Morphologic bone marrow changes in patients with BCR-ABL–positive chronic myelogenous leukemia (CML) were investigated during treatment with the tyrosine kinase inhibitor STI571. Bone marrow trephine biopsy specimens from 23 pretreated patients with CML were examined morphologically and by morphometry before and 6 weeks and 3 months after the initiation of STI571 therapy (Glivec, Novartis, Basel, Switzerland). Bone marrow changes during treatment showed a quantitative normalization of erythropoiesis, a marked reduction of granulopoiesis, and a significant decrease in megakaryocytes with the reappearance of normal-sized forms. Furthermore, a significant regression of bone marrow fibrosis was observed in patients with initial fibrosis (P < .000 000 001). These results may expand the profile of STI571 and may offer novel therapeutic possibilities in diseases with bone marrow fibrosis.
Introduction
Philadelphia chromosome—the hallmark of chronic myelogenous leukemia (CML)—results from a reciprocal translocation between the long arms of chromosomes 9 and 22.1 At the molecular level, this fusion generates a chimeric BCR-ABL oncoprotein with constitutive tyrosine kinase activity. Because BCR-ABL alone is sufficient to initiate CML, tyrosine kinase inhibitors were developed as a selective therapy for this disease.2 Clinical trials revealed encouraging results using the tyrosine kinase inhibitor STI571 in the treatment of CML.3-5 Patients treated with STI571 have been monitored clinically and by cytogenetic and molecular analyses; however, only preliminary data are available with respect to bone marrow changes induced by this approach.6 7 We studied the effects of STI571 treatment in bone marrow trephine biopsy specimens, with special emphasis on the progression or reversal of reticulin fibrosis.
Study design
Patients
Thirty-nine patients with BCR-ABL–positive CML were treated at the University Hospital in Graz with STI571 according to a study protocol by Novartis (Basel, Switzerland), which was approved by the ethics committee of the University of Graz. These patients were placed into 3 groups: group 1, patients with chronic-phase CML refractory to interferon (IFN)–α therapy, with less than 10% myeloblasts in the peripheral blood or bone marrow; group 2, patients with accelerated-phase CML as defined by Katarjian et al8; and group 3, patients with CML in blast crisis with 30% or more blast cells in peripheral blood or bone marrow. STI571 monotherapy consisted of 400 mg/d in group 1 and 600 mg/d in groups 2 and 3 without change of dosage during the observation period. Sequential bone marrow biopsy samples were taken in 23 of 39 STI571-treated patients at study entry and at 6 weeks and 3 months after the initiation of STI571 treatment. Twelve women and 11 men were enrolled in the study. Their median age was 60.5 years (range, 35-80 years), and the median duration of CML since diagnosis was 3.6 years (range, 3-144 months). Twenty-two of 23 patients were pretreated with IFN-α at a median dosage of 5 × 106 U/d (range, 1.5-10 × 106 U/d) for a median duration of 24.5 months (range, 2-96 months). One patient received monotherapy with hydroxyurea.
Bone marrow biopsies: morphometry and morphology
With the written, informed consent of the patients, 2 biopsy samples from the posterior iliac crest were taken from each. One biopsy specimen was embedded in methyl-methacrylate7 and was stained with hematoxylin and eosin, Giemsa, Prussian blue, and Gomori stains for reticulin fibers. Immunohistochemical phenotyping with monoclonal antibodies to CD66, CD33, glycophorin C (DAKO, Glostrup, Denmark), and CD61 (Ylem, Italy) was performed on the second biopsy specimen using cryostat sections.9 Morphometric analysis was performed using a semiautomatic image analysis workstation consisting of a microscope with a 3CCD color video camera and a personal computer with image analysis software (Optimas 6.5; Media Cybernetics, Silver Spring, MD).10 Custom macros were developed to calibrate illumination, perform background correction, enhance contrast, and manipulate color planes, automate detection and measurement of objects, and export data to Excel spreadsheets. In immunohistochemical stains, the positive areas were detected using an autothresholding algorithm.10 The entire biopsy area, excepting bones and artifacts, was measured in consecutive fields of view. For each slide, a quotient of the positive areas to the sum of the corresponding specimen area was calculated. Cellularity was measured as a quotient of cellular areas to the entire bone marrow area (including fat cells) at 20 × objective magnification, megakaryocytic size at 60 × objective magnification in at least 15 fields of view in each slide. For measurement of fibrosis, the number of intersections of the fibers with a 20 μm spaced grid on the computer screen was quantified in Gomori-stained slides at 60 × objective magnification. Bone marrow cellularity was also defined semiquantitatively according to Custer11: highly increased bone marrow cellularity was defined as occupation of the total bone marrow by more than 85% of hematopoietic cells, moderately increased by 70% to 84%, slightly increased by 55% to 69%, and normal by 35% to 54%. Bone marrow fibrosis was also assessed semiquantitatively by visual scoring (vs)12 and corresponded to morphometric measurements: vs 0 = 0 intersections/mm [is/mm]; vs 1 = 6.5-14.9 is/mm; vs 2 = 15.0-24.9 is/mm; vs 3 = 25.0-39.9 is/mm; vs 4 = 40.0-75.0 is/mm).
Statistical analysis
Statistical analysis was performed using a program for multilevel statistical modeling MLWin 1.10.13 Slides (biopsy specimens) represented the first level of the hierarchy, nested within the patients (second level). Effects of several factors (group, time point of therapy, STI571 doses) on a number of dependent variables (content of CD61+ cells, cellularity, fibrosis) were modeled. To validate model coefficients and to eliminate bias, nonparametric bootstrap was used. Significance tests were based on χ2 distribution.
Results and discussion
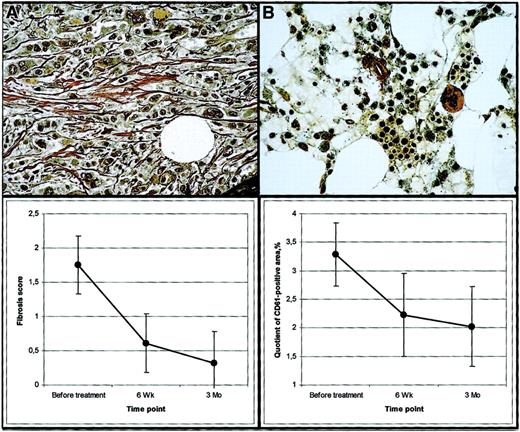
Complete hematologic remission after 3 months of STI571 therapy was found in 9 of 9 patients of group 1, in 6 of 8 patients in group 2, and in 2 of 6 patients in group 3. Major cytogenetic responses were detected in 9 of 9 patients in group 1, in 6 of 8 patients in group 2, and in 0 of 6 patients in group 3. The main morphologic bone marrow changes are summarized in Table 1. Overall, a statistically significant decrease in bone marrow cellularity after 3 months of STI571 therapy was evident (P < .000 000 001). This was attributed to a quantitative normalization of erythropoiesis and a decrease of granulopoiesis and megakaryocytes, seen in methyl-methacrylate–embedded biopsy specimens and confirmed by immunohistochemical stains. Statistical analysis of the decrease in cellularity revealed a significantly better response in group 1 patients than in groups 2 and 3 (P = .0021). In pretreatment biopsy samples, no significant differences in the amount of CD61+ megakaryocytes were detectable between the patient groups (P = .6). Under therapy, a highly significant decrease of CD61+ megakaryocytes in all patient groups was found (P < .000 0001) (Figure1). This reduction of initially small megakaryocytes (median size, 184.1 μm2 [range, 5th-95th percentiles, 81.2 μm2-303.9 μm2]) was associated with the reappearance of normal-sized megakaryocytes (median size, 770.8 μm2 [range 5th-95th percentiles, 334.6 μm2-1164.1 μm2]) and regression of fibrosis (Table 1, Figure 1). Before therapy, bone marrow fibrosis increased from group 1 to group 3 (P = .024). Within 6 weeks therapy and 3 months therapy, a significant regression of fibrosis became evident in all patient groups (P < .000 000 001) (Table 1, Figure 1).
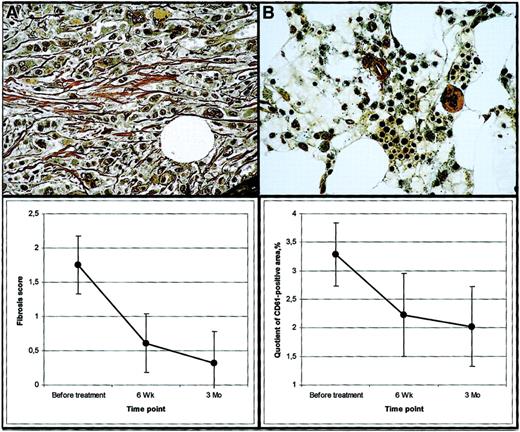
Effects of STI571 treatment on bone marrow fibrosis and megakaryocytes.
(A) Group 3 patient FM. Bone marrow biopsy before STI571 treatment showing marked fibrosis (grade 3). Gomori stain, × 400. (B) Same patient. Bone marrow biopsy after 3-month STI571 treatment without fibrosis (grade 0). Gomori stain, × 400. (C) Estimated dynamics of bone marrow fibrosis during therapy. 0 corresponds to absence of fibrosis. Error bars represent 95% confidence intervals. Estimates were obtained from a multivariate model and are bootstrap-corrected and adjusted for patient grouping. (D) Estimated dynamics of CD61+ megakaryocytes during therapy. Error bars represent 95% confidence intervals. Estimates were obtained from a multivariate model and are bootstrap-corrected and adjusted for patient grouping.
Effects of STI571 treatment on bone marrow fibrosis and megakaryocytes.
(A) Group 3 patient FM. Bone marrow biopsy before STI571 treatment showing marked fibrosis (grade 3). Gomori stain, × 400. (B) Same patient. Bone marrow biopsy after 3-month STI571 treatment without fibrosis (grade 0). Gomori stain, × 400. (C) Estimated dynamics of bone marrow fibrosis during therapy. 0 corresponds to absence of fibrosis. Error bars represent 95% confidence intervals. Estimates were obtained from a multivariate model and are bootstrap-corrected and adjusted for patient grouping. (D) Estimated dynamics of CD61+ megakaryocytes during therapy. Error bars represent 95% confidence intervals. Estimates were obtained from a multivariate model and are bootstrap-corrected and adjusted for patient grouping.
CML is a pluripotent stem cell disorder characterized by the development of a variable degree of bone marrow fibrosis during disease progression or at diagnosis.14,15 Treatment with IFN-α or busulfan may exaggerate the fibrogenic process.16 In this study, we were able to demonstrate a significant regression of bone marrow fibrosis during treatment with the tyrosine kinase inhibitor STI571, which was paralleled by a marked decrease of megakaryocytes. It is generally accepted that megakaryocytes are the principal mediators of fibrogenesis in myeloproliferative disorders, acting through the abnormal release of transforming growth factor–β and platelet-derived growth factor (PDGF).17 STI571 was found to inhibit PDGF in cell-based assays and was originally developed as a specific PDGF receptor inhibitor.18 Regression of bone marrow fibrosis by STI571 in this cohort of patients might have been caused by the normalization of megakaryocytopoiesis. However, it may also well be that STI571 exerted a specific anti-PDGF effect. According to the findings of the German CML trial, the impact of bone marrow fibrosis significantly influences the survival of patients independently of other risk factors and is an important follow-up parameter.19 Our results may, therefore, expand the profile of STI571 and offer novel therapeutic possibilities in diseases with abnormal bone marrow fibrosis.
We thank Mrs E. Steinbauer, Mr M. Al-Effah, and Mag Mr J. Bredac for their excellent technical assistance and Mr R. Staber for excellent electronic artwork
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Christine Beham-Schmid, Institute of Pathology, Karl-Franzens University, Auenbruggerplatz 25, A-8036 Graz, Austria; e-mail: christine.beham@kfunigraz.ac.at.