Abstract
Donor T cells play a pivotal role in facilitating alloengraftment but also cause graft-versus-host disease (GVHD). Ex vivo T-cell depletion (TCD) of donor marrow is the most effective strategy for reducing GVHD but can compromise engraftment. This study examined an approach whereby donor T cells are selectively eliminated in vivo after transplantation using transgenic mice in which a thymidine kinase(TK) suicide gene is targeted to the T cell using a CD3 promoter/enhancer construct. Lethally irradiated B10.BR mice transplanted with major histocompatibility complex (MHC)–incompatible TCD C57BL/6 (B6) bone marrow (BM) plus TK+ T cells were protected from GVHD after treatment with ganciclovir (GCV) in a schedule-dependent fashion. To examine the effect of GCV treatment on alloengraftment, sublethally irradiated AKR mice underwent transplantation with TCD B6 BM plus limiting numbers (5 × 105) of B6 TK+ T cells. Animals treated with GCV had comparable donor engraftment but significantly reduced GVHD when compared with untreated mice. These mice also had a significantly increased number of donor splenic T cells when assessed 4 weeks after bone marrow transplantation. Thus, the administration of GCV did not render recipients T-cell deficient, but rather enhanced lymphocyte recovery. Adoptive transfer of spleen cells from GCV-treated chimeric mice into secondary AKR recipients failed to cause GVHD indicating that donor T cells were tolerant of recipient alloantigens. These studies demonstrate that administration of TKgene–modified donor T cells can be used as an approach to mitigate GVHD without compromising alloengraftment.
Introduction
The engraftment of allogeneic bone marrow (BM) is thought to be dependent on the ability of transplanted donor immune effector cell populations to eradicate or inactivate host cells capable of mediating rejection of donor hematopoietic stem cells.1-3 A significant body of evidence indicates that donor T cells have a major role in this process. Clinical trials have shown that T-cell depletion (TCD) of donor marrow almost invariably leads to higher rates of graft rejection.4-6 Moreover, this premise is supported by murine models of transplantation where the addition of graded doses of donor T cells to the marrow inoculum has been able to overcome graft resistance in major histocompatibility complex (MHC)–incompatible donor/recipient strain combinations.3
Although T cells are able to promote engraftment, they also play a critical role in the induction of graft-versus-host disease (GVHD), which is the major complication of allogeneic bone marrow transplantation (BMT). T-cell recognition of alloantigens in the context of MHC molecules is the initiating stimulus for graft-versus-host (GVH) reactivity.7-11 Thereafter, T cells are thought to mediate tissue destruction either directly or indirectly by recruiting secondary immune effector populations (macrophages, natural killer cells, etc), which results in an amplification of immune reactivity and dysregulated cytokine production.12-15 From a clinical perspective, the pivotal role that T cells play in the pathogenesis of GVHD results in the fact that durable engraftment in many patients is achieved at the expense of increased toxicity from GVHD, particularly in mismatched related and unrelated BMT.16 Furthermore, because morbidity and mortality from GVHD are inversely proportional to the degree of donor/recipient histocompatibility,16 the effective application and expansion of allogeneic BMT into broader clinical settings has been hindered.
The most effective strategy to reduce GVHD has been ex vivo TCD whereby donor T cells are removed from the donor marrow graft before transplantation.17,18 Although this approach has effectively reduced both the incidence and severity of GVHD, there has been a corresponding increase in the risk of graft rejection in some studies. Efforts to overcome graft resistance by increasing the intensity of the conditioning regimen have reduced the incidence of rejection but inadvertently increased regimen-related mortality.19 An alternative strategy is to eliminate host-reactive donor T cells in vivo rather than ex vivo. With this approach, donor T cells are given the opportunity to facilitate alloengraftment, but are eliminated before they can initiate a lethal GVH reaction. This strategy is based on 2 assumptions. The first is that the persistence of mature donor T cells is not required for long-term viability of the marrow graft. The second is that durable engraftment can be achieved before the GVH process progresses to the point where it becomes unresponsive to selective in vivo T-cell elimination (ie, T-cell independent). Whether these assumptions are valid is unknown. To test this hypothesis, we have constructed transgenic mice that have the thymidine kinase (TK) gene targeted to T cells. Transplantation of mature transgenic T cells into MHC-mismatched recipients enables alloreactive donor T cells to be selectively eliminated after exposure to ganciclovir (GCV) allowing these assumptions to be tested.20,21 Prior studies have shown that this strategy can be used to control GVHD in both humans and in murine models.22-24 The effect of this approach on alloengraftment, however, has not been fully studied. The purpose of this study was to assess whether this strategy would allow for preservation of alloengraftment but mitigation of GVHD.
Materials and methods
Mice
C57BL/6 (B6) (H-2b, Thy1.2+) mice were obtained from either The Jackson Laboratories (Bar Harbor, ME) or the National Institutes of Health (Bethesda, MD). AKR/J (H-2k), B10.BR (H-2k), and B6.PL (H-2b, Thy1.1+) mice were purchased from The Jackson Laboratories. All animals were housed in the American Association for Laboratory Animal Care (AALAC)–accredited Animal Resource Center of the Medical College of Wisconsin. Mice received regular mouse chow and acidified tap water ad libitum.
Reagents
Ganciclovir (Cytovene; Roche Laboratories, Nutley, NJ) was dissolved in phosphate-buffered saline (PBS) and stored in aliquots at −20°C. GCV was thawed prior to use and administered to animals intraperitoneally in PBS at a dose of 50 mg/kg per day.
Generation of TK transgenic mice
Plasmid TGE-CD3 containing the murine T cell–specific δ enhancer and promoter25 was obtained from Dr Ronald Evans (Salk Institute, San Diego, CA). The enhancer region was isolated from the plasmid following restriction digestion with BamHI and cloned into the BamHI site of the pBluescript SK vector (Stratagene, La Jolla, CA). The murine CD3 promoter was cut with Pst I and blunted with T4 DNA polymerase. HindIII linkers were ligated to the fragment and, following HindIII digestion, cloned into the HindIII site downstream of the enhancer region. The herpes simplex virus (HSV) type 1 thymidine kinase (TK) gene was excised from the plasmid pHSV-106 (BRL Laboratories, Gaithersburg, MD) with restriction enzymesBglII and PvuII, blunted with DNA polymerase I, large (Klenow) fragment, and cloned into the blunted Cla I site just downstream of the CD3 promoter in the enhancer/promoter SK construct. Proper orientation of all components was confirmed by sequence analysis (Sequenase, United States Biochemical, Cleveland, OH). The transgene was then separated from plasmid sequences following restriction enzyme digestion, agarose gel electrophoresis, and electroelution. Linearized DNA containing the CD3-TK construct was microinjected into C57BL/6 murine blastocysts. Blastocysts were then implanted into pseudopregnant C57BL/6 female mice.
Transgenic mice were identified by polymerase chain reaction (PCR) amplification of tail DNA using TK-specific primers. PCR reactions contained 25 mM of each dNTP, 1.5 mM MgCl2, 10 mM Tris-HCL, pH 8.3; 50 mM KCl, 1 U Taq polymerase (PerkinElmer, Norwalk, CT), and 50 nM TK-specific primers. Reactions consisted of 30 cycles of denaturation at 94°C for 1 minute, annealing at 59°C for 1 minute, and polymerization at 72°C for 1 minute in a programmable heat block (PerkinElmer). The primer sequences used for the amplification of the TK gene were 5′-CAATCGCGAACATCTACACCACA-3′ (sense strand) and 5′-CCGAAACAGGGTAAATAACGTGTC-3′ (antisense strand) and yielded a 593-base pair product.
TK transgene expression
To confirm messenger RNA (mRNA) expression of the TKgene, reverse transcription–PCR (RT-PCR) was performed. Tissue samples were minced with a scalpel, admixed with Trizol reagent (Gibco, Gaithersburg, MD), and homogenized using a 20-gauge needle and 1-cc syringe. After centrifugation, the supernatant was removed and transferred to a new microfuge tube. RNA was isolated after chloroform extraction followed by isopropyl alcohol precipitation. One microgram of total RNA was subjected to first-strand complementary DNA (cDNA) synthesis in a 15-μL reaction for 60 minutes at 37°C according to the manufacturer's instructions (Pharmacia Biotech, Piscataway, NJ). After completion of first-strand cDNA synthesis, 1.5 μL was used for each PCR reaction using the same protocol noted above.
To confirm TK protein expression, Western blot analysis of representative tissues was performed. Briefly, tissues were suspended in RIPA buffer (50 mM Tris-Cl, 150 mM NaCl, 1% Triton X-100, and 0.1% sodium dodecyl sulfate [SDS]) and phenylmethylsulfonyl fluoride and underwent 3 cycles of freeze-thawing in a dry ice/ethanol bath. The suspension was centrifuged and the supernatant quantitated for protein content using a BCA protein assay kit (Pierce, Rockford, IL). Fifty to 100 μg protein lysate from each tissue was then run on a 12.5% SDS-polyacrylamide resolving gel. Protein was transferred onto nylon membranes using a Biorad Trans Blot apparatus (Hercules, CA) (45 minutes at 2 mA/cm2). Detection was performed using the enhanced chemoluminescence (ECL) detection system according to the manufacturer's instructions (Amersham Life Sciences, Buckinghamshire, England). The primary antibody was a rabbit polyclonal anti-TK antibody (obtained from Dr William Summers, Yale University, New Haven, CT) and was used at a dilution of 1:1000. The negative control for these experiments was the HU-143B human fibroblast cell line. This cell line is TK− and was generously provided by Dr R. Orentas (Medical College of Wisconsin, Milwaukee, WI). The positive control was the AKIL murine leukemia cell line26 that was transfected with the TK cDNA by electroporation.
GCV killing assay
Spleen cell suspensions from representative mice were obtained by pressing spleens through wire mesh screens. Erythrocytes were removed from cell suspensions by hypotonic lysis with sterile distilled water. Cells were then resuspended in complete Dulbecco modified essential medium (CDMEM) and 5% fetal calf serum (FCS) and cultured in flasks along with 5 μg/mL concanavalin A (Con A). After 3 days, cell cultures were evenly split into 2 new flasks containing media and interleukin 2 (IL-2; Proleukin, Chiron Therapeutics, Emeryville, CA) at a concentration of 40 IU/mL. GCV (10 μg/mL) was added to one of the 2 flasks. Viable cells as assessed by trypan blue dye exclusion were counted daily for 5 days to determine the degree of cell expansion.
BMT
Bone marrow was flushed from donor femurs and tibias with CDMEM and passed through sterile mesh filters to obtain single-cell suspensions. BM was T cell depleted in vitro with either anti-Thy 1.1 or anti-Thy 1.2 monoclonal antibodies (mAbs) plus low-toxicity rabbit complement (C6 Diagnostics, Mequon, WI). The hybridomas for HO-22-1 (anti-Thy1.1, mouse IgM) and 30-H12 (anti-Thy 1.2, rat IgG2b) antibodies were purchased from the American Tissue Culture Collection (Rockville, MD). BM cells were washed and resuspended in DMEM before injection. Naive donor T cells were obtained by passing erythrocyte-depleted spleen cells once or twice through nylon wool columns to remove non-T cells. Host mice were conditioned with total body irradiation (TBI) administered as a single exposure at a dose rate of 75 cGy using a Shepherd Mark I Cesium Irradiator (J. L. Shepherd and Associates, San Fernando, CA). Irradiated recipients received a single intravenous injection of TCD BM (107cells) with or without added T cells within 24 hours. For studies of GVHD in a fully MHC-mismatched system, B10.BR recipients (H-2k, Thy1.2) were lethally irradiated (900 cGy) and transplanted with TCD B6 BM (H-2b, Thy 1.2) alone or admixed with graded doses of naive B6 TK+ T cells. For studies of engraftment in a fully MHC-mismatched system, AKR recipients (H-2k, Thy1.1) were sublethally irradiated (750 or 850 cGy) and transplanted with TCD B6.PL BM (H-2b, Thy1.1) alone or admixed with graded doses of B6 T cells from TK+mice.
Flow cytometric analysis and assessment of chimerism
The mAbs conjugated to either fluorescein isothiocyanate (FITC) or phycoerythrin (PE) were used to assess chimerism in BMT recipients. FITC–anti-CD8 (clone 53-6.7, rat IgG2a) was purchased from Collaborative Biomedical Products (Bedford, MA). FITC–anti-CD45R (B220, rat IgG2a) and PE–anti-CD8 (clone CT-CD8a, rat IgG2a) were obtained from Caltag (San Francisco, CA). PE–anti-T-cell receptor-αβ (TCR-αβ; clone H57-597, hamster IgG), FITC–anti-Thy1.2 (clone 30-H12, rat IgG2b), PE–anti-CD3 (clone 145-2C11, hamster IgG), PE–anti-Thy1.1 (clone OX-7, mouse IgG1), FITC–anti-CD4 (clone RM4-4, rat IgG2b), PE–anti-Mac-1 (clone M1/70, rat IgG2b), and FITC–anti-H-2Kb (clone AF6-88.5, mouse IgG2a) were all purchased from Pharmingen (San Diego, CA). Peripheral blood was obtained from animals by tail vein bleeds. Red blood cells were removed by Ficoll-Hypaque density gradient centrifugation. Donor T cells and granulocytes were determined by constructing bit maps and staining with either H-2Kb and CD3 or H-2Kb and Mac-1, respectively. Spleen and thymus cells were obtained from chimeras at defined intervals after transplantation, processed into single-cell suspensions, and stained for 2-color analysis. Red cells were removed when necessary by hypotonic lysis. Cells were analyzed on a FACScan flow cytometer (Becton Dickinson, Mountain View, CA). The absolute number of splenic B and donor T cells was determined by analyzing cells within gates that included the entire spleen cell population after exclusion of red cells and nonviable cells by forward- and side-scatter settings. Donor T-cell chimerism was determined by analyzing cells within the lymphocyte gate. Thymocytes were analyzed within gates that included the entire thymus cell population. At least 10 000 cells were analyzed for each determination whenever possible.
Statistics
Group comparisons of parameters of donor T-cell engraftment and thymic and splenic reconstitution were performed using the Mann-WhitneyU test. A P value < .01 was deemed to be significant when pair-wise comparisons were made between 3 groups. Otherwise a P value of < .05 was deemed as significant in 2-group comparisons. Survival curves were constructed using the Kaplan-Meier product limit estimator and compared using the log-rank rest. Mice that were killed for secondary transfer experiments or engraftment studies were censored from the survival analysis at the time of death. A P value < .05 was deemed to be significant in survival experiments.
Results
Derivation and functional characterization of TK transgenic mice
A total of 47 pups were derived from impregnated female animals. Genomic DNA from these offspring was screened using PCR to detect the presence of the TK gene. Seventeen of 47 offspring were positive for the transgene. TK+ mice were mated to normal C57BL/6 animals. Analysis of genomic DNA by PCR revealed second-generation transmission of the transgene in only 6 of 17 lines. All 6 lines were then analyzed by RT-PCR to determine whether the transgene was expressed. RNA from lung, liver, spleen, BM, muscle, thymus, and kidney was obtained and subjected to RT-PCR using TK-specific primers. One line was identified that had expression of the transgene restricted to the spleen and thymus.
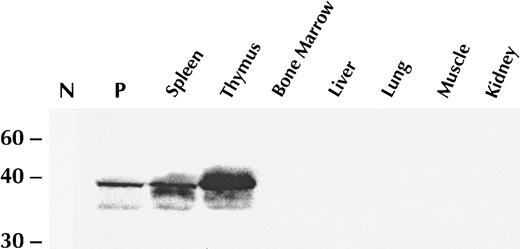
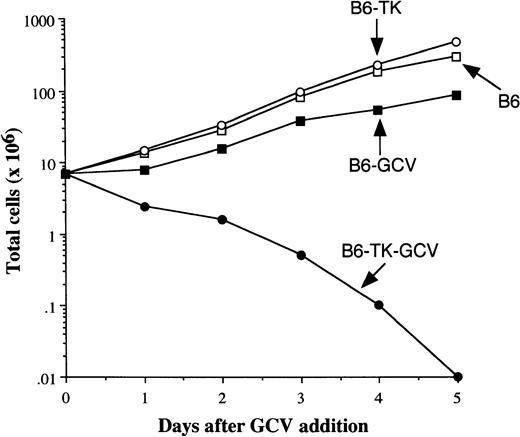
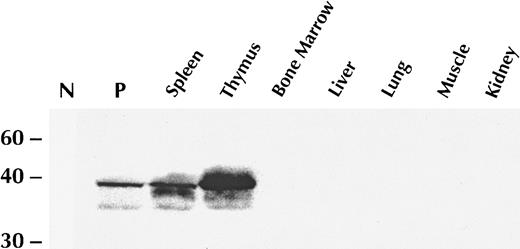
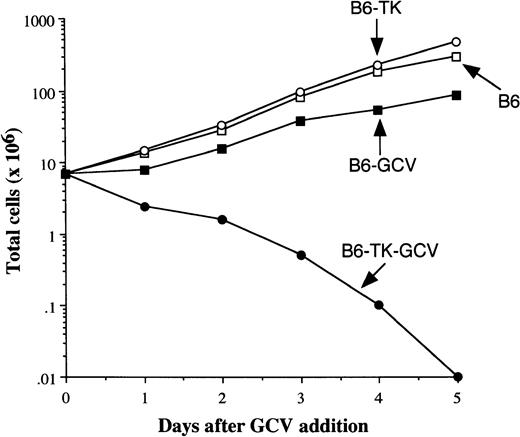
To verify that there was appropriate protein expression of the transgene, Western blot analysis was performed on lysates derived from the same tissues of this founder. These data, which are shown in Figure1, demonstrate that TK protein was detectable only in the spleen and thymus of transgenic animals, but not in the liver, lung, muscle, kidney, or BM. To confirm the functionality of the transgene in T cells, spleen cells from TK+ and TK− mice were activated in vitro with immobilized anti-CD3 antibody and IL-2 for 3 days. Cells were then transferred into fresh flasks and grown in IL-2 ± GCV (10 μg/mL). Cell expansion after addition of GCV was assessed (Figure 2). Spleen cells from TK+ mice rapidly died in vitro, indicating that the transgene was functional in these cells. Normal cells were unaffected by GCV. Activated TK+ T cells cultured in the absence of GCV had growth characteristics similar to TK− cells.
The TK transgene is expressed only in the spleen and thymus.
Western blot analysis of protein lysates derived from specified TK+ founder line tissues were probed with a rabbit polyclonal anti-TK antibody. N signifies the negative control (HU-143B human fibroblast cell line that is TK−). P denotes the positive control (AKR murine leukemia cell line transfected with the TK cDNA).
The TK transgene is expressed only in the spleen and thymus.
Western blot analysis of protein lysates derived from specified TK+ founder line tissues were probed with a rabbit polyclonal anti-TK antibody. N signifies the negative control (HU-143B human fibroblast cell line that is TK−). P denotes the positive control (AKR murine leukemia cell line transfected with the TK cDNA).
Anti-CD3 antibody-activated TK+ T cells are killed by GCV in vitro.
Spleen cells from B6 TK− and TK+ mice were activated in vitro with immobilized anti-CD3 antibody and IL-2 for 3 days. Cells were then transferred into fresh flasks and grown in IL-2 ± GCV (10 μg/mL). The total number of viable cells was monitored over the ensuing 5 days and is depicted for each of the groups.
Anti-CD3 antibody-activated TK+ T cells are killed by GCV in vitro.
Spleen cells from B6 TK− and TK+ mice were activated in vitro with immobilized anti-CD3 antibody and IL-2 for 3 days. Cells were then transferred into fresh flasks and grown in IL-2 ± GCV (10 μg/mL). The total number of viable cells was monitored over the ensuing 5 days and is depicted for each of the groups.
Treatment of recipients of HSV-TK+ T cells with GCV mitigates lethal GVHD in a schedule-dependent fashion
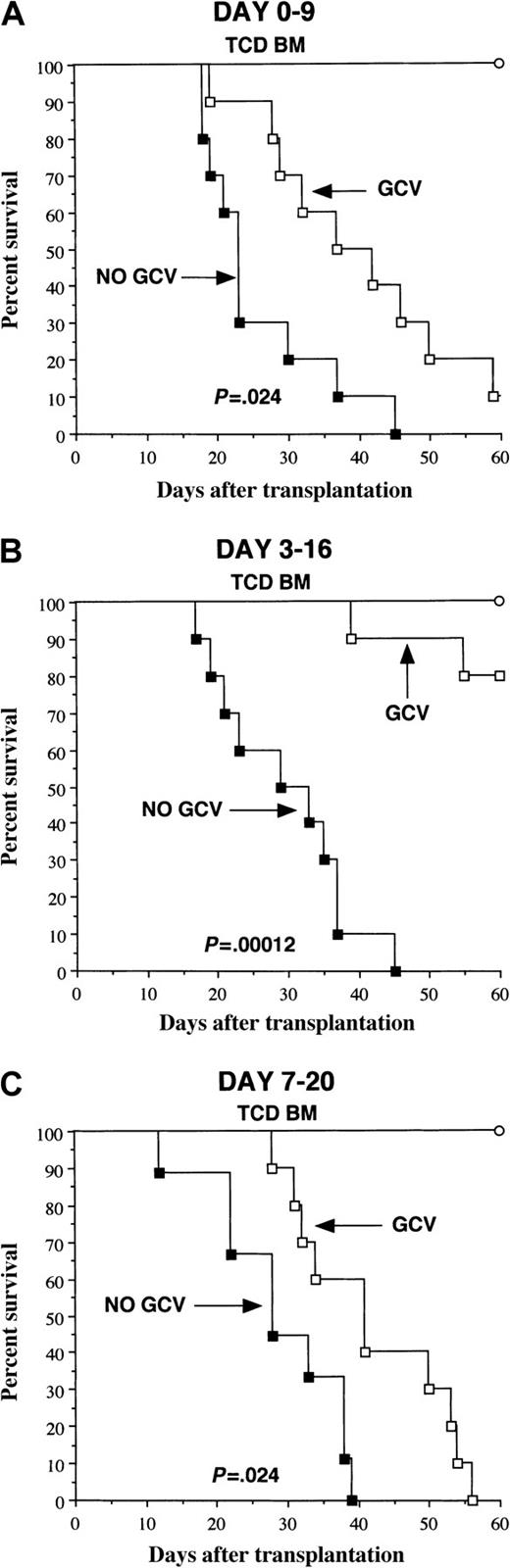
Experiments were performed to confirm that T cells from transgenic mice were capable of causing GVHD and to determine whether the in vivo administration of GCV could ameliorate GVH reactivity in lethally irradiated recipients. B10.BR recipients were transplanted with TCD B6 BM alone (control animals) or together with 3 × 106 B6 TK+ T cells. Untreated mice transplanted with naı̈ve TK+ T cells all died of GVHD within 45 days after BMT, indicating that TK+ T cells were fully capable of causing lethal GVHD (Figure 3). To assess the ability of GCV treatment to reduce the severity of GVHD, similarly transplanted cohorts of mice were administered GCV (50 mg/kg) on one of 3 schedules (ie, days 0-9, 3-16, or 7-20 after transplantation). Treatment with GCV resulted in significantly prolonged survival in all 3 groups when compared to untreated GVHD control mice. Administration of GCV on days 0 to 9 or 7 to 20, however, was less effective than treatment on days 3 to 16 (P < .0001 versus control). The administration of GCV on days 3 to 16 to mice transplanted with normal B6 T cells had no protective effect on GVHD, indicating that GCV itself could not ameliorate GVH reactivity (data not shown). Collectively, these data provided proof of the principle that GCV treatment was capable of protecting animals transplanted with TK+ T cells from GVHD and indicated that protection was, in part, schedule dependent.
GCV treatment mitigates lethal GVHD in mice transplanted with HSV-TK+ T cells.
Lethally irradiated B10.BR mice were transplanted with TCD B6 BM (107) alone (○, n = 6/group) or together with 3 × 106 B6 T cells. Animals transplanted with T cells were then either left untreated (▪, n = 9-10/group) or received the specified schedule of GCV therapy (■, n = 10/group) (panel A, days 0-9; panel B, days 3-16; and panel C, days 7-20). Actual survival is depicted. Data are cumulative results from 2 independent experiments per schedule.
GCV treatment mitigates lethal GVHD in mice transplanted with HSV-TK+ T cells.
Lethally irradiated B10.BR mice were transplanted with TCD B6 BM (107) alone (○, n = 6/group) or together with 3 × 106 B6 T cells. Animals transplanted with T cells were then either left untreated (▪, n = 9-10/group) or received the specified schedule of GCV therapy (■, n = 10/group) (panel A, days 0-9; panel B, days 3-16; and panel C, days 7-20). Actual survival is depicted. Data are cumulative results from 2 independent experiments per schedule.
Selective elimination of donor TK+ T cells after transplantation does not compromise early engraftment
Nontolerant donor T cells are thought to promote engraftment by eliminating host immune cells capable of rejecting marrow cells.3 Donor T cells recognize recipient alloantigens, become activated, undergo clonal expansion, and differentiate into competent cytotoxic T cells. We reasoned that if GCV were given to recipients early after BMT to ameliorate GVHD, it was conceivable that donor T cells might be eliminated before engraftment had occurred. To test this question, we examined the extent of donor engraftment immediately before and after GCV treatment of recipients transplanted with mature TK+ T cells.
Cohorts of sublethally irradiated AKR mice underwent transplantation with TCD B6.PL BM plus 5 × 105 B6 TK+ T cells. This congenic model was used for 2 reasons. The first was so that transgenic T cells could be identified in the recipients, and the second was to determine if there was a correlation between protection from GVHD and elimination of TK+ T cells from the recipient. One group was given GCV on days 4 to 8 after BMT, whereas the other group was left untreated. The GCV schedule was derived from the optimal schedule in GVHD studies with the modification that the duration of administration was shorter due to the fact that GVHD is less severe in this nonmyeloablative (sublethal irradiation) model. Representative animals from each group were killed on day 4 immediately before GCV treatment and on day 9 after the completion of GCV. On day 4, there was only minimal donor T-cell engraftment in the spleen or thymus of either group (Table1). By day 9, donor T cells comprised 97% of all splenic T cells in mice not treated with GCV. The majority of these donor T cells were Thy 1.2+TK+. Transgenic T cells also composed the majority of T cells in the thymus of these animals. Mice treated with GCV had an equivalent degree of donor T-cell chimerism in the spleen; however, the percentage of T cells that were TK+ was significantly reduced (14% versus 77%). The preponderance of donor T cells in the spleens of GCV-treated mice were BM-derived Thy 1.1+ T cells. These data indicate that GCV given on days 4 to 8 did not reduce the percentage of donor T-cell chimerism.
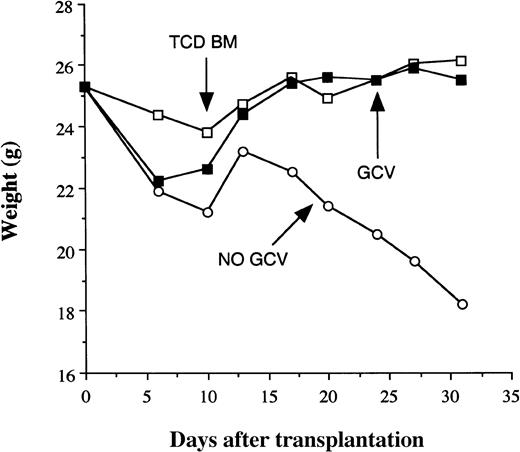
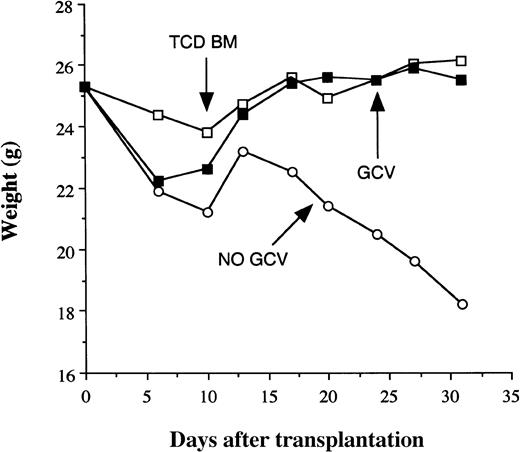
Elimination of HSV-TK+ T cells by GCV reduces GVHD severity without compromising donor engraftment
Studies were then performed to determine whether early donor engraftment was durable and whether GVHD was reduced by elimination of alloactivated donor T cells. Cohorts of sublethally irradiated AKR mice were transplanted with TCD B6.PL BM plus 5 × 105 B6 TK+ T cells. Control mice received TCD BM only. Mice in all groups were killed 3 to 5 weeks after BMT. Animals reconstituted with TK+ T cells but not treated with GCV had lost about 30% of their pretransplant body weight due to GVHD at day 30 (Figure4). Conversely, mice treated with GCV had weight loss that paralleled non-GCV–treated mice for the first 2 weeks, but thereafter regained weight similar to non-GVHD control animals. Mice that did not receive GCV treatment had complete donor T-cell chimerism but significantly reduced splenic and thymic cellularity compared to TCD BM controls, consistent with ongoing GVHD (Table 2). In contrast, although GCV-treated animals had splenic donor T-cell engraftment that was comparable to untreated mice, total spleen size (P < .001) and the number of splenic B cells (P < .001) were significantly increased relative to GVHD controls. The mean percentage of donor cells in GCV-treated versus nontreated mice was also comparable (86% versus 88%), and significantly higher than TCD BM controls (33%). GCV-treated mice also had a striking increase in the percentage of double-positive thymocytes (P < .0001) and overall thymic cellularity (P < .0001), respectively, when compared with untreated animals. Thymic reconstitution was comparable to that observed in non-GVHD control mice. Mice treated with GCV had an increased absolute number of donor T cells in the spleen (Table 2), which was directly attributable to the increase in the number of BM-derived donor T cells (data not shown).
The selective elimination of alloreactive donor T cells mitigates GVHD without compromising engraftment.
Irradiated AKR mice (850 cGy) were transplanted with TCD B6 BM alone (■, n = 9) or TCD BM plus 5 × 105 B6 TK+T cells with (▪, n = 16) or without (○, n = 13) GCV administered after transplantation. GCV was given to animals for either 5 (days 4-8, 2 experiments) or 10 (days 4-13, 1 experiment) days after transplantation and the results were combined. The mean weights of animals are depicted over the first 4 weeks.
The selective elimination of alloreactive donor T cells mitigates GVHD without compromising engraftment.
Irradiated AKR mice (850 cGy) were transplanted with TCD B6 BM alone (■, n = 9) or TCD BM plus 5 × 105 B6 TK+T cells with (▪, n = 16) or without (○, n = 13) GCV administered after transplantation. GCV was given to animals for either 5 (days 4-8, 2 experiments) or 10 (days 4-13, 1 experiment) days after transplantation and the results were combined. The mean weights of animals are depicted over the first 4 weeks.
At a dose of 850 cGy, mice given TCD BM only still had a low level of donor T-cell chimerism. To determine if transplantation ofTK gene-modified cells could facilitate engraftment under conditions where TCD BM was completely rejected, we performed identical experiments at a TBI exposure of 750 cGy. At this TBI dose, mice transplanted with TCD BM only rejected their grafts as assessed by both T-cell and myeloid engraftment (Table 3). Animals transplanted with 5 × 105 B6 TK+ T and treated with GCV on days 4 to 8, however, had a higher incidence of graft rejection compared to untreated mice (4 of 6 versus 1 of 6). When the administration of GCV was delayed until days 8 to 12 after transplantation, donor T-cell and myeloid engraftment was equivalent in both groups. Mice transplanted with TK+ T cells but not treated with GCV lost 16% of their body weight by day 35. Conversely, GCV-treated mice had a 3% gain in body weight that was significantly different at 5 weeks after BMT (P = .004; data not shown). Collectively, these data indicate that GVHD can be substantially reduced without compromising alloengraftment under conditions where engraftment is dependent on the presence of mature donor T cells in the marrow graft.
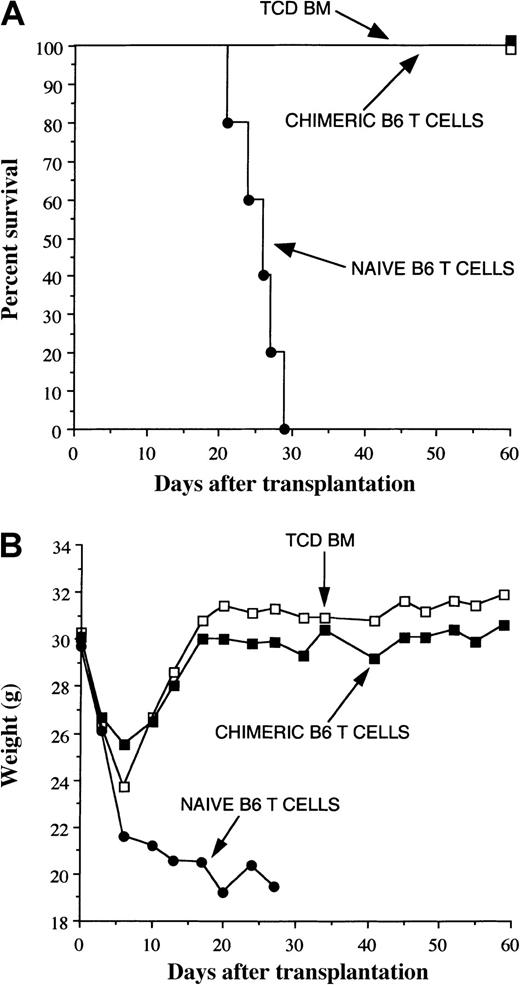
Reconstituting BM-derived donor T cells are tolerant of host alloantigens
The majority of donor T cells in mice after GCV treatment were derived from BM. In the absence of GVHD, these cells undergo thymic selection whereby self-reacting T cells are eliminated before they egress into the periphery. During GVHD this process can become deranged and “autoreactive” BM-derived donor T cells can emerge into the periphery as a consequence of impaired thymic selection.27 These cells have been shown to have antihost reactivity in vitro27 and have been postulated to cause GVHD. Because mice in our studies were allowed to have a limited GVH reaction before GCV was administered, we reasoned that some degree of thymic damage might have occurred before the reaction was abrogated. Thymic phenotyping studies (Table 2) did not reveal any abnormalities consistent with GVHD in GCV-treated mice. As a functional test for tolerance, we performed adoptive transfer experiments into secondary AKR hosts. Splenic T cells from these chimeras (0.5 × 106/mouse) were cotransplanted with normal TCD B6 BM into lethally irradiated secondary AKR recipients. Phenotypic analysis of the chimeric T-cell population indicated that 98% of T cells were donor in origin. Thy1.2+ TK+ T cells represented 5% of all donor T cells, whereas the remaining cells were Thy1.1+ (ie, BM derived). GVHD control mice consisted of lethally irradiated AKR mice transplanted with an equivalent number (0.5 × 106/mouse) of normal B6 Thy 1.2+ T cells. GVHD control animals all died, whereas mice transplanted with chimeric T cells survived without any clinical signs of GVHD (Figure5). These data provided evidence that reconstituting BM-derived donor T cells underwent appropriate thymic selection and that the composite donor T-cell population was tolerant of recipient alloantigens.
Donor T cells from GCV-treated mice are tolerant of host alloantigens.
Irradiated AKR mice (850 cGy) were transplanted with TCD B6 BM plus 5 × 105 B6 TK+ T cells. Mice were then treated with GCV from days 4 to 13 after transplantation. Four weeks after BMT, mice were killed and pooled spleen cells from these animals were cotransplanted with normal TCD B6 BM into lethally irradiated (1100 cGy) AKR hosts (▪, n = 6). Control groups consisted of similarly conditioned mice transplanted with TCD B6 BM alone (■, n = 4) or TCD B6 BM plus 5 × 105 B6 naive T cells (●, n = 5). Survival is depicted in panel A and serial weights in panel B.
Donor T cells from GCV-treated mice are tolerant of host alloantigens.
Irradiated AKR mice (850 cGy) were transplanted with TCD B6 BM plus 5 × 105 B6 TK+ T cells. Mice were then treated with GCV from days 4 to 13 after transplantation. Four weeks after BMT, mice were killed and pooled spleen cells from these animals were cotransplanted with normal TCD B6 BM into lethally irradiated (1100 cGy) AKR hosts (▪, n = 6). Control groups consisted of similarly conditioned mice transplanted with TCD B6 BM alone (■, n = 4) or TCD B6 BM plus 5 × 105 B6 naive T cells (●, n = 5). Survival is depicted in panel A and serial weights in panel B.
Discussion
Donor T cells play a critical role in preventing graft rejection after allogeneic BMT. A number of studies have shown that T cells promote engraftment by eradicating or inactivating host T cells that reject the marrow graft.1-3,6 CD8+ T cells are responsible for preventing graft rejection in mice, primarily by the generation of cytotoxic T cells that eliminate host immune cells,28 although CD8 cells may also mediate veto activity.29-31 In animal models, the number of donor T cells can be adjusted to facilitate engraftment without inducing significant GVHD.3 This goal has been more elusive in clinical BMT where a similar strategy has resulted in a prohibitively high risk of GVHD.32 In this study, we used an alternative approach to address the divergent role of T cells in engraftment and GVHD. We demonstrated that GVHD could be significantly reduced without compromising engraftment of the donor marrow by the selective elimination of alloreactive TK gene–modified donor T cells. These data also indicated that the ability of donor T cells to facilitate alloengraftment could be dissociated from the ability of these same cells to cause lethal GVHD. The dissociation of these 2 events appeared to be based solely on the temporal manipulation of T-cell survival by GCV administration resulting in a limited GVH reaction and not on any inherent property of transgenic T cells to differentially promote engraftment at the expense of GVH reactivity.
The results of this study provide insight into the tempo of donor engraftment early after BMT. Analysis of chimerism 4 days after transplantation demonstrated no evidence of donor T-cell engraftment in either cohort of mice. Host T cells comprised nearly all of the T-cell population. By day 9, however, complete donor T-cell chimerism had been established in the spleens of untreated mice and donor T cells constituted the primary T-cell population in the thymus. These data are consistent with the interpretation that donor T cells are able to eliminate host immune cells capable of rejecting the graft within the first week after transplantation. Notably, GCV treatment on days 4 to 8 did not reduce the level of donor T-cell engraftment in the spleen even though there was a substantial reduction in the percentage of transgenic T cells in these animals. Thus, these cells were able to eradicate host T cells before the majority of TK+ T cells were themselves eliminated by GCV. Although we cannot exclude that the small percentage of residual donor T cells remaining after GCV treatment may have contributed to engraftment, the inability of purified Thy 1.2+ TK+ T cells to cause GVHD in adoptive transfer experiments (unpublished observations, January 2000) suggests that the graft facilitating capability of these cells is negligible.
Despite the administration of GCV and subsequent elimination of alloactivated donor T cells, GCV-treated animals had an increased number of splenic T cells 4 weeks after BMT (Table 2). Thus, the administration of GCV did not render recipients T-cell deficient. Rather, these animals had increased donor T-cell repopulation, presumably due to the reduction in GVHD,33,34 suggesting that this approach may not only mitigate GVHD but also enhance T-cell reconstitution. An important observation is the fact that the majority of donor T cells in GCV-treated mice were derived from BM (Table 1). This contrasted with what was observed in untreated animals where splenic-derived T cells comprised the majority of T cells. BM-derived T cells typically undergo selection in the thymus where they are tolerized to host alloantigens, unless GVHD-induced thymic damage precludes normal deletional mechanisms.27 In these studies, adoptive transfer experiments showed that donor T cells remaining after GCV treatment did not cause clinically significant GVHD (Figure 5). Thus, donor T cells, of which the majority were BM derived, were tolerant of host alloantigens. Whether these T cells are competent to mediate third-party responses against alloantigens and viral infections is a significant question and one that is currently under investigation.
It should be emphasized that TK+ T cells persisted in mice after GCV treatment. There are several possible explanations for this observation. One is that an effective GCV concentration was not maintained at all times that transgenic T cells were proliferating. Hence some alloreactive T cells were able to escape elimination over the 5-day treatment course. An alternative explanation is that residual TK+ T cells did not recognize recipient alloantigens and therefore were nonproliferative. In that regard, we would note that the absolute number of TK+ T cells was approximately the same in both GCV-treated and non-GCV–treated chimeras (Table 2). The fact that the former cohort of mice had significantly reduced GVHD suggests that these residual TK+ T cells were in fact not reactive against recipient alloantigens. Adoptive transfer studies also support the premise that these cells were tolerant of host alloantigens. However, these data are not conclusive. An alternative explanation is that GCV treatment resulted in the more rapid emergence of BM-derived donor T cells, some of which were able to function as regulatory T cells capable of down-regulating GVH reactivity.35 Ongoing studies using purified TK+ T cells in adoptive transfer experiments (see above) are needed to definitively address this question.
A fundamental aspect of this approach is that a GVH reaction is allowed to begin but is abrogated before substantial tissue damage has occurred in the host. The administration of GCV to TK-transplanted animals targets dividing T cells, the majority of which are presumably responding to host alloantigens.36 Several studies have substantiated that this strategy is feasible, although there has been variability in the degree of GVHD protection afforded. In the present study, we observed that administration of GCV over many days to weeks was required for effective GVHD protection. This is in contrast to studies by Lake-Bullock and colleagues23 where the administration of as few as 2 doses of GCV was sufficient for abrogation of GVHD. Cohen and coworkers24 reported more variability in the degree of GVHD protection in their studies. They postulated that this variability stemmed from the use of 2 different transgenic lines of mice that differentially expressed theTK transgene. This was supported by studies showing a difference in GCV-mediated killing in vitro between activated T cells from the respective lines. The level of transgene expression may therefore be one explanation for the variable duration of GCV administration required for effective prevention in different studies. An alternative explanation may lie in differences in the murine transplantation models used to evaluate GVHD. For example, in our studies, a short course of GCV treatment was highly effective in preventing GVHD in sublethally irradiated AKR recipients transplanted with a low dose of donor B6 T cells. Conversely, a more protracted course of GCV gave less protection in lethally irradiated B10.BR recipients transplanted with a 6-fold higher dose of B6 T cells. The implication for clinical BMT is that the administration schedule of GCV may be an important variable in modulating the intensity of the GVH reaction and may vary depending on the intensity of the conditioning regimen and the degree of MHC incompatibility between donor and recipient.
In this study, the addition of mature donor T cells was necessary to overcome graft resistance. Prior studies have shown an inverse correlation between the intensity of the conditioning regimen and the dose of T cells necessary to facilitate alloengraftment.37-39 Thus, less intensively conditioned recipients require larger doses of donor T cells for equivalent engraftment. Our study identifies the GCV administration schedule as another variable that also affects donor engraftment when mice are transplanted with TK+ T cells. At TBI exposures of 850 cGy, a GCV schedule of days 4 to 8 resulted in engraftment in all recipients (Table 2). In contrast, the same schedule resulted in graft rejection in the majority of mice conditioned with 750 cGy (Table 3). The latter group of mice required that GCV be given later after transplantation (ie, days 8-12) for engraftment to be achieved. We infer that this was due to a higher percentage of host T cells surviving the less intense conditioning regimen necessitating that donor T cells persist in the host for a longer period of time. These findings may have implications for human transplantation. In clinical marrow transplantation, there is growing interest in the use of nonmyeloablative conditioning regimens to reduce regimen-related toxicity, particularly in older recipients or those with underlying vital organ dysfunction.40 41 The infusion of large numbers of donor T cells in the stem cell graft, however, has been necessary to overcome graft resistance in patients given nonmyeloablative conditioning and has been shown to cause GVHD. Our data suggest that an alternative approach for these patients may be to infuse larger numbers of donor T cells that have been modified with insertion of the TK gene. However, the current study would argue that the successful application of this approach will be contingent on the careful modulation of conditioning regimen intensity, donor T-cell dose, and GCV administration schedule.
In summary, these results show that the ability of donor T cells to facilitate engraftment and cause GVHD can be dissociated by manipulating survival of alloactivated T cells through gene targeting of the donor T cell. These data also demonstrate that the persistence of host-reactive donor T cells after BMT is not a prerequisite for durable engraftment. The extent to which this strategy may be beneficial in patients with leukemia will depend on whether there is commensurate retention of graft-versus-leukemia reactivity. In nonmalignant conditions (eg, marrow failure syndromes or immunodeficiency disorders), however, where there is no risk of relapse, the ability of TK gene–modified donor T cells to facilitate donor engraftment without causing clinically significant GVHD may expand the spectrum of patients who can benefit from allogeneic BMT.
We would like to thank Tina Agostini and Sanja Jankovic-Vodanovic for their technical assistance in performing the murine transplantation studies. The authors also acknowledge Rob Payne from the NIAID transgenic facility who provided invaluable assistance in helping to establish the founder line. Dr William Summers is acknowledged for providing the thymidine kinase monoclonal antibody. We thank Robert Truitt for critically reviewing the manuscript.
Supported by grants from the American Cancer Society (RPG 9808401), the Charles E. Culpeper Foundation, and the Firefighter's Fund (Milwaukee, WI).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
William R. Drobyski, Bone Marrow Transplant Program, Froedtert Memorial Lutheran Hospital, 9200 W Wisconsin Ave, Milwaukee, WI 53226; e-mail: bill@bmt.mcw.edu.