Abstract
Clinical data on 7840 HIV-positive patients, representing 43 745 patient-years of follow-up, has been collected. All patients with ARL since 1986 (n = 150) were assessed at presentation for prognostic factors and outcomes recorded. Comparisons are made between cases in the pre-HAART era (1988-1995), and the HAART era (1996-1999). Statistical models are used to calculate the incidence of ARL and factors predicting its development. The incidence of ARL has not changed over time (3 to 7 of 1000 patients per year,P = .933), but contributes to a greater percentage of first AIDS-defining illnesses (ADI) in the HAART era (P ≤ .0001). Older age, nadir CD4 count, and no prior HAART use, predict the development of ARL. There has been no change in stage at presentation, presence of B symptoms, performance status, or marrow involvement between the 2 time cohorts or between patients with or without prior HAART exposure. Similarly, there is no difference in survival duration between the pre-HAART and HAART era (log rankP = .15) or specifically in patients treated with HAART before ARL diagnosis (log rank P = .12). The use of HAART has not yet been shown to influence the incidence or survival of ARL. However, because nadir CD4 count and use of HAART are independent predictors of ARL development, this may translate into a future fall in new cases.
Introduction
High-grade B-cell non-Hodgkin lymphoma (NHL) has been classified as an AIDS-defining illness (ADI) since 1985, following the description of NHL in a group of 90 HIV-1 seropositive men.1 It has since been recognized to occur in AIDS patients at a frequency more than 100 times that of the general population.2 AIDS-related lymphoma (ARL) appears to be slightly more common in hemophiliacs and less common in intravenous drug users compared with other HIV transmission groups.3In the era before highly active antiretroviral therapy (pre-HAART) (before 1996), the incidence of AIDS-related lymphoma remained fairly constant at around 6 to 7 cases per 1000 person-years.4The annual occurrence of NHL as a percentage of all ADIs in 1994 was estimated at 3.0% in the United States2 and 3.6% in Europe.5 As a first ADI, NHL occurred in only 1.5% of cases. Because the development of ARL is associated with a relative risk of death of 20.56,6 HIV-associated NHL consequently accounted for up to 16% of all deaths attributable to AIDS.
The widespread introduction of HAART since 1996 has led to dramatic reductions in AIDS-related morbidity and mortality throughout the developed world.7,8 This is largely due to a marked fall in the incidence of the major opportunistic infections such asPneumocystis carinii pneumonia (PCP), cytomegalovirus (CMV), and Mycobacterium avium complex (MAC). Although this trend has also been observed for Kaposi sarcoma, the effect on NHL has not been so clear. Ledergerber et al9 have recently reported from the Swiss HIV Cohort Study. A substantial relative risk reduction from 1992-1994 to 1997-1998 was seen for the development of Kaposi sarcoma as well as for other AIDS-defining conditions. No significant trend was seen for NHL, implying an ongoing risk for patients, despite the use of potent antiretroviral therapies. Other groups from the United States confirm this finding. The US AIDS Clinical Trial Group (ACTG) found the incidence rates for both Kaposi sarcoma and NHL to be decreasing, but the former far more profoundly and consistently.10 In contrast, a group from the San Francisco City Clinic found the incidence of lymphoma between 1993 and 1996 to be unchanged at 1.4 to 1.8 per 100 person-years,11whereas the Multicenter AIDS Cohort Study (MACS) actually found an increase in the incidence of NHL at a rate of 21% per year.12 During the same period, the incidence of Kaposi sarcoma fell by 66%.
As a percentage of first ADIs, NHL has increased. In western Europe, it rose from 3.6% in 1994 to 4.9% in 1997.5 This is likely to reflect the reduction in other causes of AIDS rather than a true rise in NHL incidence. It may be that with increasing use and duration of HAART, both the incidence and characteristics of AIDS-related lymphoma will change. Most published studies have only reported follow-up to 1997. We reviewed the incidence, presentation, and survival of all patients with lymphoma treated in our clinic from 1986 to October 1999.
Patients and methods
Clinical data on all individual HIV-1 seropositive patients attending the Chelsea and Westminster Hospital (CWH) have been prospectively collected since 1981, and these patients comprise the total population at risk of developing lymphoma in our study. This database contains information on 7840 patients and represents 43 745 patient-years of follow-up. The incidence of NHL has been calculated using the total numbers of HIV- seropositive patients attending the CWH each year as the denominator. Information on patient demographics including age, sex, ethnicity, and mode of HIV transmission are recorded. Other information extracted from the database includes AIDS diagnoses, CD4 cell counts, and history of antiretroviral therapy. As HIV viral load data have been available only since 1996, we did not include this in the analysis presented.
For the purposes of this study, only patients with systemic NHL were included as cases (excluding cases of Hodgkin disease and primary central nervous system lymphoma). All cases were confirmed by diagnostic histology. The characteristics of the patients with systemic NHL were compared with those of the general HIV clinic population to identify significant predictors of lymphoma development. Lymphoma cases were also divided on the basis of their date of NHL diagnosis into the pre-HAART era (defined as before 1996) and the HAART era (defined as 1996-1999), and more specifically, into patients who had treatment with HAART before NHL diagnosis and those who had not. Comparisons of the incidence, clinical details, and survival of patients who developed NHL during the 2 periods are described.
Statistical methods
All data presented as qualitative categories have been grouped into quartiles. Where variables were found to have missing data, a separate category was identified and estimates are presented separately for this.
A log-linear regression analysis was used to determine the incidence of NHL. A log transformed person time at risk was used as a rate multiplier in the log-linear model. A person time at risk was defined as entry into the study as an HIV positive case until either development of NHL, or if not an NHL case, then either the date of death or the most recent follow-up. Therefore, a person who has NHL would no longer contribute to patient time of follow-up since having NHL and any further clinical observation on that patient would be excluded from the analysis.
All P values are 2-sided. Log-linear regression models were used to derive incidence rates per patient year and the corresponding rate ratios. These were derived using the GENMOD procedure in SAS (Cary, NC) with the assumption that NHL events occurred randomly and followed a Poisson distribution.
Results
Incidence of non-Hodgkin lymphoma
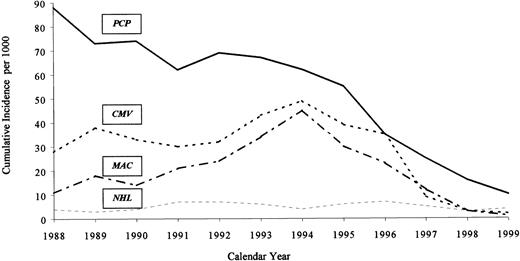
A total of 150 patients have been diagnosed with systemic NHL during 1986-1999. An additional 47 patients were diagnosed with primary central nervous system lymphoma, but these are not included in the following analysis and are described elsewhere.13 The number of cases diagnosed per year has fluctuated from 5 to 19 (Table1). The cumulative incidence of NHL ranges from 3 of 1000 patients per year to 7 of 1000 patients per year, and there has been no significant trend in this incidence over time (P = .933) (Figure 1). This is in contrast to the incidence of PCP, MAC, and CMV within the clinic, all of which have fallen dramatically since 1995 (Figure 1). In particular, if the pre-HAART and HAART eras are directly compared, the incidence of NHL remains unchanged (0.53% vs 0.47%,P = .73) (Table 2). The percentage of NHL accounting for a first ADI, however, has changed, rising from 1.3% pre-HAART to 5.6% post-HAART (P ≤ .0001). This reflects the significant reduction in the number of new AIDS cases (17.7% vs 5.8%) because of other opportunistic infections between the 2 periods.
Cumulative incidence per 1000 population of major opportunistic infections and non-Hodgkin lymphoma from 1988-1999.
Cumulative incidence per 1000 population of major opportunistic infections and non-Hodgkin lymphoma from 1988-1999.
Factors involved in the development of non-Hodgkin lymphoma
The univariate log-linear model showed a significant association between age at entry to the study and incidence of NHL, whether age was assessed as a continuous variable or grouped by quartiles (Table3). The incidence of lymphoma in a patient presenting over the age of 37 years was shown to be over 3 times that of patients who were under 26 years old (P ≤ .001). There were no significant differences in the incidence of NHL by gender (P = .14), ethnicity (P = .37), intravenous drug use (P = .27), or year of entry to the study (P = .88).
First recorded and nadir CD4 cell count are presented in the univariate model. Five NHL patients had neither count available; these patients had been found to be HIV positive at the time of NHL diagnosis and died very shortly afterward.
The CD4 count nadir, and first recorded CD4 count, were both strongly associated with the development of lymphoma. As the CD4 count fell, the development of lymphoma became more likely. Of note, in this analysis, CD4 counts are analyzed and presented in statistical quartiles. The incidence of NHL was twice that in patients whose first-ever CD4 count was below 305 cells/μL compared with those whose first-ever CD4 was above 305 cells/μL. A similar trend was seen in patients whose nadir CD4 count fell below 114 cells/μL, compared with those whose nadir CD4 remained above 114 cells/μL. If a specific nadir CD4 count of 350 cells/μL is taken (the level at which initiation of treatment is advocated in the UK), a steep rise in incidence below this level is seen. Above 350 cells/μL, the incidence of NHL is 0.7 cases per 10 000 patient-years, whereas below this level, it rises to 10 cases per 10 000 patient-years (P < .001). Indeed, only 2 of the 150 patients had a nadir CD4 count of more than 350 cells/μL.
The only other variable shown to be protective against the development of NHL was the use of HAART (defined as an antiretroviral regimen containing at least one protease inhibitor or non-nucleoside reverse transcriptase inhibitor). Seventeen NHL patients had experienced a HAART-containing regime before the diagnosis of NHL, as opposed to 133 either naı̈ve to therapy or treated with nucleosides alone. The incidence of NHL was significantly lower in patients who had been treated with HAART (P < .001)
A multivariate log-linear model was used to determine independent predictors of NHL. Those variables found to be significant in the univariate log-linear model were entered into the multivariate model. A conservative P value selection criteria (P < .1) was used to enter variables into the multivariate model. As nadir CD4 counts and first recorded CD4 counts are correlated with each other, only nadir CD4 count was selected for entry. Older age at entry and nadir CD4 count were found to be independent significant predictors of NHL incidence, as was the use of HAART (P < .001) (Table4). The incidence estimates presented in Table 4 are adjusted for gender, ethnicity, intravenous drug use, and year of entry to the study.
Clinical features of systemic non-Hodgkin lymphoma
The patients with systemic NHL have been divided into 2 cohorts that correspond to the introduction of HAART (Table5). The cohorts were analyzed for established prognostic factors at NHL presentation. There has been no significant change in the stage of NHL at presentation, presence of B symptoms, ECOG (Eastern Cooperative Oncology Group) performance status, or bone marrow involvement between the 2 cohorts. However, in the recent cohort, fewer patients had a prior AIDS-defining illness, CD4 cell counts were higher, and patients were older. Those patients diagnosed with NHL within the HAART era were then further subdivided into 2 groups on the basis of whether they had actually received HAART before NHL diagnosis (Table 6). Those patients who had received prior HAART (n = 17) had higher CD4 counts but otherwise presented with similar clinical features to the group with no prior HAART exposure (n = 34).
Survival of systemic non-Hodgkin lymphoma
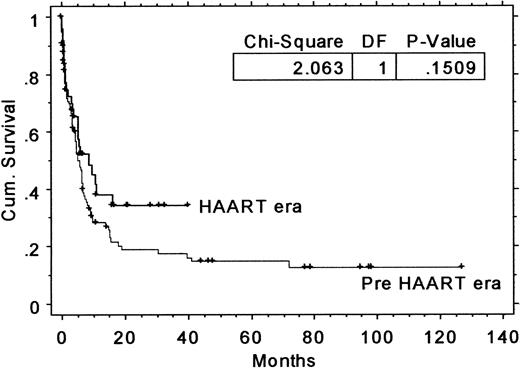
The overall survival of the pre- and post-HAART era cohorts are not significantly different (Mantel Cox log rank P = .15) with 2-year overall survivals of 29.0% (95% CI: 19.6%-38.4%) for the pre-HAART cohort, and 41.2% (95%CI: 26.2%-56.2%) for the more recent cohort (Figure 2). There is also no survival difference seen between those patients in the 1996-1999 era with HAART exposure before NHL diagnosis and those with no prior HAART exposure (log-rank P = .12, data not shown). This lack of significant improvement in overall survival may simply reflect insufficient sample size and follow-up, but is of concern, given that some prognostic factors such as prior AIDS diagnosis and median CD4 count are more favorable in the recent cohort.
Kaplan-Meier overall survival duration curves for AIDS-related systemic non-Hodgkin lymphoma comparing pre-HAART era (1988-1995) and HAART era (1996-1999).
Kaplan-Meier overall survival duration curves for AIDS-related systemic non-Hodgkin lymphoma comparing pre-HAART era (1988-1995) and HAART era (1996-1999).
Discussion
The development of non-Hodgkin lymphoma in association with HIV-1 infection is not only more common than in the general population, but is also associated with a less favorable outcome. This study describes our experience with lymphoma in this setting over the past 11 years. During this time, potent therapies for the treatment of HIV infection have become available, and morbidity and mortality have plummeted. Despite this, the incidence of NHL remains largely unchanged—a finding confirmed by other studies.9-11 As the incidence of other AIDS-defining illnesses drop, NHL becomes increasingly common as a first ADI and is likely to form a larger part of inpatient HIV care.
We have shown that older age, nadir CD4 count, and nonuse of HAART are all independently associated with the development of NHL. Increasing age is well recognized as a risk factor for the development of lymphoma in all patient groups, and the extended life span of HIV patients after the introduction of HAART may ultimately contribute to a larger “at-risk” population.
Unlike opportunistic infections, the development of NHL is unlikely to be the result of exposure to one single pathogen, but rather a consequence of several different events. It is, nevertheless, clearly linked to all forms of cellular immunosuppression, and both the absolute nadir CD4 count and the duration of nadir are likely to be important. The relationship to CD4 count is confirmed in our model showing that both first recorded and nadir CD4 counts are important predictors of NHL development. Because, in our study, the use of HAART has a significant protective effect on the development of NHL, it is hoped that the widespread use of these therapies, started before the nadir CD4 count drops below a critical level, may eventually help reduce the number of new cases of NHL. Recent data from the EuroSIDA study confirm that the nadir CD4 count has an important effect on HIV-1 disease progression, even if HAART is later able to induce a subsequent good CD4 rise.14 What constitutes a “safe” nadir CD4 count is more difficult to predict, although our study shows the incidence of NHL above a nadir CD4 of 350 cells/μL to be low (0.7 cases per 10 000 patient-years).
Early series reported the most influential prognostic variables for survival to be related to the severity of immunosuppression rather than lymphoma-related factors. Multivariate analysis of 2 series revealed that the CD4 count at diagnosis, a history of a prior AIDS-defining diagnosis, a poor performance status, and bone marrow involvement, were independent adverse prognostic factors.15,16 An International Prognostic Index for lymphoma has since been introduced for aggressive lymphomas in the non–HIV-infected population.17 Recent prospective data from an AIDS Clinical Trials Group (ACTG) study have suggested that the prognostic variables in ARL closely resemble those in the International Prognostic Index for non–HIV-associated NHL.18 In our cohort, those patients with NHL presenting since 1996 show no significant change in prognostic factors relating to the tumor itself (B symptoms, stage of disease, ECOG performance status) whether treated with HAART before their lymphoma diagnosis or not. Those patients on HAART had significantly higher CD4 counts at NHL diagnosis but there are no differences in other prognostic variables or overall survival. This study suggests that HAART may reduce the likelihood of developing systemic lymphoma but does not alter the natural history of NHL in people with HIV-1 infection.
In conclusion, it remains to be seen whether the incidence of NHL will eventually fall, similar to that of other opportunistic infections and Kaposi sarcoma. A significant number of patients (19% in our study) may always present with NHL unaware of their HIV diagnosis. For known HIV-positive patients however, our data suggest that better preservation of long-term immunologic function with HAART may translate into a future fall in the number of new cases of NHL.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Mark Bower, Department of Oncology, Chelsea and Westminster Hospital, 369 Fulham Rd, London SW10 9NH, UK.