killed 100% of control colonies.
Bone marrow expansion cultures
Expansion cultures were initiated immediately after the coculture phase of transduction, which was designated as day 0 of expansion. Nonadherent bone marrow cells were gently removed by pipetting off the medium, and the producer cells were washed twice with 5 mL PBS. During these steps, care was taken not to disrupt the producer cell layer. Cells were then centrifuged, media were removed, and the cells were replated in suspension culture dishes at a total of 1 × 107 cells in 10 mL medium.22 The medium used for expansion was DMEM supplemented with 15% heat-inactivated fetal calf serum; in some experiments, it was supplemented with a commercially available preparation of BSA, insulin, and soluble transferrin (BIT; Stem Cell Technologies, Vancouver, Canada). The medium also contained 20 ng/mL murine IL-3, 50 ng/mL human IL-6, and 50 ng/mL murine stem cell factor (SCF). Cells were cultured in nontreated suspension dishes (Corning, Corning, NY) and grown in 5% CO2 at 37°C in a standard humidified tissue culture incubator. Cells were split on days 3, 6, and 9 and re-seeded at 1 × 106 cells/mL in 10 mL.
Hoechst 33342 SP cell assay
Murine bone marrow cells were collected and resuspended at 1 × 106 cells/mL in DMEM plus 10 mmol/L HEPES and 2% FBS. In a water bath, the cells were allowed to equilibrate at 37°C, and 5 μg/mL Hoechst 33342 (Fisher Scientific, Pittsburgh, PA) was added for 90 minutes as previously described.20 Cells were then centrifuged at 4°C and resuspended in ice-cold Hanks' balanced salt solution plus 10 mmol/L HEPES and 2% FBS at 1 × 107cells/mL. For flow cytometric analysis or sorting, a Becton Dickinson (San Jose, CA) FACS Vantage flow cytometer was configured for dual-emission wavelength analysis as previously described.20 Cells were gated based on forward and side light scatter to exclude debris. For experiment 2 with the HaMDR1Δ34 vector, propidium iodide staining (2 μg/mL) was used to derive a gate excluding dead cells. Cells were analyzed at approximately 5000 cells/s until data from 1 × 106cells were collected. The SP cell gate was defined based on normal fresh C57BL/6 bone marrow cells.
Analysis of sorted Hoechst 33342 SP cells for stem cell activity
Sorted SP cells were collected in 100 μL FBS. For limiting dilution analyses, sorted SP cells from C57BL/6 mice were mixed with 2 × 105 fresh normal bone marrow cells from congenic HW80 mice to rescue mice from lethal irradiation (11 Gy; cesium 137 Cs source). Both hemoglobin electrophoresis29 and PCR of peripheral blood leukocytes for MDR1 vector sequences were performed to assay for reconstitution in mice 16 weeks after transplantation. The P7 and P8 PCR primers and conditions used have been previously described.12
Transplants and competitive repopulation assays
Donor bone marrow cells were mixed at the indicated ratios and injected into the tail veins of HW80 recipient mice that had been lethally irradiated with 11 Gy using a 137Cs γ-irradiator. Peripheral blood was obtained by retro-orbital bleeding in anesthetized mice at varying time points after reconstitution and analyzed by hemoglobin electrophoresis or DNA PCR. Hemoglobin electrophoresis was performed on cellulose acetate plates as previously described29 using a commercially available kit (Helena Laboratories, Beaumont, TX). For PCR, genomic DNA was isolated from the circulating leukocytes in 70 μL blood using the InstaGene Genomic DNA kit (Bio-Rad, Hercules, CA) and resuspended in 20 μL water. One microliter of the DNA solution was amplified using a commercially available kit (Qiagen, Valencia, CA) and the following parameters: 35 cycles, 94°C X 1′, 60°C X 1′, 72°C X 1′. PCR primers used to amplify fragments from the HaMDR1and HaMDR1Δ34 vectors were 5′ CCACGTCAGCCTTGGACACA 3′ and 5′ GCCGCTTGGTGAGGATCTCT 3′.
Results
Expansion of MDR1-transduced SP cells during ex vivo culture
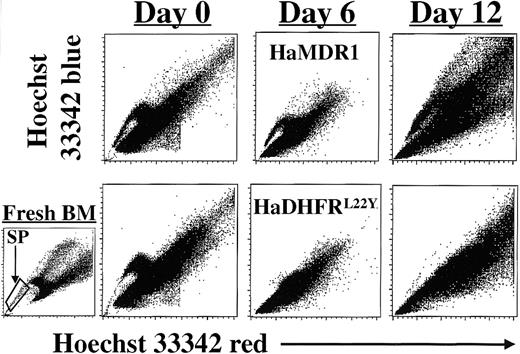
To determine whether enforced P-gp expression would result in an increase in SP cell numbers during ex vivo expansion cultures, murine bone marrow (BM) cells were transduced with the HaMDR1 retroviral vector22 and cultured for 12 additional days in media containing fetal calf serum, IL-3, IL-6, and SCF. As a control, cells were transduced with a vector expressing a human dihydrofolate reductase gene (HaDHFRL22Y) within the same vector backbone.27 SP cells were quantitated by Hoechst 33342 staining and flow cytometry after 0, 6, or 12 days of culture (Figure1). In populations of cells transduced with the HaDHFRL22Y vector, a loss of cells in the lower part of the SP tail, corresponding to stem cells with long-term repopulating activity,21 had already occurred immediately after the transduction procedure (day 0). After an additional 6 days of expansion, SP cells were no longer detectable in these control cultures. In contrast, cultures of cells that were transduced with the HaMDR1 vector showed preservation of SP cell numbers at early time points, with an increase in the absolute number of SP cells averaging 187-fold (n = 3; SE = 161; range, 38- to 380-fold) after 12 days of ex vivo culture. These data show that although SP cells were lost over time in extended BM cultures, enforced expression of the MDR1 gene resulted in a large amplification of SP cells in a 12-day period.
Quantitation of Hoechst 33342 SP cells in bone marrow expansion cultures after MDR1 gene transfer.
Murine bone marrow cells were prestimulated for 48 hours in the presence of growth factors and then retrovirally transduced with either the HaMDR1 or the HaDHFRL22Y vector for another 48 hours. The time point immediately after coculture was defined as day 0 of expansion. Transduced cells were then grown in suspension cultures for 12 days. Hoechst 33342 staining of BM cells was performed on days 0, 6, and 12 to determine the frequency of SP cells within the expanding cell populations. FACS profiles, representative of 3 independent expansion experiments, are shown for BM cells transduced with either the HaMDR1 (top panels) or the HaDHFRL22Y vectors (bottom panels). On the left, a sample of normal, freshly isolated C57BL/6 BM cells is shown with the SP gate indicated.
Quantitation of Hoechst 33342 SP cells in bone marrow expansion cultures after MDR1 gene transfer.
Murine bone marrow cells were prestimulated for 48 hours in the presence of growth factors and then retrovirally transduced with either the HaMDR1 or the HaDHFRL22Y vector for another 48 hours. The time point immediately after coculture was defined as day 0 of expansion. Transduced cells were then grown in suspension cultures for 12 days. Hoechst 33342 staining of BM cells was performed on days 0, 6, and 12 to determine the frequency of SP cells within the expanding cell populations. FACS profiles, representative of 3 independent expansion experiments, are shown for BM cells transduced with either the HaMDR1 (top panels) or the HaDHFRL22Y vectors (bottom panels). On the left, a sample of normal, freshly isolated C57BL/6 BM cells is shown with the SP gate indicated.
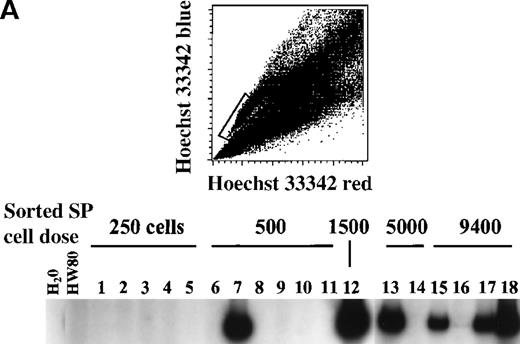
Repopulating activity in 12 day-expanded, sorted SP cells
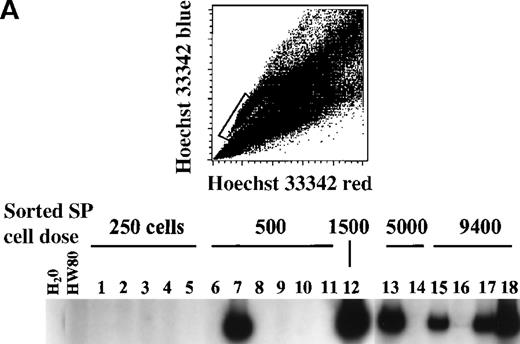
To determine whether repopulating cells were present and enriched within the expanded SP population, we performed limiting dilution transplantation experiments in irradiated mice using sorted SP cells. Control experiments with normal, fresh BM cells showed reconstitution with SP cell doses as low as 250 cells (data not shown), consistent with previously reported values.20 The repopulating cell frequency in the MDR1-transduced SP cell population was determined by transducing C5BL/6 BM cells with the HaMDR1 vector, expanding transduced cells for 12 days, and sorting for SP cells by flow cytometry. These sorted SP cells were injected into lethally irradiated recipient mice along with 2 × 105 fresh BM cells (HW80 background); the latter were used to confer radioprotection to the mice. Reconstitution analysis was performed 16 weeks after transplantation using a PCR assay to detect HaMDR1 vector sequences in total peripheral blood leukocyte DNA. Reconstitution was also studied using hemoglobin electrophoresis to determine the relative erythroid contributions arising from sorted SP cells.
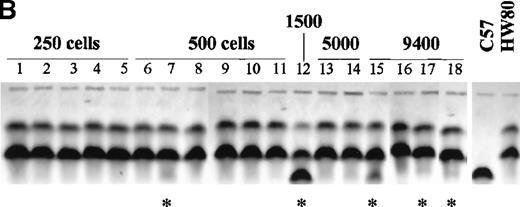
The PCR assay showed repopulation of recipient mice with SP cell doses as low as 500 cells, and vector-marked cells were present in most mice receiving between 1500 and 9400 expanded SP cells (Figure2A). Usually, hemoglobin electrophoresis also showed contributions from the expanded SP cells derived from the C57BL/6 background; however, the percentage contribution was very low in most mice (Figure 2B). These data suggested that the expanded SP cell population may be somewhat enriched for repopulating cells relative to whole BM but that the frequency of repopulating cells in the expanded SP population is significantly less than that in fresh SP cells from normal bone marrow. The low degrees of chimerism for the expanded SP cells could reflect a limited repopulation capacity of the expanded cells or simply a greater number of stem cells in the fresh HW80 graft used to provide radioprotection. This relative decrease in the concentration of repopulating cells in the expanded SP population suggested that a significant proportion of the expansion resulted from a phenotypic change in the cells without a corresponding change in repopulation potential. This interpretation is consistent with our previous results showing that the absolute numbers of functionally defined repopulating cells increased 12- to 30-fold in MDR1-transduced whole bone cultures,22 though in this study the absolute number of SP cells increased approximately 180-fold during the same culture period.
Limiting-dilution transplant analysis of MDR1-transduced SP cells isolated from 12-day expansion cultures.
HaMDR1-transduced BM cells (C57BL/6 background) were placed in liquid suspension culture and expanded for 12 days. On day 12, the SP cell fraction was isolated by flow cytometry using the sorting gate shown in A. The sorted cells were then injected into lethally irradiated recipient mice at the indicated doses, along with a 2 × 105 fresh BM cells (HW80 background). (A) 16 weeks after transplantation, peripheral blood leukocyte DNA was prepared and analyzed by PCR for the presence of the HaMDR1 proviral genome. A water-only control and a nontransplanted mouse control (HW80) are shown on the left as negative controls. Transplanted mice received cell doses ranging from 250 to 9400 cells, as indicated above the lanes. The numbers 1 to 18 correspond to individual recipient mice. (B) Reconstitution was also measured using hemoglobin electrophoresis. Erythroid cells derived from the sorted SP cells are identified by the faster-migrating, C57BL/6-derived hemoglobin isoform. The animal numbers are the same as in A, and samples from nontransplanted C57BL/6 and HW80 mice are shown on the right. Asterisks indicate samples in which there were detectable amounts of C57BL/6-derived hemoglobin.
Limiting-dilution transplant analysis of MDR1-transduced SP cells isolated from 12-day expansion cultures.
HaMDR1-transduced BM cells (C57BL/6 background) were placed in liquid suspension culture and expanded for 12 days. On day 12, the SP cell fraction was isolated by flow cytometry using the sorting gate shown in A. The sorted cells were then injected into lethally irradiated recipient mice at the indicated doses, along with a 2 × 105 fresh BM cells (HW80 background). (A) 16 weeks after transplantation, peripheral blood leukocyte DNA was prepared and analyzed by PCR for the presence of the HaMDR1 proviral genome. A water-only control and a nontransplanted mouse control (HW80) are shown on the left as negative controls. Transplanted mice received cell doses ranging from 250 to 9400 cells, as indicated above the lanes. The numbers 1 to 18 correspond to individual recipient mice. (B) Reconstitution was also measured using hemoglobin electrophoresis. Erythroid cells derived from the sorted SP cells are identified by the faster-migrating, C57BL/6-derived hemoglobin isoform. The animal numbers are the same as in A, and samples from nontransplanted C57BL/6 and HW80 mice are shown on the right. Asterisks indicate samples in which there were detectable amounts of C57BL/6-derived hemoglobin.
Expansion of MDR1-transduced stem cells in vivo
To determine whether the MDR1 vector was having a direct effect on stem cell proliferation or whether the effect was specific to ex vivo expansion cultures, we tested whether MDR1-mediated stem cell expansion would also occur directly in vivo. Bone marrow cells were transduced with either the HaMDR1 or the HaDHFRL22Y vector, and these grafts were mixed immediately after transduction for competitive repopulation experiments. C57BL/6 BM cells were transduced with the HaMDR1 vector, and HW80 BM cells were transduced with the HaDHFRL22Y vector. After transduction, equal donor volumes from each graft were mixed and transplanted into lethally irradiated recipient mice. Mice received between 2.3 to 5.1 × 106 HaDHFRL22Y-transduced cells and between 1.8 to 2.5 × 106 HaMDR1-transduced cells. In one experiment, the recipient mice were divided into 2 cohorts. One group of mice received two 5-day courses of granulocyte–colony-stimulating factor (G-CSF)/SCF growth factor treatment during weeks 5 and 8 after transplantation, as has been described,30 and one group of mice was left untreated. Because treatment with these growth factors is known to cause a significant increase in stem cell content in vivo,30 we hypothesized that the treated mice might show an earlier outgrowth of the MDR1-transduced graft.
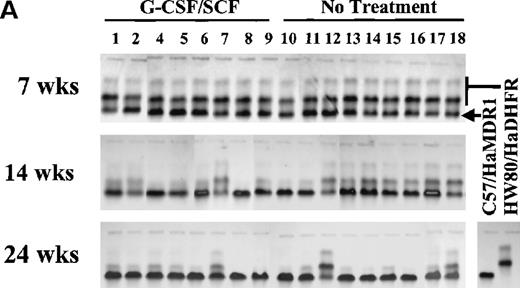
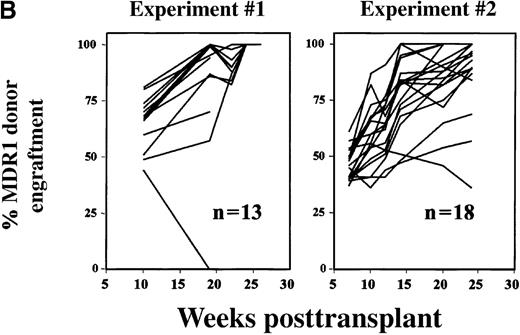
At 7 weeks after transplantation, hemoglobin reconstitution patterns uniformly reflected the input ratio of the grafts, with a roughly 50/50 mix of the 2 hemoglobin patterns (Figure3A). At later time points, mice from both groups showed a gradual increase in the proportion of erythroid cells derived from the MDR1-transduced graft. At 14 weeks after transplantation, the cytokine-treated group showed increased proportions of cells from the MDR1-transduced graft relative to the untreated group, but this did not reach statistical significance (P= .094). At 24 weeks this difference was no longer apparent, and the MDR1-transduced BM graft had completely overtaken the control graft in most cases. Data from 2 independent experiments are graphically shown in Figure 3B. Most mice showed a large and progressive shift toward MDR1-transduced donor cell engraftment over time. These experiments demonstrated that the capacity of MDR1 vectors to expand stem cells is not limited to the 12-day culture protocol.
Competitive repopulation assay in mice transplanted with equal donor volumes of HaMDR1- and HaDHFRL22Y-transduced BM cells.
BM cells from C57BL/6 mice were transduced with the HaMDR1 vector, and HW80 marrow cells were transduced with the HaDHFRL22Yvector. Immediately after the transduction, equal donor volumes from each transduced graft were mixed and transplanted into lethally irradiated recipient mice. Engraftment was monitored by tracking the proportion of donor hemoglobin specific for either the HaMDR1-transduced (lower band) or the HaDHFRL22Y-transduced (upper 2 bands) cells. (A) Hemoglobin electrophoresis gels are shown for mice from experiment 2, obtained at 7, 14, and 24 weeks after transplantation. These mice were divided into 2 groups. One received two 5-day courses of G-CSF/SCF treatment (left), and the other was the untreated group (right). Each lane represents a sample from a single mouse. The hemoglobin pattern for the C57BL/6 and HW80 controls are shown on the right. (B) Two independent mixing experiments were performed, and the data for both of these are graphically shown. The y-axis represents the percentage of donor engraftment with MDR1-transduced cells, as indicated by hemoglobin electrophoresis. Each line represents an individual mouse analyzed serially over time.
Competitive repopulation assay in mice transplanted with equal donor volumes of HaMDR1- and HaDHFRL22Y-transduced BM cells.
BM cells from C57BL/6 mice were transduced with the HaMDR1 vector, and HW80 marrow cells were transduced with the HaDHFRL22Yvector. Immediately after the transduction, equal donor volumes from each transduced graft were mixed and transplanted into lethally irradiated recipient mice. Engraftment was monitored by tracking the proportion of donor hemoglobin specific for either the HaMDR1-transduced (lower band) or the HaDHFRL22Y-transduced (upper 2 bands) cells. (A) Hemoglobin electrophoresis gels are shown for mice from experiment 2, obtained at 7, 14, and 24 weeks after transplantation. These mice were divided into 2 groups. One received two 5-day courses of G-CSF/SCF treatment (left), and the other was the untreated group (right). Each lane represents a sample from a single mouse. The hemoglobin pattern for the C57BL/6 and HW80 controls are shown on the right. (B) Two independent mixing experiments were performed, and the data for both of these are graphically shown. The y-axis represents the percentage of donor engraftment with MDR1-transduced cells, as indicated by hemoglobin electrophoresis. Each line represents an individual mouse analyzed serially over time.
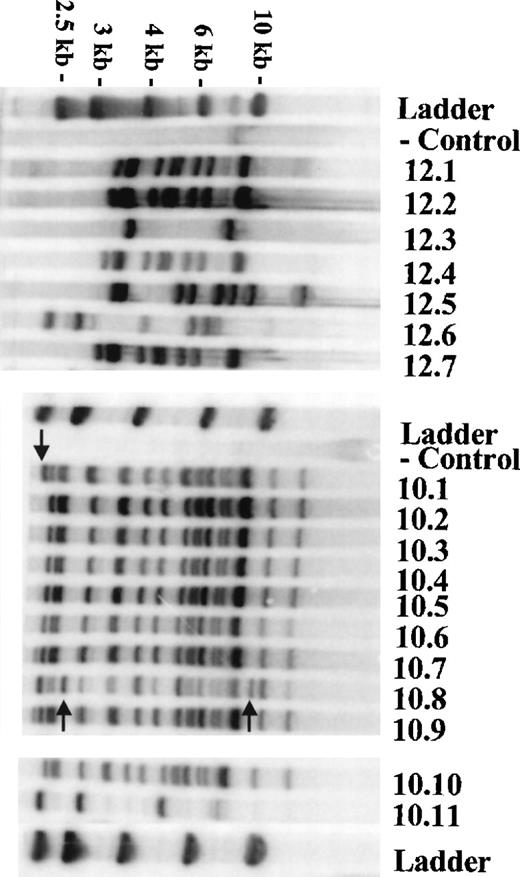
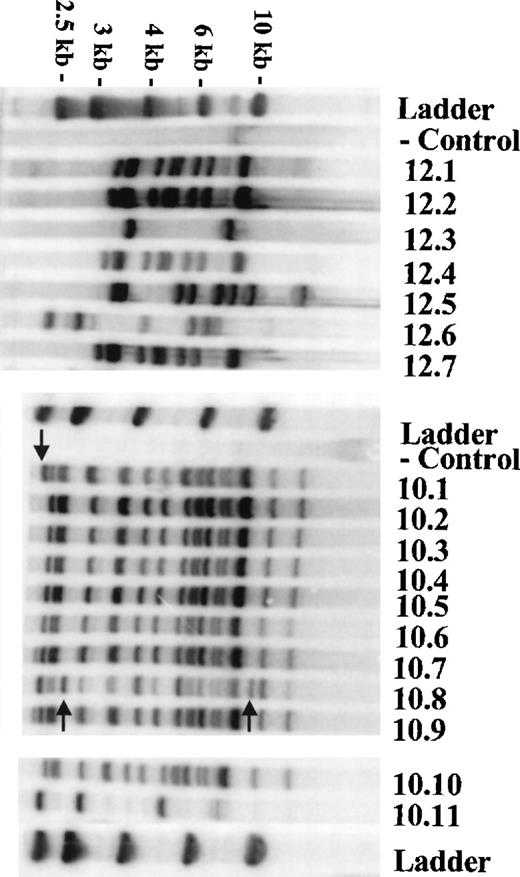
Clonality and copy number in transduced stem cell clones
We next determined whether the outgrowth of MDR1-transduced cells in vivo was caused by polyclonal stem cell expansion. Six of the primary transplant recipients from experiment 1 were killed 20 to 26 weeks after transplantation, and the BM cells were injected into irradiated secondary recipients. Day 12 CFU-S colonies were then isolated, and DNA was analyzed by Southern blotting for MDR1-vector integration sites. Figure 4 shows 2 representative Southern blots depicting the range of clonality observed in these mice. Mouse 12 showed 4 unique integration patterns within 7 individual CFU-S, indicating that hematopoiesis was polyclonal at a time when MDR1-transduced stem cells had expanded and out-competed the control graft. It was noted that there was an increased number of clones with relatively high vector copy numbers (12.1, 12.2, 12.4, 12.5, and 12.7) versus low copy numbers (12.3 and 12.6). Mouse 10 showed oligoclonal hematopoiesis, whereas all clones but 1 (10.11) showed a highly uniform banding pattern with very high copy number (18 integrants). Some stem cell clones in mouse 10 showed unique integrations (arrows) in addition to the common integration sites. This was probably caused by self-renewing stem cell divisions that occurred during the 48-hour transduction period. Of the 6 primary mice analyzed, 3 showed polyclonal stem cell patterns, 1 was oligoclonal, and 2 showed a monoclonal pattern (some data not shown). The increased proportion of clones with relatively high copy numbers may reflect a proliferative advantage for stem cell clones with relatively high levels of P-gp expression.
Clonality analysis of secondary CFU-S from mice transplanted with HaMDR1-transduced BM cells.
Two mice from mixing experiment 1 were killed 24 and 20 weeks after transplantation, and bone marrow-derived CFU-S colonies were harvested 12 days after injection into irradiated mice. DNA was prepared from each CFU-S colony and analyzed for vector integration sites by Southern blot analysis. Because the probe is upstream of the 5′EcoRI site in the vector, each band represents a unique integration site within a CFU-S clone. The left panel shows the analysis of 7 clones derived from mouse 12, and the right panel shows 11 clones from mouse 10. DNA from a normal spleen (control) shows a faint endogenous band hybridizing with the MDR1 probe fragment. The DNA ladder is shown on each gel, and the ladder marker sizes are indicated on the left. Small arrows in the right panel indicate unique retroviral integration sites in a parent stem cell clone.
Clonality analysis of secondary CFU-S from mice transplanted with HaMDR1-transduced BM cells.
Two mice from mixing experiment 1 were killed 24 and 20 weeks after transplantation, and bone marrow-derived CFU-S colonies were harvested 12 days after injection into irradiated mice. DNA was prepared from each CFU-S colony and analyzed for vector integration sites by Southern blot analysis. Because the probe is upstream of the 5′EcoRI site in the vector, each band represents a unique integration site within a CFU-S clone. The left panel shows the analysis of 7 clones derived from mouse 12, and the right panel shows 11 clones from mouse 10. DNA from a normal spleen (control) shows a faint endogenous band hybridizing with the MDR1 probe fragment. The DNA ladder is shown on each gel, and the ladder marker sizes are indicated on the left. Small arrows in the right panel indicate unique retroviral integration sites in a parent stem cell clone.
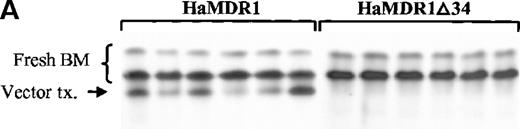
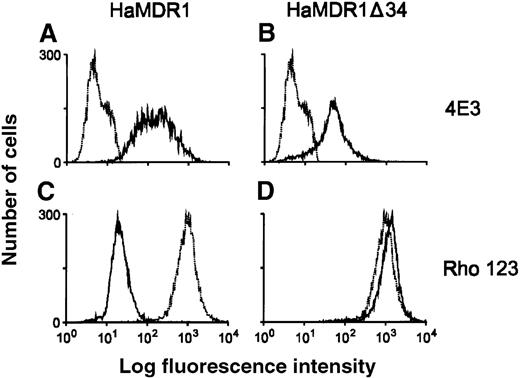
Development of a functionally inactivated MDR1 vector
We next tested whether the expansion of SP cells and repopulating cells required the efflux-pump function of P-gp. A vector was constructed (HaMDR1Δ34) that was otherwise identical to HaMDR1 except for a coding region deletion, resulting in the loss of 34 amino acids in the linker region between the 2 adenosine triphosphate hydrolysis sites. As originally described,28 this mutant MDR1 cDNA expresses P-gp on the cell surface at relatively normal levels, but the mutant protein cannot act as an efflux pump. As expected, producer cells expressing the HaMDR1Δ34 vector had relatively high levels of P-gp expressed on the cell surface, as detected by flow cytometry using the monoclonal antibody 4E3, but lacked the ability to efflux the P-gp substrate Rho 123 (Figure 5). The ability of the HaMDR1Δ34 vector to transduce early bone marrow cells was compared with the HaMDR1 vector by evaluating the transduction frequency of the 2 vectors in primary CFU-S. This analysis showed that the HaMDR1Δ34 vector was highly efficient at transducing CFU-S and had a titer at least equivalent to the wild-type HaMDR1 vector (Figure6).
P-gp expression and function in producer cells transduced with the HaMDR1▵34 vector.
Monoclonal antibody 4E3 was used to detect cell surface expression of P-gp in GP-E86 cells transduced with the HaMDR1 vector (A) or with the HaMDR1Δ34 vector (B). The heavy line represents results from the producer cell lines, whereas the lighter lines show negative controls using nontransduced GP-E86 cells. Molecular pump function was also assayed in these cells using a rhodamine exclusion assay (C-HaMDR1, D- HaMDR1Δ34). The presence of cells with low fluorescence indicates rhodamine efflux activity caused by P-gp expression. Again, the light lines are nontransduced negative controls.
P-gp expression and function in producer cells transduced with the HaMDR1▵34 vector.
Monoclonal antibody 4E3 was used to detect cell surface expression of P-gp in GP-E86 cells transduced with the HaMDR1 vector (A) or with the HaMDR1Δ34 vector (B). The heavy line represents results from the producer cell lines, whereas the lighter lines show negative controls using nontransduced GP-E86 cells. Molecular pump function was also assayed in these cells using a rhodamine exclusion assay (C-HaMDR1, D- HaMDR1Δ34). The presence of cells with low fluorescence indicates rhodamine efflux activity caused by P-gp expression. Again, the light lines are nontransduced negative controls.
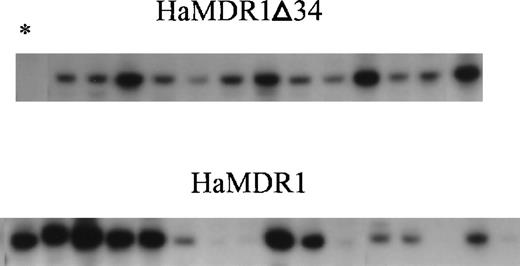
Transduction efficiency of vectors in primary CFU-S.
Whole bone marrow cells were transduced either with the HaMDR1Δ34 vector (top row), or the HaMDR1 vector (bottom row). The cells were then injected into irradiated recipients, and DNA was later prepared from day 14 CFU-S colonies. Southern blot analysis was performed to detect the proviral genome by digesting with EcoRI and probing with a full-length MDR1 cDNA. Each lane represents a sample from an individual colony. The lane marked by an asterisk is from an nontransduced CFU-S colony, which serves as a negative control.
Transduction efficiency of vectors in primary CFU-S.
Whole bone marrow cells were transduced either with the HaMDR1Δ34 vector (top row), or the HaMDR1 vector (bottom row). The cells were then injected into irradiated recipients, and DNA was later prepared from day 14 CFU-S colonies. Southern blot analysis was performed to detect the proviral genome by digesting with EcoRI and probing with a full-length MDR1 cDNA. Each lane represents a sample from an individual colony. The lane marked by an asterisk is from an nontransduced CFU-S colony, which serves as a negative control.
Requirement of P-gp pump function for SP cell expansion in vitro
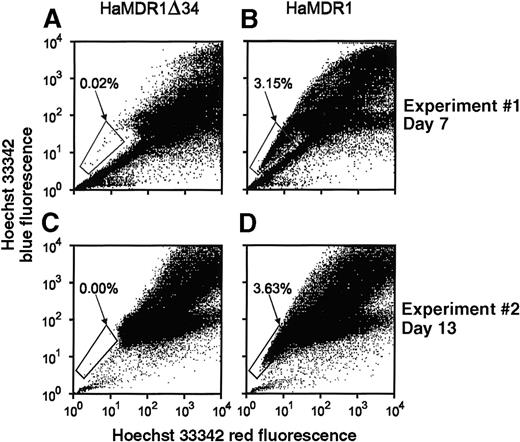
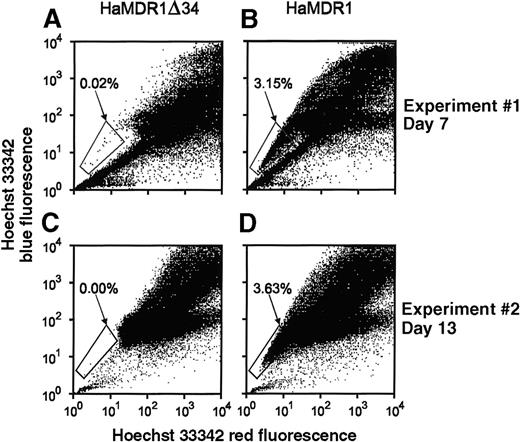
In 2 separate experiments, BM cells were transduced with the HaMDR1Δ34 vector, expanded in culture, and analyzed at various time points for changes in the number of SP cells. The first experiment was analyzed after 7 days of culture and showed no SP cell expansion in cultures transduced with the HaMDR1Δ34 vector, whereas there was a marked expansion of SP cells using the HaMDR1 vector (Figure7). A second experiment showed a complete lack of SP cells in cultures transduced with the HaMDR1Δ34 vector and expanded for 13 days (Figure 7). These experiments demonstrated that P-gp pump function was required for the expansion of SP cells in culture.
Quantitation of SP cell expansion in cultures of cells transduced with the HaMDR1▵34 vector.
BM cells were transduced with either the HaMDR1Δ34 (A, C) or the HaMDR1 vector (B, D) and then were expanded in suspension cultures for the indicated time periods. (A, B) SP cell analyses performed after 7 days of expansion. (C, D) A second independent experiment analyzed after 13 days of culture. The percentage of cells in the SP cell gate is indicated in each panel. In experiment 2, propidium iodide was added before flow cytometry analysis to exclude dead cells from the initial gated population.
Quantitation of SP cell expansion in cultures of cells transduced with the HaMDR1▵34 vector.
BM cells were transduced with either the HaMDR1Δ34 (A, C) or the HaMDR1 vector (B, D) and then were expanded in suspension cultures for the indicated time periods. (A, B) SP cell analyses performed after 7 days of expansion. (C, D) A second independent experiment analyzed after 13 days of culture. The percentage of cells in the SP cell gate is indicated in each panel. In experiment 2, propidium iodide was added before flow cytometry analysis to exclude dead cells from the initial gated population.
Requirement of pump function for the expansion of repopulating cells
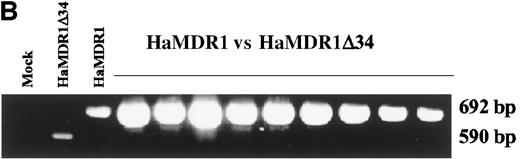
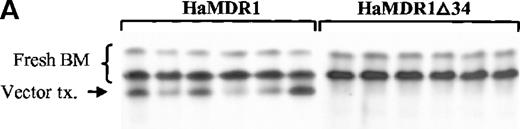
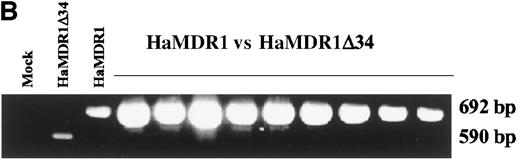
The HaMDR1Δ34 vector was next evaluated in competitive repopulation experiments to determine whether P-gp pump function was required for the expansion of repopulating cells. Bone marrow from C57BL/6 mice was transduced with either the HaMDR1Δ34 or the HaMDR1 vector, and then expanded in culture for 12 days. In one experiment, the expanded cells were competed against fresh BM cells from HW80 mice. The input ratio used was 0.02 femur volumes of transduced, expanded marrow to 0.25 femur volumes of fresh HW80 marrow. Sixteen weeks after transplantation, the recipient mice were analyzed by hemoglobin electrophoresis. All 6 mice transplanted with HaMDR1 transduced cells showed significant contributions from the transduced graft (Figure8A), despite the low input ratio of transduced cells. In contrast, there was no detectable donor contribution from the HaMDR1Δ34-transduced graft in any of the 6 mice that received HaMDR1Δ34-transduced and expanded cells along with fresh BM cells.
Competitive repopulation studies using cells transduced with the HaMDR1▵34 vector.
(A) Hemoglobin electrophoresis of 12-day expanded cells competed against fresh bone marrow cells. C57BL/6 cells were transduced with either the HaMDR1 vector (left lanes) or with the HaMDR1Δ34 vector (right lanes) and competed against fresh HW80 bone marrow cells at a femur volume ratio of 0.02 transduced to 0.25 fresh. Sixteen weeks after transplantation into irradiated recipient mice, hemoglobin electrophoresis was performed to monitor engraftment from the 2 donor sources. Each lane represents the results from an individual transplanted mouse. (B) PCR analysis of DNA from peripheral leukocytes of mice transplanted with equal volumes of HaMDR1 and HaMDR1Δ34-transduced marrow. The single primer set was used that flanked the Δ34 deletion and amplified a 692-bp and a 590-bp fragment from the HaMDR1 and the HaMDR1Δ34 proviral genomes, respectively. From the left, the first lane is from a mock-transduced mouse, the second lane from a mouse that received only HaMDR1Δ34-transduced cells, and the third lane from a mouse that received only HaMDR1-transduced cells. The remaining lanes are from 2 independent experiments in which mice were transplanted using 0.02 femur volumes from each expanded graft. The 3 mice in the first experiment were analyzed 11 weeks after transplantation, and the last 6 lanes are from mice from a second experiment analyzed 18 weeks after transplantation.
Competitive repopulation studies using cells transduced with the HaMDR1▵34 vector.
(A) Hemoglobin electrophoresis of 12-day expanded cells competed against fresh bone marrow cells. C57BL/6 cells were transduced with either the HaMDR1 vector (left lanes) or with the HaMDR1Δ34 vector (right lanes) and competed against fresh HW80 bone marrow cells at a femur volume ratio of 0.02 transduced to 0.25 fresh. Sixteen weeks after transplantation into irradiated recipient mice, hemoglobin electrophoresis was performed to monitor engraftment from the 2 donor sources. Each lane represents the results from an individual transplanted mouse. (B) PCR analysis of DNA from peripheral leukocytes of mice transplanted with equal volumes of HaMDR1 and HaMDR1Δ34-transduced marrow. The single primer set was used that flanked the Δ34 deletion and amplified a 692-bp and a 590-bp fragment from the HaMDR1 and the HaMDR1Δ34 proviral genomes, respectively. From the left, the first lane is from a mock-transduced mouse, the second lane from a mouse that received only HaMDR1Δ34-transduced cells, and the third lane from a mouse that received only HaMDR1-transduced cells. The remaining lanes are from 2 independent experiments in which mice were transplanted using 0.02 femur volumes from each expanded graft. The 3 mice in the first experiment were analyzed 11 weeks after transplantation, and the last 6 lanes are from mice from a second experiment analyzed 18 weeks after transplantation.
In addition, both transduced grafts were directly competed by transfusing equal volumes of each graft into irradiated recipients and then using PCR to evaluate the relative contributions to engraftment in peripheral blood leukocytes. PCR primers were developed that flanked the 34-amino acid deletion and, therefore, could co-amplify products of 2 different sizes from the HaMDR1 and HaMDR1Δ34 vectors (692 and 590 bp, respectively). In 9 mice from 2 independent experiments, there was no detectable contribution from the HaMDR1Δ34 vector, whereas HaMDR1-transduced cells were readily detected (Figure 8B). The presence of the HaMDR1Δ34-amplification product was easily detected in mice transplanted solely with unexpanded, transduced cells, ruling out a lack of stem cell transduction with HaMDR1Δ34 as the explanation for the competition result.
Myeloproliferative disorder in transplanted mice
We reported previously that recipients of ex vivo expanded HaMDR1-transduced BM cells developed myeloproliferative disease.22 In this study, we analyzed the peripheral white blood cell counts of transplanted mice at varying times after transplantation, looking for the characteristic leukocytosis associated with the myeloproliferative syndrome. In the 2 groups of mice transplanted with freshly transduced HaMDR1-transduced cells, 3 of 13 and 1 of 18 showed leukocyte counts greater than 20 000 cells/μL at 24 and 26 weeks after transplantation, respectively. In contrast, in our earlier experiments22 that used cells expanded for 12 days in vitro, we saw leukocytosis in 21 of 24 and 7 of 7 mice at 25 and 27 weeks, respectively. The 4 mice transplanted exclusively with HaMDR1Δ34-transduced bone marrow cells have been followed up for 15 weeks, and none have shown leukocytosis or any other abnormalities.
Discussion
Although it is well known that the MDR1 gene is expressed in primitive human hematopoietic cells,11 the functional importance, if any, of MDR1 gene expression has not been defined. There are several lines of evidence suggesting that expression of the MDR1 gene, or perhaps of other ABC transporters, has an important functional role in stem cells. Repopulating stem cells from a variety of species can be purified based on their ability to exclude fluorescent dyes, a property at least partially attributable to transporter expression. This conservation of transporter expression in stem cells is consistent with an important functional effect. A more direct line of evidence comes from our previous experiments showing that enforced expression of the MDR1 gene resulted in marked amplification of murine stem cells in a 12-day culture period.22 The data presented here confirm and extend our earlier observations and provide further support for the concept that MDR1 transporter function can influence the replicative behavior of stem cells. It is unknown whether these stem cell effects are limited to the setting of enforced overexpression or whether they reflect a critical stem cell function normally provided by endogenous transporter expression.
An intriguing link between MDR1 expression and normal stem cell function has been the identification of the SP stem cell phenotype. SP stem cells are found in the bone marrow of multiple mammalian species and express low to undetectable levels of the CD34 antigen,21 indicating that they may contain the primitive CD34− stem cells that have been recently described in xenograft transplantation experiments.31,32 Because the SP phenotype can be abrogated with verapamil, a known inhibitor of P-gp, it has been suggested that the SP phenotype may be caused by expression of the MDR1 gene or perhaps by another ABC transporter.20Our experiments demonstrated that enforced MDR1 expression resulted in a large amplification of SP stem cells in culture. These data strengthen the functional link between the SP stem cell phenotype and MDR1 gene expression. One possible mechanism for the MDR1-mediated expansion of stem cells is through a reduction of apoptosis in the cultures. CD34+ hematopoietic cells normally undergo apoptosis during ex vivo expansion cultures.33 It has recently been shown that P-gp can inhibit apoptosis in cultured hematopoietic cells8 and in other cell systems.9,34 35
In contrast, when DHFR-transduced control cells were cultured, SP stem cells were progressively lost over time. This loss of SP cells correlates with the known loss of repopulating stem cells with extended culture periods.36-38 Deleterious effects on SP stem cells were even noted in control cultures immediately after the 4-day transduction period. The relative loss of long-term repopulating stem cells during transduction with the DHFR control vector may, in part, explain the difficulty in obtaining durable gene marking in large animal models. Culture conditions have recently been identified that minimize the loss and differentiation of repopulating stem cells,36 39 and it may be that these methods result in relative preservation of SP stem cells.
To determine whether MDR1-mediated stem cell amplification was restricted to the setting of ex vivo expansion cultures, we examined whether freshly transduced cells would have a direct competitive advantage in vivo after transplantation. These experiments showed a large selective advantage for the HaMDR1-transduced cells that progressively emerged in transplanted mice during a 6-month time frame. Although it is theoretically possible that some of the observed stem cell expansion might have occurred during the 2-day transduction period, our previous results22 showed little amplification of repopulating cells at day 0. Furthermore, the slow emergence of the MDR1-transduced graft over 24 weeks is most consistent with a direct proliferative advantage in vivo. These data suggest that MDR1 expression may modulate an endogenous stem cell substrate in vivo rather than simply extrude some component within the ex vivo culture media. In the secondary CFU-S experiments, we noted that most stem cell clones had relatively high copy numbers of the MDR1 vector (8 to 18 copies). The degree of amplification seen in a given stem cell clone may be directly related to the level of expression of P-gp, consistent with the correlation between copy number and expansion. It is unlikely that these high copy numbers would be achieved in transplanted primate stem cells using current gene transfer methodologies, raising the question whether the observed stem cell effects would be expected in large animals or in clinical trials.
Before this study, one important mechanistic question was whether the pump function of P-gp was necessary for stem cell expansion. If the pump function were not required, it would suggest that amplification was caused by direct membrane effects from P-gp or some artifacts of the retroviral transduction system. Using a vector that expressed a functionally inactive P-gp, we were able to show that pump function was required for expansion of SP cells in vitro and for expansion of repopulating cells in vivo. These findings provide further support for the concept that the observed stem cell effects are caused by the redistribution of a critical substrate within stem cells.
Some mice transplanted with MDR1-transduced cells developed a myeloproliferative syndrome characterized by high white blood cell counts, immature myeloid cells in the peripheral circulation, and splenomegaly, resulting in a syndrome that phenotypically resembled chronic myelogenous leukemia. This syndrome occurred with a decreased incidence and a longer latency period than in historical controls22 transplanted with ex vivo-expanded, MDR1-transduced cells. This comparison suggested that the rate of syndrome development was related to the degree of stem cell expansion, perhaps because of increased probability of a second genetic event required for transformation. In prior studies of MDR1 transfer into murine stem cells,23,40,41 the development of a myeloproliferative syndrome was not reported. One possible explanation for this discrepancy has to do with the differences in the vectors used in these studies. The vector used in our stem cell expansion experiments was modified to reduce cryptic mRNA splicing within the MDR1 coding sequence12 24 and likely expressed greater amounts of P-gp than the vectors used in the previous studies.
The relation between MDR1 gene expression and the occurrence of a myeloproliferative disorder in our model system raises the possibility that dysregulated P-gp expression may contribute to the development of leukemia. Among patients with acute myelogenous leukemia, between 35% and 70% demonstrate P-gp expression in the pretreatment leukemic blasts. P-gp expression is a strongly negative prognostic factor.42 Increased P-gp expression in blast cells is caused by hypomethylation of sequences in the MDR1 promoter, at least in some patients.43 In chronic myelogenous leukemia, approximately 60% of patients show MDR1 expression in leukemic cells from the bone marrow.44 Although the occurrence of MDR1-negative cases seemingly argues against a necessary role for dysregulated transporter expression in leukemogenesis, it should be noted that high levels of expression of other transporter family members have been identified in a significant number of cases.42 45
Acknowledgments
We thank Dr Michael Gottesman for his generous gift of the Δ34 MDR1 cDNA plasmid. We also thank Richard Ashmun, Richard Cross, Jim Houston, and Sam Lucas for their invaluable assistance in performing the SP cell assays.
Supported by National Heart, Lung, and Blood Institute program project grant P01 HL 53749, James S. McDonnell Foundation grant 94-50, ASSISI Foundation of Memphis grant 94-00, Cancer Center support grant P30 CA 21765, and American Lebanese Syrian Associated Charities.
K.D.B. and S.Z. contributed equally to this work.
Reprints:Brian P. Sorrentino, Division of Experimental Hematology, St. Jude Children's Research Hospital, 332 N. Lauderdale, Memphis, TN 38105; e-mail: brian.sorrentino@stjude.org.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.