Abstract
Genetic modification of hematopoietic stem cells often results in the expression of foreign proteins in pluripotent progenitor cells and their progeny. However, the potential for products of foreign genes introduced into hematopoietic stem cells to induce host immune responses is not well understood. Gene marking and induction of immune responses to enhanced green fluorescent protein (eGFP) were examined in rhesus macaques that underwent nonmyeloablative irradiation followed by infusions of CD34+ bone marrow cells transduced with a retroviral vector expressing eGFP. CD34+ cells were obtained from untreated animals or from animals treated with recombinant human granulocyte colony-stimulating factor (G-CSF) alone or G-CSF and recombinant human stem cell factor. Levels of eGFP-expressing cells detected by flow cytometry peaked at 0.1% to 0.5% of all leukocytes 1 to 4 weeks after transplantation. Proviral DNA was detected in 0% to 17% of bone marrow–derived colony-forming units at periods of 5 to 18 weeks after transplantation. However, 5 of 6 animals studied demonstrated a vigorous eGFP-specific cytotoxic T lymphocyte (CTL) response that was associated with a loss of genetically modified cells in peripheral blood, as demonstrated by both flow cytometry and polymerase chain reaction. The eGFP-specific CTL responses were MHC-restricted, mediated by CD8+lymphocytes, and directed against multiple epitopes. eGFP-specific CTLs were able to efficiently lyse autologous CD34+ cells expressing eGFP. Antibody responses to eGFP were detected in 3 of 6 animals. These data document the potential for foreign proteins expressed in CD34+ hematopoietic cells and their progeny to induce antibody and CTL responses in the setting of a clinically applicable transplantation protocol.
Introduction
Genetic modification of hematopoietic stem cells has the potential to treat a wide variety of disorders, including inherited metabolic abnormalities, malignancy, and human immunodeficiency virus infection.1,2 Although levels of gene marking in initial nonhuman primate and human clinical trials generally have been disappointingly low,3,4 advances involving the optimization of transduction of primitive hematopoietic cells and the administration of recombinant growth factors have recently resulted in significant increases in the levels of gene marking obtained in vivo.5-8 These advances now make possible the application of hematopoietic stem cell gene therapy for multiple diseases. In many instances, genetic modification of cells may result in the expression of potentially immunogenic proteins in hematopoietic stem cells. Examples of potential immunogens that might be introduced into hematopoietic stem cells include selectable markers such as neomycin phosphotransferase (neo),9foreign proteins such as transdominant viral proteins,10normal host proteins in subjects with congenital disorders that abrogate or alter expression of a specific gene product,11or cryptic open readings frames contained in vector sequences.12
In several gene-therapy applications not involving hematopoietic stem cells, induction of immune responses against transgenes has resulted in the elimination of genetically modified cells. Cytotoxic T lymphocyte (CTL) responses against a hygromycin/thymidine kinase gene have resulted in elimination of autologous T lymphocytes transduced with a retroviral vector expressing the hybrid selectable marker.13 Similarly, immune responses against recombinant adenoviral vectors and their transgenes have resulted in elimination of transduced cells following intramuscular injection of adenovirus vectors.14 However, induction of immune responses to the products of genes introduced into hematopoietic stem cells has been relatively uncommon. For instance, multiple studies in nonhuman primates have documented sustained expression of reporter genes such as enhanced green fluorescent protein (eGFP) or murine CD24 in macaques following autologous transportation of CD34+ cells transduced with murine leukemia virus (MLV) or lentivirus vectors.6,8,15 Long-term persistence of genetically modified cells has been observed after both myeloablative6,15 and nonmyeloablative8irradiation. In contrast, antibody responses and T-lymphocyte proliferative responses to α-L-iduronidase have been reported in dogs deficient in this enzyme that underwent autologous bone marrow transplantation with transduced cells without irradiation.11 Several mechanisms are likely to be involved in achieving long-term engraftment of genetically modified cells expressing potential immunogens, including immunosuppressive effects of irradiation regimens used for conditioning and the ability of neoantigens expressed in bone marrow cells to induce tolerance.9,16 17 At present, our understanding of the conditions that lead to induction of immune responses following autologous transplantation with genetically modified stem cells is still incomplete, and little information is available on the generation of CTL responses to transgenes expressed in hematopoietic stem cells in large animal models.
To evaluate the efficiency of different cytokine priming regimens on the levels of gene marking in vivo, we initiated a study using transduction of rhesus macaque CD34+ hematopoietic cells with an MLV/eGFP vector followed by reinfusion of transduced cells after nonmyeloablative irradiation. In these animals, we observed induction of relatively strong CTL and antibody responses against eGFP that were associated with the disappearance of eGFP-expressing cells in vivo.
Materials and methods
Retroviral vector production
The LZRS/eGFP vector was prepared by excising lacZfrom the MLV vector LZRS pBMN-Z18 byBamHI-NotI digestion and inserting aBamHI-NotI fragment containing eGFP (Clontech Laboratories, Palo Alto, CA) in its place. The resulting retroviral vector, LZRS/eGFP, does not express any proteins other than eGFP. A stable retroviral producer cell line was generated by calcium phosphate transfection of the human 293T cell–based MLV retroviral producer cell line Phoenix, which expresses the MLV amphotropic envelope,18 followed by selection of transfected cells using puromycin (2 μg/mL; Sigma Biochemicals, St Louis, MO) and then fluorescence-activated cell sorting using a Becton Dickinson FACS Vantage (Mountain View, CA) to select producer cells expressing the 10% highest eGFP fluorescence. For production of retroviral vector, producer cells were cultured in Stem Span SFEM (Stem Cell Technologies, Vancouver, BC, Canada). End-point dilution titers of retroviral supernatants were typically 1 × 105infectious units per milliliter, as determined by titration on 3T3 cells before concentration. All supernatants were concentrated 5-fold using Centriprep 30 concentrators (Amicon; Millipore, Beverly, MA) before use.
Animals
Rhesus monkeys, Macaca mulatta, with a mean weight of 2.8 ± 0.3 kg, were serologically negative for simian T-cell lymphotropic virus, simian type D virus, simian immunodeficiency virus, and herpes B virus. Research was conducted according to the principles enunciated in the Guide for the Care and Use of Laboratory Animals prepared by the Institute of Laboratory Animal Resources, National Research Council,19 and was approved by the Harvard Medical School Animal Care and Use Committee.
Cytokine mobilization and bone marrow harvesting
When indicated, macaques were treated with either granulocyte colony-stimulating factor (G-CSF) alone (10 μg/kg subcutaneous injections once a day for 5 days; Amgen, Thousand Oaks, CA), with marrow harvested on day 6, or G-CSF (10 μg/kg subcutaneous injections once a day for 5 days) and stem cell factor (SCF; 20 μg/kg subcutaneous injections once a day for 5 days) (a generous gift from Amgen), with marrow harvested on day 15 concurrent with reinfusion of 40 mL of autologous whole blood. Mononuclear cells from iliac crest bone marrow aspirates were isolated with sodium diatrizoate (Histopaque-1077; Sigma, St Louis, MO) followed by treatment with 0.45% ammonium chloride. Cells were resuspended in RPMI 1640 medium (Sigma) supplemented with 10% fetal calf serum (FCS), 10 mM HEPES, 2 mM L-glutamine, 50 IU/mL penicillin, and 50 μg/mL streptomycin (R10), and cultured on polystyrene at 37°C overnight. CD34+cells were then isolated from nonadherent cells by positive selection with immunomagnetic beads (Dynal, Lake Success, NY), as described previously.20 Cells purified in this manner were more than 90% CD34+ as assessed by flow cytometry.
Transduction and reinfusion of CD34+ cells
CD34+ cells were cultured in 24-well plates (non-tissue culture–treated; Falcon/Becton Dickinson Labware, Franklin Lakes, NJ) coated with 25 μg/well recombinant human fibronectin fragment CH-296 (Retronectin; Biowhittaker, Walkersville, MD) at a concentration of 1.5 to 2.5 × 105 cells per well (total volume 1.5 mL). Before transduction with retroviral vector, CD34+ cells were prestimulated for 24 hours with SCF (50 ng/mL), flt-3 ligand (50 ng/mL), and interleukin (IL)-3 (10 ng/mL) (all from Stem Cell Technologies) in Stem Span SFEM. After prestimulation, the cells were transduced once daily for 4 days. Each day, 1 mL of vector supernatant was removed from each well and replaced with 1 mL of viral supernatant supplemented with SCF, flt-3, and IL-3. Transduced CD34+ cells were then reinfused after whole-body irradiation with 240 cGy from a 60Co source.
Polymerase chain reaction (PCR) assays
PCR analysis of the MLV packaging sequence in samples of peripheral blood mononuclear cells (PBMCs) and colony-forming units (CFUs) was performed by quantitative real-time PCR with the fluorogenic 5′ nuclease assay (Taq Man) analyzed on an ABI PRISM 7700 Sequence Detection System (PE Applied Biosystems, Foster City, CA). Primers and probes were as follows: 5′ primer, CGC AAC CCT GGG AGA CGT CC; 3′ primer, CGT CTC CTA CCA GAA CCA CAT ATC C; and fluorescent probe, 6-FAM-CCG TTT TTG TGG CCC GAC CTG AG-TAMRA; as modified from previously published sequences.21 Amplification was performed in a final volume of 50 μL with 500 nM each primer, 200 nM probe, 3.5 mM MgCl2, 200 μM dNTPs (except for 400 μM dUTP in place of dTTP), 1.25 Ampli Taq Gold, and 0.5 U uracil-N-glycosylase (AmpErase; all reagents from PE Applied Biosystems). Amplification was carried out with 200 ng of template DNA for 45 to 50 cycles using 2-step PCR with an annealing temperature of 64°C and a melting temperature of 95°C. DNA was extracted from all cells with the use of the QIAamp DNA Blood Minikit (Qiagen, Valencia, CA). Standard curves for the MLV packaging sequence were generated by serial 10-fold dilutions of duplicate samples of the HEL-eGFP cell line (kindly provided by Karen Pollak, Indianapolis University School of Medicine) in DNA from untransduced CEMx174 cells. Samples from animals were run in quadruplicate, and reported values represent the means of replicate wells. This assay has a lower limit of detection of 0.01% transduced cells. Comparison of levels of transduction determined by flow cytometry and PCR revealed concordance within a 3-fold range for levels of transduced cells between 0.1% and 10%, consistent with the level of variation reported by others using this approach.22
PCR detection of replication-competent retrovirus was performed using primers specific for the MLV amphotropic envelope. Primers used were: 5′ primer, GAA CCA TCA AGG AGA CTT TAA CTA AAT TAA; and 3′ primer, AAG GCA TCT TGT ACA GTT CCC AGG AGG GAG.23 Amplification was carried out using “touchdown” PCR with an initial annealing temperature of 55°C, decreasing by 1°C per cycle for the first 10 cycles, followed by 30 cycles with an annealing temperature of 55°C. Reactions were performed with 200 ng template DNA, 0.2 mM of each oligonucleotide primer, 0.8 mM dNTPs, 3.5 mM MgCl2, and 1 U polymerase (Gibco BRL, Grand Island, NY). PCR products were separated on 1% agarose gels, stained with ethidium bromide, and visualized under UV light.
Flow cytometric analysis
Antibodies used for immunophenotyping included anti-CD4, anti-CD8, anti-CD20, anti-CD34 (Qbend-10; Coulter-Immunotech, Hialeah, FL), and anti-macaque CD3 (6G12), kindly provided by J. Wong, Massachusetts General Hospital.24 Cells were stained according to the manufacturer's instructions for staining and whole-blood lysis (Becton Dickinson). Flow cytometric analysis of the cells was performed using a FACS Calibur (Becton Dickinson), and eGFP emission was detected in the fluorescein isothiocyanate (FITC) channel. Negative controls from normal macaques were run with every experimental sample and were used to establish gates for eGFP expression, such that the level of background staining was always less than 0.1%, and generally less than 0.05%.
Colony assays
Purified populations of hematopoietic progenitor cells were resuspended in Dulbecco's Modified Eagle's Medium (Gibco BRL) with 2% FCS, 10 IU/mL penicillin, and 10 μg/mL streptomycin, and then added to complete methylcellulose medium with cytokines (IL-3, granulocyte–macrophage colony-stimulating factor, erythropoietin, and SCF) (Stem Cell Technologies) supplemented with an additional 20 ng/mL IL-3 (Stem Cell Technologies).3,25After 7 to 15 days at 37°C with 5% CO2, the total number of colonies was determined in duplicate using standard morphologic criteria.26 Colonies positive for eGFP were assessed using an inverted fluorescent microscope with a mercury light source (Olympus, Mellville, NY). Colonies processed for PCR analysis were placed in microcentrifuge tubes; lysed in 20 mM Tris-HCL (pH 8.4), 50 mM KCl, and 50 μg/mL Proteinase K (Sigma) at 56°C for 1 hour; and subjected to heat inactivation at 95°C for 15 minutes. Lysates were then analyzed for the vector DNA sequences with real-time PCR.
CTL assays
PBMCs obtained by sodium diatrizoate centrifugation were resuspended in R10 medium and then cultured with autologousherpes papio–transformed B-lymphoblastoid cell lines (B-LCLs) expressing eGFP antigens (gamma irradiated, 10 000 rad) at a responder to stimulator ratio of 10:1. Stimulator cells consisted of either transduced autologous B-LCLs expressing eGFP or autologous B-LCLs sensitized with eGFP peptides. B-LCLs were transduced with the LZRS/eGFP retrovirus vector and sorted using a FACS Vantage to obtain high-expressing cell lines (more than 90% eGFP+). eGFP peptides corresponding to the entire eGFP sequence were synthesized as 20–amino acid peptides, as described previously,27 with each peptide overlapping the previous peptide by 10 amino acids. Peptide-sensitized B-LCL lines were prepared by incubation of PBMCs with pools of up to 5 peptides, each at a final concentration of 20 μg/mL, for 60 minutes at 37°C, followed by 2 washes with R10 medium. Recombinant IL-2 (donated by M. Gately, Hoffman LaRoche, Nutley, NJ) was added to a final concentration of 20 U/mL on day 4 of culture. CTL clones were isolated by limiting-dilution cloning of stimulated PBMCs followed by restimulation every 10 to 14 days with concanavalin A (5 μg/mL; Sigma) and irradiated human PBMCs in the presence of IL-2 (50-100 U/mL), as described previously.28CTL assays were performed 10 to 14 days after stimulation. Where indicated, effector cells were fractionated into CD4+ and CD8+ populations with the use of immunomagnetic particles (Dynal), as described previously.29
Target cells consisted of autologous or allogeneic B-LCLs stably expressing eGFP or B-LCLs sensitized with peptide pools, as described above. Nontransduced B-LCLs were used as negative controls. For assays using CD34+ cells as target cells, autologous CD34+ cells were transduced as described above and used as target cells 48 hours after the last transduction cycle. Levels of eGFP expression in CD34+ cells were assessed by flow cytometric analysis of CD34+ cells 48 hours after transduction. On the day of assay, target cells were labeled with 51Cr (DuPont-NEN, Wilmington, DE), 50 μCi per 106 cells. Target cells (104 cells/well) were dispensed in duplicate for each effector-to-target ratio into 96-well U-bottom plates (CoStar, Cambridge, MA). Cold targets consisting of unlabeled, nontransduced autologous B-LCLs at a cold-to-hot target ratio of 15:1 were used to decrease background lysis. Chromium release was assayed after a 5-hour incubation at 37°C, as described in detail previously.29Spontaneous release of target cells was less than 35% in all assays. On the basis of assays from 6 control animals not exposed to eGFP, specific lysis of more than 10% seen at more than one effector-to-target ratio as compared with control B-LCLs was interpreted as significant.
Anti-GFP enzyme-linked immunosorbent assay (ELISA)
Individual wells of 96-well plates (Nunc Immunoplates, Naperville, IL) were coated with 0.3 μg per well of recombinant eGFP (Clontech) in pH 9.0 carbonate buffer at room temperature overnight. After washing, the plates were blocked by 0.3% bovine serum albumin. Serial 2-fold dilutions of serum were prepared in phosphate-buffered saline (PBS) with 0.05% Tween, 5% FCS, and 5% heat-inactivated goat serum and incubated at room temperature for 1 hour. Plates were then washed 4 times with PBS/0.05% Tween and then incubated with 100 μL of a 1:200 dilution of anti-monkey IgG–alkaline phosphatase (Kirkegaard and Perry Labs, Gaithersburg, MD) at room temperature for 1 hour. After 4 washes, 150 μL of substrate solution (p-nitrophenylphosphate at 1 mg/mL in diethanolamine buffer; Kirkegaard and Perry Labs) was added, and the reaction was stopped after 30 minutes by the addition of 150 μL of 5% EDTA. Absorbance was read at 410 nm. End-point dilution titers were calculated based on the last dilution at which the OD was 0.100 greater than that of the pretransplant control serum tested at the identical dilution or an OD of 0.100, whichever was greater.
Results
Yield and transduction efficiency of CD34+ cells obtained with or without cytokine treatment
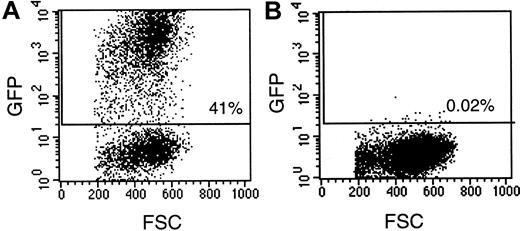
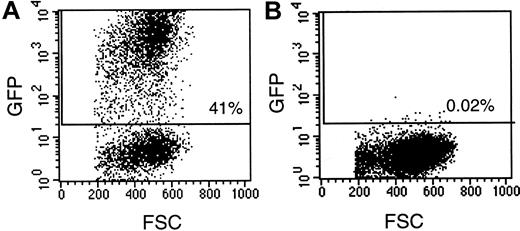
Several studies have shown that treatment with hematopoietic growth factors can enhance levels of gene marking of hematopoietic stem cells in nonhuman primates.7,8,30 The original goal of this study was to directly compare the effects of different cytokine priming regimens on the level of gene marking using an MLV vector expressing eGFP to facilitate rapid quantitation of transduced cells. Treatment with either G-CSF alone or G-CSF and SCF was well tolerated and resulted in increases in peripheral white blood cell counts to levels of 27 000 and 32 600 cells/μL 3 to 5 days after treatment (data not shown). No significant effect of cytokine treatment was observed on the overall yield of CD34+ cells initially isolated from bone marrow or on the number of cells obtained after in vitro culture and retroviral transduction in serum-free medium supplemented with IL-3, SCF, flt3, and the fibronectin fragment CH-296 (Table 1). In general, transduction of CD34+ cells with LZRS/eGFP vector resulted in relatively high levels of eGFP expression (Figure1). Bone marrow cells from animals that were not treated with cytokines (nos. 96-97, 254-97) demonstrated variable levels of eGFP expression (14% and 41%, respectively), with comparable differences in the level of CFU expressing eGFP (Table 1). Animals treated with G-CSF alone had lower levels of transduction efficiency of both bone marrow cells and CFU. Animals treated with the combination of G-CSF and SCF had relatively high levels of transduction of bone marrow cells (mean 58%) and CFU (mean 62%), consistent with previous reports.7 30
Assessment of eGFP expression by rhesus CD34+ cells transduced with the LZRS/eGFP vector.
CD34+ cells were transduced for 3 days with LZRS/eGFP and evaluated by flow cytometry for expression of eGFP. (A) Transduced cells; (B) untransduced cells. FSC indicates forward scatter.
Assessment of eGFP expression by rhesus CD34+ cells transduced with the LZRS/eGFP vector.
CD34+ cells were transduced for 3 days with LZRS/eGFP and evaluated by flow cytometry for expression of eGFP. (A) Transduced cells; (B) untransduced cells. FSC indicates forward scatter.
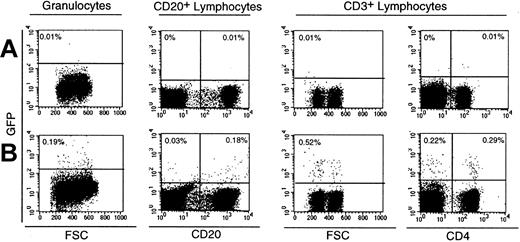
Expression of eGFP in granulocytes and lymphocytes following transplantation
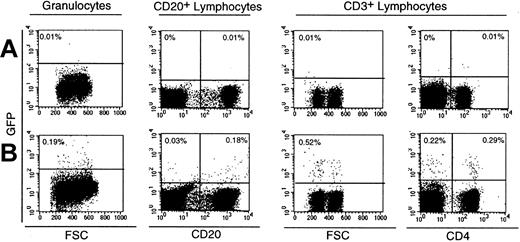
After retroviral transduction of CD34+ cells, all macaques received a nonmyeloablative dose of 240 cGy whole-body irradiation, followed by reinfusion of autologous transduced CD34+ cells. Whether the animals were treated with cytokines or not, the nonmyeloablative doses of radiation used in this study were well tolerated and resulted in only transient myelosuppression. In animals not receiving cytokine treatment, mean absolute neutrophil counts at nadir were 369/μL and platelet counts were 99 000/μL; the duration of neutropenia was approximately 3 days. The use of eGFP as a reporter gene allowed us to rapidly and precisely quantitate the level of gene expression in different subsets of leukocytes following transplantation. Using multiparameter flow cytometry, we determined the percentage of eGFP-expressing cells in granulocytes and CD20+ and CD3+ lymphocytes. Representative data are shown in Figure2.
Assessment of eGFP expression in leukocytes in a macaque following reinfusion of transduced CD34+ cells.
Flow cytometric detection of eGFP in peripheral blood leukocytes in an untransplanted animal (A) and in animals having transplantation with CD34+ bone marrow cells transduced with LZRS/eGFP (B). eGFP+ cells are shown in granulocytes (Mm 280-97) and CD20+ B cells (Mm 278-97) 3 weeks after transplantation (B). CD3+ T cells from Mm 280-97 at 5 weeks after transplantation were analyzed to demonstrate eGFP expression in CD3+CD4+ cells as well as CD3+CD4− cells, 93% of which were CD8+. Gates for expression of eGFP were established using an untransplanted animal as a control at each time point examined. The percentage of gated cells in each quadrant is indicated.
Assessment of eGFP expression in leukocytes in a macaque following reinfusion of transduced CD34+ cells.
Flow cytometric detection of eGFP in peripheral blood leukocytes in an untransplanted animal (A) and in animals having transplantation with CD34+ bone marrow cells transduced with LZRS/eGFP (B). eGFP+ cells are shown in granulocytes (Mm 280-97) and CD20+ B cells (Mm 278-97) 3 weeks after transplantation (B). CD3+ T cells from Mm 280-97 at 5 weeks after transplantation were analyzed to demonstrate eGFP expression in CD3+CD4+ cells as well as CD3+CD4− cells, 93% of which were CD8+. Gates for expression of eGFP were established using an untransplanted animal as a control at each time point examined. The percentage of gated cells in each quadrant is indicated.
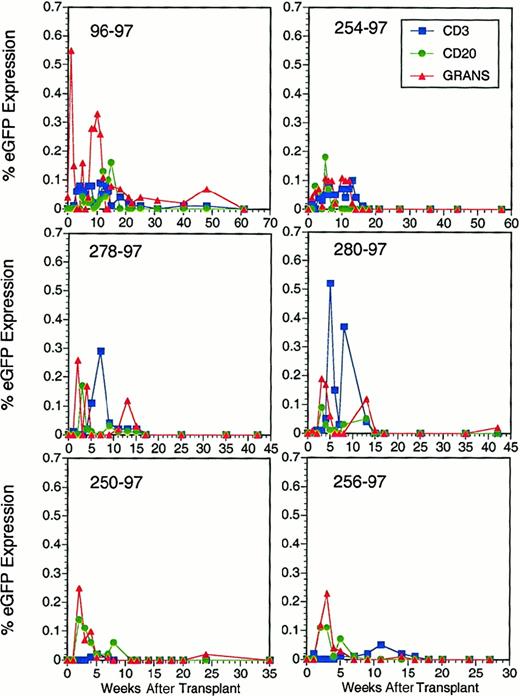
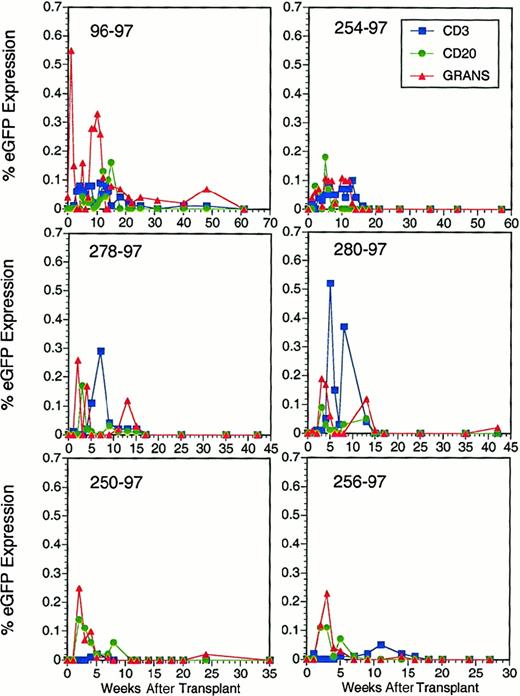
Generally similar patterns of eGFP expression were observed in all 6 animals studied. Early peaks of 0.18% to 0.55% eGFP-expressing granulocytes were observed at 1 to 2 weeks after transplantation, followed by a decline and then loss of eGFP expression in most animals after 10 weeks (Figure 3). Levels of eGFP-expressing B cells were generally low (less than 0.2%) in all animals and declined to undetectable levels after 15 weeks. Peak levels of eGFP expression in T lymphocytes generally occurred at 5 to 7 weeks and subsequently declined to undetectable levels in all animals after 10 to 15 weeks. Interestingly, despite lower levels of transduction of CD34+ cells and CFU, animals treated with G-CSF alone did not demonstrate clear differences in the levels of eGFP-expressing cells in vivo and tended to have higher levels of eGFP expression in T lymphocytes than the other animals. However, regardless of the administration of cytokines, levels of eGFP expression in all leukocyte subsets ultimately declined to undetectable levels in all animals by 17 weeks after transplantation.
Quantitation of eGFP expression in lymphocytes and granulocytes in macaques following reinfusion of transduced CD34+ cells.
Flow cytometric detection of eGFP in CD3+ T cells, CD20+ B cells, and granulocytes at sequential time points after transplantation with autologous CD34+ bone marrow cells transduced with LZRS/eGFP. Reported levels of eGFP expression reflect values obtained after subtraction of the background staining of concurrent negative controls consisting of blood samples from normal animals. Percent eGFP expression in negative controls was always less than 0.1%.
Quantitation of eGFP expression in lymphocytes and granulocytes in macaques following reinfusion of transduced CD34+ cells.
Flow cytometric detection of eGFP in CD3+ T cells, CD20+ B cells, and granulocytes at sequential time points after transplantation with autologous CD34+ bone marrow cells transduced with LZRS/eGFP. Reported levels of eGFP expression reflect values obtained after subtraction of the background staining of concurrent negative controls consisting of blood samples from normal animals. Percent eGFP expression in negative controls was always less than 0.1%.
Analysis of the level of genetically modified PBMCs using PCR primers specific for the MLV packaging sequence revealed generally similar patterns of gene marking as those observed by flow cytometric analysis of eGFP expression (Table 2). In animal Mm 96-97, an initial peak of 0.15% in PBMCs was observed at 3 weeks after infection, followed by a progressive decrease to 0.01% or less at 25 weeks. Similar early, low-level peaks in MLV DNA at weeks 1 to 3 followed by steady declines were observed in the other 5 animals studied. At the last time points examined, all animals had undetectable levels of MLV DNA in PBMCs (less than 0.01% MLV-DNA+cells).
Analysis of the presence of vector DNA by PCR in CFUs derived from animals after transplantation demonstrated a low but significant level of engraftment of transduced cells in each animal at periods ranging from 5 to 18 weeks after transplantation (Table3). The frequency of MLV-DNA CFU varied from 0% to 17% at the initial time points examined and decreased to undetectable levels in the 2 animals for which repeat samples were available.
On the basis of PCR amplification using primers specific for the MLV amphotropic envelope, no evidence for replication-competent retrovirus was found in any of the 6 animals studied (data not shown).
Thus, independent of the mobilization strategy, eGFP+ cells reached only low levels in peripheral blood leukocytes, and eGFP expression fell to undetectable levels between 5 and 20 weeks after transplantation.
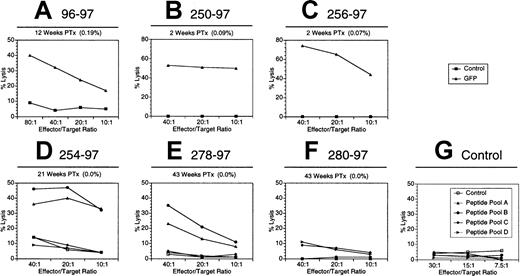
Detection of CTL responses against eGFP
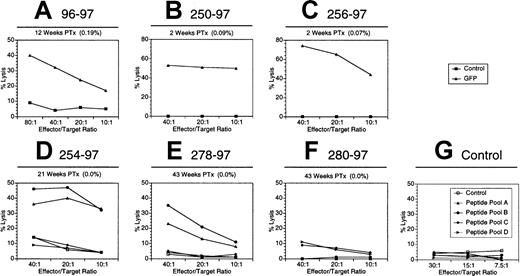
The reproducible loss of eGFP expression in all animals studied prompted us to examine whether induction of a CTL response against eGFP might contribute to decreases in the frequency of eGFP+cells in vivo. To detect eGFP-specific CTLs, we stimulated PBMCs with autologous B-LCLs expressing eGFP antigens and then examined them for their ability to lyse eGFP-expressing target cells. Initial studies in animal Mm 96-97 with the use of eGFP-expressing B-LCLs revealed relatively vigorous eGFP-specific CTL activity at 12 weeks after transplantation (Figure 4A). Similar results were observed at 16 weeks (data not shown) and 25 weeks after transplantation (Figure 5), at which time the percentage of eGFP-expressing cells had declined to less than 0.05% (Figure 3). We were also able to detect eGFP-specific CTLs at 2 weeks after transplantation in animals Mm 250-97 and Mm 256-97 with the use of eGFP-expressing B-LCLs (Figure 4B,C). Similar levels of CTL activity were observed in both animals at 6 weeks after transplantation (data not shown). In animal Mm 254-97, we were unable to obtain a stable autologous B-LCL expressing eGFP and, as an alternative, used stimulator and target cells pulsed with overlapping eGFP peptides. Vigorous eGFP-specific CTL activity was observed 21 weeks after infection, and CTLs lysed target cells sensitized with either of 2 different pools of eGFP peptides (Figure 4D). Examination of eGFP-specific activity at early time points in animals Mm 278-97 and Mm 280-97 was also complicated by difficulties in establishing stable B-LCLs expressing eGFP. However, subsequent assays using peptide–sensitized B-LCLs for stimulation of PBMCs revealed strong CTL activity in Mm 278-97 at 43 weeks after transplantation. When examined 43 weeks after transplantation with peptide-sensitized B-LCLs, only low-level CTL activity was observed in Mm 280-97 (Figure 4F). On the basis of control assays using peptide-stimulated effector cells from 6 GFP-naı̈ve animals (Figure 4G and data not shown), this level of lysis was not significant. Overall, relatively vigorous CTL activity against eGFP was observed in 5 of 6 animals.
Detection of eGFP-specific CTLs in macaques following infusion of autologous CD34+ hematopoietic cells transduced with the LZRS/eGFP vector.
PBMCs were stimulated with autologous B-LCLs either expressing eGFP (A-C) or sensitized with eGFP peptides (D-G). PBMCs shown in G were obtained from an untransplanted control. Stimulated effector cells were examined for eGFP-specific CTL activity using transduced B-LCLs expressing eGFP or sensitized with eGFP peptides. The level of eGFP-expressing leukocytes at the indicated time after transplantation (PTx) is shown. Controls consisted of untransduced autologous B-LCLs.
Detection of eGFP-specific CTLs in macaques following infusion of autologous CD34+ hematopoietic cells transduced with the LZRS/eGFP vector.
PBMCs were stimulated with autologous B-LCLs either expressing eGFP (A-C) or sensitized with eGFP peptides (D-G). PBMCs shown in G were obtained from an untransplanted control. Stimulated effector cells were examined for eGFP-specific CTL activity using transduced B-LCLs expressing eGFP or sensitized with eGFP peptides. The level of eGFP-expressing leukocytes at the indicated time after transplantation (PTx) is shown. Controls consisted of untransduced autologous B-LCLs.
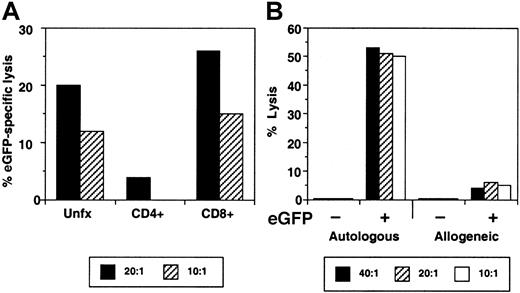
eGFP-specific CTL activity is mediated by CD8+ lymphocytes and is MHC restricted.
(A) Stimulated PBMCs from Mm 96-97 were obtained at 25 weeks after transplantation, separated into CD4+ and CD8+fractions using immunomagnetic beads, and then examined for eGFP-specific CTL activity using an eGFP-expressing autologous B-LCL. (B) Stimulated PBMCs from Mm 256-97 were examined for their ability to lyse eGFP-transduced (+) or -untransduced (−) autologous and allogeneic B-LCLs.
eGFP-specific CTL activity is mediated by CD8+ lymphocytes and is MHC restricted.
(A) Stimulated PBMCs from Mm 96-97 were obtained at 25 weeks after transplantation, separated into CD4+ and CD8+fractions using immunomagnetic beads, and then examined for eGFP-specific CTL activity using an eGFP-expressing autologous B-LCL. (B) Stimulated PBMCs from Mm 256-97 were examined for their ability to lyse eGFP-transduced (+) or -untransduced (−) autologous and allogeneic B-LCLs.
Classic CTL activity is MHC restricted and mediated by CD8+T lymphocytes.31 Fractionation of effector cells into CD4+ and CD8+ T-cell populations with immunomagnetic particles revealed significant eGFP-specific CTL activity only in the CD8+ population (Figure 5A). Similarly, no significant lysis was observed against allogeneic B-LCLs expressing eGFP (Figure 5B).
Identification of eGFP-specific CTL epitopes
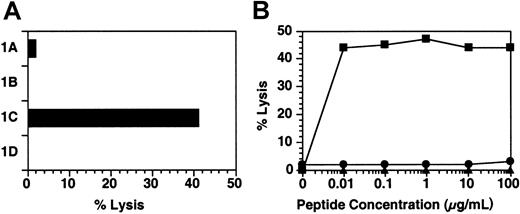
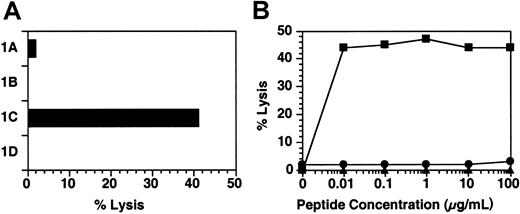
CD8+ CTLs recognize antigenic peptides in the form of 8- to 11–amino acid peptides bound to MHC class I molecules.32 The specific epitopes recognized by CTLs can thus be identified by incubating target cells with synthetic peptides corresponding to the target protein sequence. Using eGFP-specific CTL clones, we mapped CTL epitopes recognized by Mm 96-97. We identified optimal epitopes by examining recognition of a panel of truncated peptides and examining lysis of peptide-sensitized cells over a range of peptide concentrations. A representative example of these titrations is shown in Figure 6. An eGFP-specific CTL clone from animal 96-97 was tested against pools of 20–amino acid peptides corresponding to the eGFP sequence and then against individual peptides. Significant lysis was observed against only one 20–amino acid peptide (data not shown), and the clone was then analyzed for its ability to recognize overlapping 12–amino acid peptides (Figure 6A) and then 9–amino acid peptides (Figure 6B). A total of 3 eGFP epitopes were fine mapped in this fashion (Table4). One of the epitopes was recognized by CTL lines obtained from 2 different animals (250-97 and 254-97). These animals are likely to share a class I MHC allele because CTL clones from these animals could lyse each other's peptide-sensitized B-LCLs (data not shown). Thus, the eGFP protein possesses multiple epitopes that can be recognized by host CTL responses.
Fine mapping of CTL epitopes recognized by clone 96.5.
The CTL clone 96.5 was derived from eGFP-stimulated PBMCs from animal Mm 96-97. (A) Initial mapping of eGFP epitopes. Eleven to 12–amino acid peptides, overlapping by 8 to 9– amino acids, were synthesized. Specific sequences were: 1A, MVSKGEELFTGV; 1B, GEELFTGVVPIL; 1C, FTGVVPILVELD; and 1D, VVPILVELDGD. Autologous B-LCLs were sensitized with 100 μg/mL and tested for lysis using clone 96.5 at an effector-to-target ratio of 10:1. (B) Fine mapping of epitope specificity of CTL clone 96.5. Nine–amino acid peptides corresponding to the sequence of peptide 1A were used to sensitize target cells at the indicated concentrations. Peptide sequences were as follows: 1E (▴), FTGVVPILV; 1F (●), TGVVPILVE; 1G (▪), GVVPILVEL.
Fine mapping of CTL epitopes recognized by clone 96.5.
The CTL clone 96.5 was derived from eGFP-stimulated PBMCs from animal Mm 96-97. (A) Initial mapping of eGFP epitopes. Eleven to 12–amino acid peptides, overlapping by 8 to 9– amino acids, were synthesized. Specific sequences were: 1A, MVSKGEELFTGV; 1B, GEELFTGVVPIL; 1C, FTGVVPILVELD; and 1D, VVPILVELDGD. Autologous B-LCLs were sensitized with 100 μg/mL and tested for lysis using clone 96.5 at an effector-to-target ratio of 10:1. (B) Fine mapping of epitope specificity of CTL clone 96.5. Nine–amino acid peptides corresponding to the sequence of peptide 1A were used to sensitize target cells at the indicated concentrations. Peptide sequences were as follows: 1E (▴), FTGVVPILV; 1F (●), TGVVPILVE; 1G (▪), GVVPILVEL.
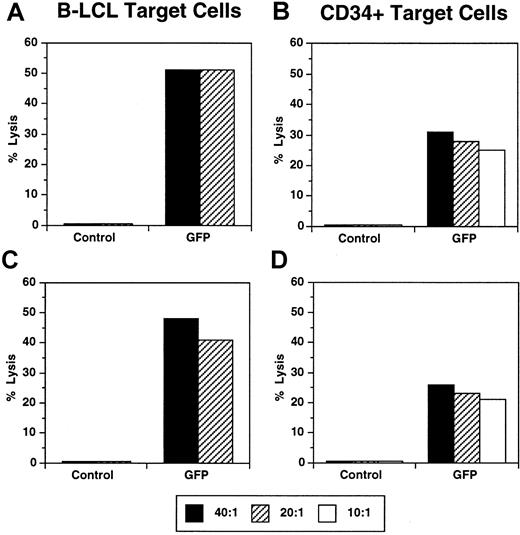
Lysis of GFP-expressing CD34+ cells by CTLs
Transformed B cells are typically used as target cells for CTL assays, in large part because of the ease of culturing B-LCLs and expressing foreign antigens in these cells. However, the ability of CTLs to lyse different hematopoietic lineages expressing foreign genes may vary because of differences in antigen processing or expression of accessory molecules.33 We therefore examined whether eGFP-specific CTLs were able to recognize CD34+ cells expressing eGFP. CD34+ bone marrow cells were isolated from 2 animals, transduced with LZRS/eGFP under optimized conditions, and then used as target cells in standard 51Cr-release assays. eGFP-expressing CD34+ cells were efficiently recognized by eGFP-specific CTLs, but there was minimal or no lysis of autologous CD34+ cells not expressing eGFP (Figure7). Similar results were observed in both animals studied. Overall levels of lysis were only slightly lower than those observed in concurrent assays using eGFP-expressing B-LCLs. Given the lower level of eGFP expression in CD34+ target cells compared with B-LCLs, these data document that CD34+ cells expressing eGFP are also well recognized by eGFP-specific CTLs.
eGFP-specific CTLs lyse autologous CD34+cells transduced with the LZRS/eGFP vector.
eGFP-specific effector cells were generated from animals Mm 250-97 (A,B) and Mm 256-97 (C,D) by stimulation of PBMCs with autologous B-LCLs expressing eGFP and then tested for their ability to lyse either autologous B-LCLs (A,C) or CD34+ cells (B,D). Control target cells consisted of untransduced B-LCLs or CD34+cells. eGFP-expressing B-LCLs were stable cell lines obtained by cell sorting (> 90% eGFP+). eGFP-expressing CD34+cells were generated by transduction with the LZRS/eGFP vector in the presence of IL-3, SCF, and flt3 ligand. Levels of GFP expression were 32% for Mm 250-97 (B) and 54% for Mm 256-97 (D).
eGFP-specific CTLs lyse autologous CD34+cells transduced with the LZRS/eGFP vector.
eGFP-specific effector cells were generated from animals Mm 250-97 (A,B) and Mm 256-97 (C,D) by stimulation of PBMCs with autologous B-LCLs expressing eGFP and then tested for their ability to lyse either autologous B-LCLs (A,C) or CD34+ cells (B,D). Control target cells consisted of untransduced B-LCLs or CD34+cells. eGFP-expressing B-LCLs were stable cell lines obtained by cell sorting (> 90% eGFP+). eGFP-expressing CD34+cells were generated by transduction with the LZRS/eGFP vector in the presence of IL-3, SCF, and flt3 ligand. Levels of GFP expression were 32% for Mm 250-97 (B) and 54% for Mm 256-97 (D).
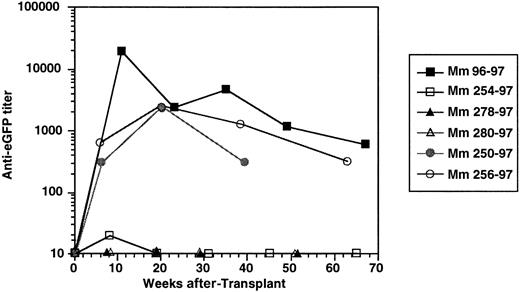
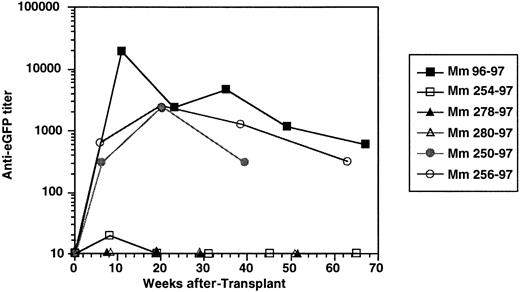
Antibody responses against eGFP
Antibody responses against eGFP were serially evaluated by ELISA in all animals. Three of 6 animals (Mm 96-97, Mm 250-97, and Mm 256-97) developed relatively strong antibody responses against eGFP, with anti-eGFP titers reaching as high as 1:20 000 (Figure8). Titers generally peaked 12 to 20 weeks after transplantation and declined thereafter, but some were still elevated as long as 68 weeks after transplantation. Interestingly, neither of the G-CSF–primed animals (Mm 278-97 and Mm 280-97) developed an antibody response against eGFP. The other animal that did not develop eGFP-specific antibodies was the unprimed animal that had the lowest level of in vivo gene marking (Mm 254-97).
Induction of antibody responses to eGFP.
Antibody titers reflect end-point dilution titers to eGFP as determined by ELISA.
Induction of antibody responses to eGFP.
Antibody titers reflect end-point dilution titers to eGFP as determined by ELISA.
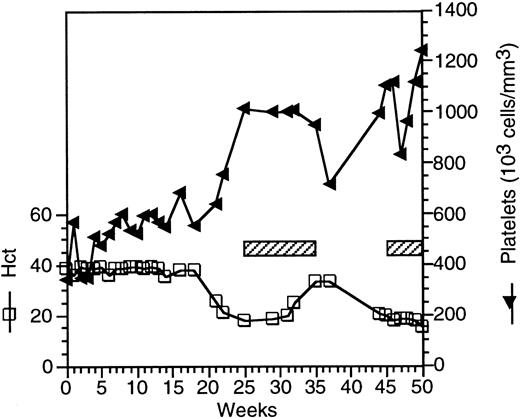
Development of hemolytic anemia after transplantation with LZRS/eGFP-transduced CD34+ cells
One of the animals (250-97) that underwent autologous transplantation of LZRS/GFP-transduced cells after G-CSF/SCF priming developed anemia 20 weeks after transplantation, with the hematocrit decreasing to 20% (normal, 36% to 44%). This decrease was observed after a stable hematocrit of 0.36 to 0.39 (36% to 39%) had been maintained between 5 and 20 weeks after transplantation when blood was being collected infrequently. This animal also developed thrombocytosis (Figure 9) but maintained normal levels of polymorphonuclear leukocytes and lymphocytes (data not shown). Because of a clinical diagnosis of hemolytic anemia, the animal was placed on immunosuppressive therapy with prednisone and azathioprine. After 8 weeks of therapy, the hematocrit began to increase, and the immunosuppressive therapy was gradually tapered and then discontinued. Five weeks after discontinuing prednisone and azathioprine, the animal again developed a profound anemia, with the hematocrit decreasing to 0.17 (17%). The lactate dehydrogenase (LDH) level at this time was 2027 U/L (normal, 0-785 U/L), haptoglobin was less than 0.08 g/L (8 mg/dL) (normal, 0.64-1.92 g/L [64-192 mg/dL]), and reticulocyte count was 4.2%. Cultures for simian retrovirus D, which has been associated with anemia in macaques,34 were negative. Immunosuppressive therapy was resumed with prednisone and azathioprine, but the hematocrit dropped to 15% at 50 weeks after transplantation, and the animal was euthanized at that time. Findings at necropsy included a hypercellular bone marrow biopsy with stainable iron and early erythroid maturation, a relative lack of mature erythrocytes, and abundant deposition of hemosiderin in renal tubules. No evidence of opportunistic infections, including parasitic or viral infections, was identified. These pathologic findings, in combination with the elevated LDH and low haptoglobin, are diagnostic of a hemolytic anemia. An additional animal, 96-97, had a transient neutropenia of 416 to 1000 cells/μL between 18 and 48 weeks after transplantation, which resolved thereafter and was not associated with any known infection. None of the other animals studied had any hematologic abnormalities that persisted after recovery from whole-body irradiation.
Development of hemolytic anemia in macaque Mm 250-97 following transplantation with LZRS/eGFP-transduced CD34+cells.
Hematocrit (Hct) and platelet counts are shown at the indicated times after transplantation. The hatched bar indicates the duration of immunosuppressive therapy with prednisone and azathioprine.
Development of hemolytic anemia in macaque Mm 250-97 following transplantation with LZRS/eGFP-transduced CD34+cells.
Hematocrit (Hct) and platelet counts are shown at the indicated times after transplantation. The hatched bar indicates the duration of immunosuppressive therapy with prednisone and azathioprine.
Discussion
The initial aim of this study was to evaluate the use of hematopoietic growth factors to increase levels of gene marking in vivo following retroviral transduction of CD34+ hematopoietic cells. With or without cytokine pretreatment, we observed peak levels of eGFP-expressing T lymphocytes and granulocytes of between 0.1% and 0.5% at 1 to 3 weeks after transplantation, declining to undetectable levels in peripheral blood by 20 weeks after transplantation. However, in 5 of 6 animals studied, we detected a relatively vigorous CTL response against eGFP, which was able to lyse both eGFP-expressing B-LCLs and CD34+ cells. Antibody responses to eGFP were also detected in 3 of 6 animals after transplantation. In animals that could be studied at the early time points after transplantation, the onset of eGFP-specific CTL responses was temporarily associated with a rapid decrease in the level of eGFP-expressing cells. Using PCR, we were unable to detect persistence of the transgene in PBMCs, although vector sequences were detectable in CFUs in some animals after disappearance of MLV sequences from peripheral blood.
The kinetics of the induction of eGFP-specific CTL responses and their consistent detection in 5 of 6 animals studied suggest that induction of an immune response to eGFP contributed to the clearance of eGFP-expressing cells in peripheral blood. An alternative explanation is that the transient detection of genetically modified cells in peripheral blood reflected a failure to achieve engraftment of transduced bone marrow cells. We believe this latter interpretation is unlikely for several reasons. First, we detected eGFP-expressing cells in multiple lineages (granulocytes, B lymphocytes, T lymphocytes) following infusion of purified CD34+ cells, thus indicating in vivo differentiation. Second, analysis of the presence of vector DNA in CFUs showed engraftment of genetically modified cells in bone marrow for periods of up to 18 weeks after transplantation. Interestingly, low levels of vector DNA in CFUs persisted in some animals even after loss of detectable transduced cells in peripheral blood, a phenomenon previously observed by Lutzko et al.11 The level of gene marking in CFUs did appear to exceed that observed in peripheral blood, a finding previously observed in some35-37 but not all3 large-animal models and human clinical trials. Although the use of nonmyeloablative irradiation in this study (240 cGy) may have contributed to the low levels of genetically modified cells that we observed in peripheral blood, long-term persistence of transduced cells has been observed in at least 2 studies also using nonmyeloablative irradiation, albeit at higher doses than we used (320-500 cGy).8 38 Further studies directly comparing the survival of cells containing immunogenic or nonimmunogenic vector DNA in the setting of nonmyeloablative conditioning will be necessary to rigorously evaluate the role of immune responses in limiting persistence of genetically modified cells following autologous bone marrow transplantation.
Many reports have suggested that induction of immune responses against foreign genes introduced into hematopoietic stem cells occurs infrequently. For instance, in macaques conditioned with nonmyeloablative irradiation, Rosenzweig et al8 observed 5% to 10% murine CD24-expressing cells for up to 4 to 6 months. Similarly, studies using either MLV or lentiviral vectors in macaques receiving myeloablative irradiation have demonstrated sustained expression of eGFP in 1% or more of multiple hematopoietic lineages up to 40 weeks after transplantation in nonhuman primates.6,15 Although detailed analysis of immune responses was not carried out in these studies, the persistent expression of foreign genes and the infrequent observance of CTL responses against the reporter gene in the one study that examined CTL responses8 suggested that induction of immune responses against foreign genes introduced into hematopoietic stem cells in the setting of myeloablative or nonmyeloablative irradiation was relatively uncommon. This issue has been examined in detail by Heim et al,9 who analyzed the induction of immune responses to the reporter gene neo introduced into hematopoietic stem cells following autologous bone marrow transplantation. In macaques that received myeloablative irradiation, no difference in long-term expression was observed between cells transduced with an expressedneo gene and those transduced with a nonexpressed gene. However, infusion of T lymphocytes transduced with the expressedneo gene in naı̈ve animals resulted in induction of antibody responses to neomycin phosphotransferase, whereas long-term persistence of neo-expressing T cells was observed in animals that had undergone bone marrow transplantation withneo-expressing bone marrow cells. These results provide rigorous documentation that in the setting of myeloablative irradiation, expression of transgenes in hematopoietic stem cells and their progeny can induce tolerance and result in long-term persistence of transgene-expressing cells. These results contrast with those obtained by Lutzko et al,11 who observed the generation of antibody responses and proliferative responses in dogs deficient for this enzyme to α-L-iduronidase following autologous bone marrow transplantation with transduced bone marrow cells. The notable difference between this study and those involving nonhuman primates6,8,15 is that no radiation or other conditioning regimen was used for the dogs studied by Lutzko et al.11
Several factors are likely to determine whether transplantation of genetically modified hematopoietic stem cells results in induction of immune responses or tolerance, including the amount of irradiation used for conditioning, the immunogenicity of the transgene, and the degree of expression of neoantigens in the thymus. Myeloablative irradiation induces not only depletion of bone marrow progenitors, but also immunosuppression, in large part because of the depletion of the total-body T-cell pool.39 Intrinsic differences in the immunogenicity of eGFP and murine CD24, which differs only in 6 of 94 amino acids from human and macaque CD24, may explain in part why CTLs were less frequently observed (1 of 4 animals) in the previous report by Rosenzweig et al,8 who also used nonmyeloablative irradiation. The degree of expression of neoantigens in the thymus may also play a role. Expression of novel antigens in the thymus is a potent means to induce tolerance by eliminating production of new T cells that recognize a specific neoantigen.17 This approach has been used to induce tolerance to alloantigens and xenoantigens following bone marrow transplantation.16,40In the studies by Rosenzweig et al8 and Heim et al,9 animals that had the lowest levels of gene marking appeared to be predisposed to develop immune responses against the transgene and to eliminate transgene-expressing cells. There may therefore be a minimal threshold of expression of foreign genes after transplantation of transduced hematopoietic stem cells that is required to induce tolerance. Hematopoietic growth factors used to prime hematopoietic cells or to facilitate hematopoietic reconstitution following irradiation may also affect induction of immune responses. G-CSF has been reported to induce mobilization of T-helper type-2 dendritic cells in humans.41 Interestingly, neither of the animals that received G-CSF alone in our study developed antibodies to eGFP. In sum, we propose that induction of immune responses against transgenes expressed in hematopoietic stem cells will reflect the combined effects of the following: (1) the degree of immunosuppression induced by the conditioning regimen; (2) the immunogenicity of the transgene; (3) the extent of gene expression in transduced cells in vivo; and (4) other factors, including the MHC type of the animal and the use of hematopoietic growth factors.
Because most stem cell gene-therapy protocols currently used in human clinical trials involve no conditioning or relatively nontoxic conditioning unless there is an independent indication for myeloablation, the results we observed in animals in this study may well be applicable to human stem cell gene-therapy trials. Immune responses may be induced not only against foreign genes such as eGFP or transdominant viral proteins, but also to normal human proteins that might be introduced into subjects with congenital disorders. Because CTLs can recognize differences of a single amino acid within a 9- to 11–amino acid epitope even for a host protein,42 CTL responses may also be directed to normal host proteins that differ only slightly from the mutant form expressed in the recipient host. The induction of CTL responses against novel transgenes has also been observed previously in subjects who received infusions of autologous T cells transduced with a retroviral vector expressing a hybrid thymidine kinase and hygromycin gene.13 CTL responses against eGFP in a murine model following infusion of eGFP-expressing syngeneic cell lines or dendritic cells were also reported recently.43
The causal relation between the introduction of eGFP into CD34+ hematopoietic cells and hemolytic anemia or neutropenia observed in 2 of these animals is unknown. In our experience at New England Regional Primate Research Center, the incidence of either neutropenia or hemolytic anemia in animals not infected with simian immunodeficiency virus or other pathogenic retroviruses is uncommon, affecting less than 5% of all animals (unpublished data). Precise estimates of the incidence of hemolytic anemia in nonhuman primates are not available, but available evidence suggests that profound anemias, as observed in animal Mm 250-97, are quite uncommon.44 A detailed autopsy revealed no evident cause for anemia. In murine models, induction of an immune response to a foreign antigen, especially after viral infection, may lead to autoimmune disease.45 However, in light of the relatively small number of animals analyzed in our study, it is not possible to determine definitively whether induction of immune responses against GFP may have contributed to the hemolytic anemia.
In conclusion, our results document the induction of CTL and antibody responses against eGFP in macaques that received autologous infusions of MLV/eGFP-transduced CD34+ cells. In animals that could be evaluated early after transplantation, the detection of an eGFP-specific CTL response was temporarily associated with a decline to undetectable levels. These results dictate caution in the introduction of potentially immunogenic genes into hematopoietic stem and progenitor cells in human clinical trials.
We thank Garry Nolan for providing the LZRS retroviral vector and Phoenix packaging cell line, Graham Molineaux and Amgen for providing recombinant SCF, Prabhat K. Sehgal and Mike Casto for expert care of the animals, Maurice Gately for providing recombinant IL-2, Johnson Wong for providing rhesus CD3-specific monoclonal antibodies, Robert Donahue and Steve Braun for helpful suggestions, Michelle Elliott and Meredith Simon for histopathologic examination, David Sachs for providing access to the large-animal irradiator facility, Donna Hempel and Lou Alexander for preparation of the LZRS/eGFP vector, and Carolyn A. O'Toole for manuscript preparation.
Supported by National Institutes of Health grants RR00168, AI39423, and CA73473.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
R. Paul Johnson, Division of Immunology, New England Regional Primate Research Center, Harvard Medical School, One Pine Hill Dr, PO Box 9102, Southborough, MA 01772; e-mail:paul_johnson@hms.harvard.edu.