The incidence of postengraftment invasive aspergillosis (IA) in hematopoietic stem cell transplant (HSCT) recipients increased during the 1990s. We determined risks for IA and outcomes among 1682 patients who received HSCTs between January 1993 and December 1998. Risk factors included host variables (age, underlying disease), transplant variables (stem cell source), and late complications (acute and chronic graft-versus-host disease [GVHD], receipt of corticosteroids, secondary neutropenia, cytomegalovirus [CMV] disease, and respiratory virus infection). We identified risk factors associated with IA early after transplantation (≤ 40 days) and after engraftment (41-180 days). Older patient age was associated with an increased risk during both periods. Chronic myelogenous leukemia (CML) in chronic phase was associated with low risk for early IA compared with other hematologic malignancies, aplastic anemia, and myelodysplastic syndrome. Multiple myeloma was associated with an increased risk for postengraftment IA. Use of human leukocyte antigen (HLA)–matched related (MR) peripheral blood stem cells conferred protection against early IA compared with use of MR bone marrow, but use of cord blood increased the risk of IA early after transplantation. Factors that increased risks for IA after engraftment included receipt of T cell–depleted or CD34-selected stem cell products, receipt of corticosteroids, neutropenia, lymphopenia, GVHD, CMV disease, and respiratory virus infections. Very late IA (> 6 months after transplantation) was associated with chronic GVHD and CMV disease. These results emphasize the postengraftment timing of IA; risk factor analyses verify previously recognized risk factors (GVHD, receipt of corticosteroids, and neutropenia) and uncover the roles of lymphopenia and viral infections in increasing the incidence of postengraftment IA in the 1990s.
Introduction
The most important risk factor for invasive aspergillosis (IA) has historically been neutropenia.1Recently, several groups have reported a large second risk period corresponding with the occurrence of graft-versus-host disease (GVHD) among allogeneic hematopoietic stem cell transplant (HSCT) recipients.2,3 In the cohort of patients who developed IA at the Fred Hutchinson Cancer Research Center (FHCRC) between 1987 and 1993, risk factors identified in multivariable models included transplantation at an older age, having an underlying disease other than chronic myelogenous leukemia (CML) in chronic phase, exposure to construction, transplantation during the summer, prolonged neutropenia, and administration of corticosteroids for treatment of GVHD.2 In this earlier study, the incidence of IA appeared to increase during the first 6 months of 1993.2Our subsequent analyses have verified that the incidence of IA has remained high, with the one-year cumulative incidence approximating 10% in allograft recipients.4
During the past decade, multiple changes in transplant practices have affected the epidemiology of opportunistic infections. In the early 1990s, 2 important supportive care measures were adopted in our center: administration of fluconazole for prevention of candidiasis, and use of pp65 antigenemia or polymerase chain reaction (PCR)–guided ganciclovir administration for prevention of cytomegalovirus (CMV) disease. Both have been successful in preventing infection and mortality attributed to Candida albicans and CMV.5-7 Both strategies have drawbacks, as fluconazole has no activity against molds, and prevention of CMV infection early after transplantation is associated with an increased risk for CMV disease late after transplantation owing to delayed CMV-specific immune reconstitution.8 9 Although several reports have noted that the increased incidence in IA appears to have occurred coincidentally with the introduction of these other preventive strategies, no large studies have been performed to identify specific risks during the latter 1990s. During this period of time, other changes in clinical practices could have affected the risks for IA, including the use of alternative stem cell sources and conditioning regimens. This study was performed to identify the risk factors for IA and outcomes in a large cohort of patients who received allogeneic HSCTs at FHCRC between 1993 and 1998.
Patients and methods
Study patients
Patients who developed invasive fungal infections were identified by examination of a computerized microbiology database, histopathology reports, and prospectively collected hospital epidemiology records. A total of 327 patients developed invasive mold infections at our center between 1993 and 1998.4 In this study, we evaluated the risks among 187 patients who developed proven or probable IA after a first myeloablative allogeneic HSC transplantation between January 1, 1993, and December 31, 1998 (characteristics of entire cohort in Table1). This study was approved by the FHCRC institutional review board.
Characteristics and outcomes of the cohort of patients who received allogeneic HSCTs at FHCRC, 1993-1998 (n = 1682)
| . | No. (%) . |
|---|---|
| Median recipient age, y (range) | 37 (0-68) |
| Male sex | 1013 (60.2) |
| Underlying diagnosis | |
| CML, chronic phase | 404 (24.0) |
| Hematologic malignancy, first remission | 166 (9.9) |
| Hematologic malignancy, other | 729 (43.3) |
| Other | 383 (22.8) |
| Donor and stem cell source | |
| MR BM | 566 (33.7) |
| MR PBSCs | 192 (11.4) |
| MM/UR BM | 882 (52.4) |
| MM/UR PBSCs | 29 (1.7) |
| Cord blood | 13 (0.8) |
| T cell–depleted/CD34-selected | 70 (4.2) |
| CMV serostatus* | |
| D−/R− | 571 (34.2) |
| D+/R− | 252 (15.1) |
| D−/R+ | 366 (21.9) |
| D+/R+ | 483 (28.9) |
| CMV disease | 166 (9.9) |
| GVHD, acute grade higher than 1 | 1207 (77.2) |
| GVHD, clinically extensive | 696 (59.0) |
| Respiratory virus infection | 280 (16.7) |
| Delayed neutrophil engraftment | 973 (57.9) |
| Delayed lymphocyte engraftment | 1123 (66.8) |
| Delayed monocyte engraftment | 1162 (69.1) |
| Secondary neutropenia | 170 (10.1) |
| . | No. (%) . |
|---|---|
| Median recipient age, y (range) | 37 (0-68) |
| Male sex | 1013 (60.2) |
| Underlying diagnosis | |
| CML, chronic phase | 404 (24.0) |
| Hematologic malignancy, first remission | 166 (9.9) |
| Hematologic malignancy, other | 729 (43.3) |
| Other | 383 (22.8) |
| Donor and stem cell source | |
| MR BM | 566 (33.7) |
| MR PBSCs | 192 (11.4) |
| MM/UR BM | 882 (52.4) |
| MM/UR PBSCs | 29 (1.7) |
| Cord blood | 13 (0.8) |
| T cell–depleted/CD34-selected | 70 (4.2) |
| CMV serostatus* | |
| D−/R− | 571 (34.2) |
| D+/R− | 252 (15.1) |
| D−/R+ | 366 (21.9) |
| D+/R+ | 483 (28.9) |
| CMV disease | 166 (9.9) |
| GVHD, acute grade higher than 1 | 1207 (77.2) |
| GVHD, clinically extensive | 696 (59.0) |
| Respiratory virus infection | 280 (16.7) |
| Delayed neutrophil engraftment | 973 (57.9) |
| Delayed lymphocyte engraftment | 1123 (66.8) |
| Delayed monocyte engraftment | 1162 (69.1) |
| Secondary neutropenia | 170 (10.1) |
Only patients who received myeloablative conditioning regimens between January 1, 1993, and December 31, 1998, were included in the cohort. Cohort does not include patients who developed IA prior to HSC transplantation. Characteristics and outcome variables shown are those that were examined in risk factor models.
BM indicates bone marrow; PBSCs, peripheral blood stem cells; MM, mismatched; and UR, unrelated.
CMV serostatus was not available for 10 patient-donor pairs.
Conditioning regimens, GVHD prophylaxis, and supportive care for allograft recipients at FHCRC have been previously described.10-13 Standard care for prevention of candidiasis and CMV disease included fluconazole (400 mg/d) until day 75 after HSC transplantation5,6 and administration of ganciclovir based on monitoring for CMV pp65 antigenemia.14 During the years 1993 through 1995, several patients received ganciclovir prophylactically (at engraftment) as part of a randomized trial.15 Inpatients were housed in rooms equipped with high-efficiency particulate air (HEPA) filtration, but laminar airflow (LAF) was not used. Standard antimicrobials for treatment of fever in the setting of neutropenia included ceftazidime with addition of an aminoglycoside or a quinolone, and/or vancomycin when clinically indicated. Amphotericin B (0.5-1.0 mg/kg/d or equivalent doses of lipid formulations) was given to patients with unexplained fever that persisted beyond 96 hours.
Chest x-rays were routinely performed weekly or when clinically indicated, such as for evaluation of fever. Computed tomography (CT) scans were performed to evaluate abnormalities. Cultures of bronchoalveolar lavage (BAL) and tissue biopsy specimens and identification of filamentous fungi were performed according to standard protocols. Patients were treated for IA with amphotericin B deoxycholate (1-1.5 mg/kg/d) or equivalent doses of lipid formulations, except for fewer than 20 patients in 1998 who were treated with an investigational azole antifungal as part of a randomized protocol or as secondary therapy.
Definitions and statistical analyses
Only patients with IA that was documented as proven or probable according to standardized definitions16 were considered to be case patients. Briefly, proven disease required histopathologic or microbiologic documentation of disease from biopsied tissues, and infection was considered probable if the fungus was identified from culture of BAL when consistent signs and symptoms were present. The day of diagnosis of the invasive fungal infection was the day on which the first diagnostic test was performed. For patients whose diagnosis was obtained from postmortem examination, the day of death was considered to be the day of diagnosis. Patients who received their first HSCT during the same years were considered controls. Patients who had known aspergillosis diagnosed prior to HSC transplantation were excluded from the analysis.
The one-year cumulative incidence of invasive aspergillosis was calculated according to year of transplantation. Risk factors associated with aspergillosis after allogeneic HSC transplantation were identified in a multivariable Cox regression model. The end point was time to diagnosis of aspergillosis, with censoring at date of last follow-up, relapsed malignancy, second transplantation, or death. To identify specific risk factors for IA during the “early” and “late” periods after transplantation, we developed additional multivariable Cox regression models for early infection (diagnosed up to 40 days after transplantation) and late infection (diagnosed more than 40 days after transplantation). Forty days was chosen as a cutoff point to ensure that the early model reflected the immediate postengraftment period of neutropenia and to be consistent with previous analyses.2 Follow-up time was censored at 40 days for the early aspergillosis model and at 180 days for the late aspergillosis model. Additional models were constructed to evaluate the risks for infection diagnosed more than 180 days after transplantation and to evaluate the risks for infection between days 40 and 100. The latter model was designed to measure the impact of corticosteroids, as data on drug administration were most reliable prior to patients' discharge from Seattle, which usually occurs approximately 100 days after transplantation.
Candidate host variables included sex, age, underlying disease and remission status, and CMV serostatus of donor and recipient. To identify risks related to the transplantation, we evaluated conditioning regimen, stem cell source, and donor type. Composite variables for stem cell source (bone marrow or peripheral blood stem cells [PBSCs]) and donor type (unrelated, human leukocyte antigen [HLA]–matched related, or HLA-mismatched related) were entered into the model. Cord blood recipients were identified with an independent variable, without accounting for HLA matching. Transplantation with T cell–depleted or CD34-selected stem cells was included as an independent variable.
Neutropenia was included as a time-dependent covariate in all models. This factor contributed to the hazard estimate if the diagnosis of IA occurred prior to engraftment (defined as > 2 consecutive days with an absolute neutrophil count > 750) or after secondary neutropenia (absolute neutrophil count < 750 for 2 consecutive days after engraftment). To measure the effect of delayed reconstitution of monocytes and lymphocytes, time-dependent engraftment covariates were included in the late IA model. Engraftment was defined as at least 3 consecutive days with more than 300 monocytes per milliliter or more than 300 T lymphocytes per milliliter, respectively. Other time-dependent covariates included acute and chronic GVHD (graded independently according to published criteria17 18), CMV disease (CMV detected by direct fluorescent antibody [DFA] or cultured by shell vial or conventional culture from BAL or tissue), and infection with respiratory viruses. Infection with parainfluenza viruses, respiratory syncytial virus (RSV), and influenza viruses was defined by presence of signs and symptoms of either upper respiratory infection or pneumonia and identification of the virus with DFA staining, shell vial culture, or conventional culture of respiratory secretions. Only viral infections that occurred before the diagnosis of IA during the corresponding time period were considered potential risk factors for aspergillosis.
The highest daily dose of corticosteroids (prednisone and methylprednisolone; < 1.9 mg/kg/d, 2.0-2.9 mg/kg/d, > 3.0 mg/kg/d) was calculated and entered into the risk factor model for days 40 through 100 as a time-dependent variable. Receipt of corticosteroids were considered a potential risk factor for aspergillosis only if the drugs were received prior to the diagnosis of IA.
All candidate variables were entered into the multivariable model and sequentially eliminated in a stepwise backward fashion until all remaining variables were statistically significant. Survival after infection was estimated with Kaplan-Meier curves for all patients who had diagnosis established before death.19 Associations in 2 × 2 tables were analyzed with χ2 and Fisher exact tests, when applicable.20 Two-sided Ps of .05 or less were considered significant.
To compare the incidence and timing of IA between 1993 and 1998 with those during earlier years, data were abstracted from a previously defined cohort of patients with IA at our institution.2 In the earlier study, cases were identified and defined using similar methods.
Results
Incidence and timing of aspergillosis
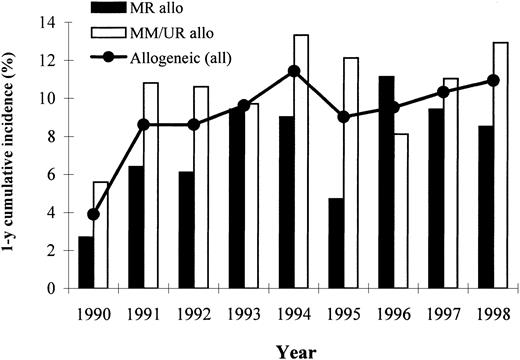
Between 1990 and 1998, the overall incidence of proven or probable IA increased in all allograft recipients (Figure1). Over this period, the annual incidence of IA was 10.5% among recipients of HLA-mismatched or unrelated (MM/UR) donor transplants and 7.3% among recipients of matched related (MR) donor transplants.
One-year cumulative incidence of proven or probable IA among allogeneic graft recipients through the 1990s.
Data for years 1990 through 1992 were abstracted from a previously published study.2 Diagnoses established after second transplantation, relapsed malignancy, or death are not included.
One-year cumulative incidence of proven or probable IA among allogeneic graft recipients through the 1990s.
Data for years 1990 through 1992 were abstracted from a previously published study.2 Diagnoses established after second transplantation, relapsed malignancy, or death are not included.
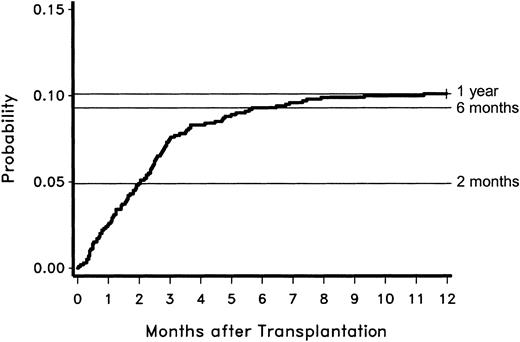
Between 1993 and 1998, 57 cases of IA (30% of the total) were diagnosed early (< 40 days) after HSC transplantation, and 99 cases (53%) were diagnosed between days 40 and 180. An additional 31 cases (17%) developed later than 6 months after transplantation. The probability of developing proven or probable IA according to time after transplantation is shown in Figure 2. Probability reached approximately 5% at 2 months, 9% at 6 months, and 10% at 1 year after transplantation. By years 3 and 5 after transplantation, the probability of IA increased minimally, to 11.1% and 11.4%, respectively (data not shown).
Probability of developing proven or probable IA according to time after transplantation for 187 case patients between 1993 and 1998.
Probability of developing proven or probable IA according to time after transplantation for 187 case patients between 1993 and 1998.
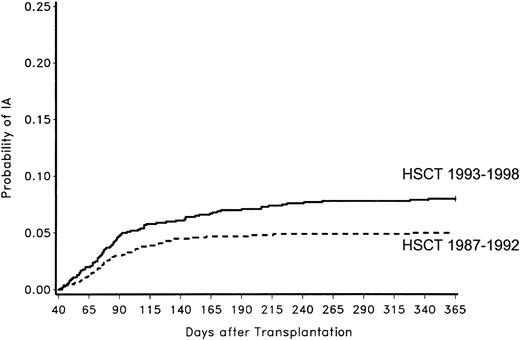
The timing of infection was compared with the timing of infection in the previously described cohort of patients who developed IA between January 1987 and June 1993.2 More patients in the later years (1993 through 1998) were diagnosed with IA later than 6 months after transplantation (31 of 187 vs 7 of 158;P < .001). This trend was accompanied by a trend toward decreased aspergillosis occurring before day 40 (57 of 187 vs 62 of 158; P = .09).
To determine whether the increased number of cases of postengraftment aspergillosis in the later cohort was simply due to a larger number of patients' being alive after recovery from neutropenia because of improved supportive care strategies, we calculated the probability of IA only among people alive at day 40 in both cohorts. The probability of IA during the initial 100 days after transplantation was significantly higher in the 1993-1998 cohort than in the 1987-1992 cohort (P = .05). The differential continued to increase by one year after transplantation (P = .001; Figure3).
Probability of developing proven or probable IA among patients alive at day 40 in 2 cohorts.
The first cohort underwent HSC transplantation between 1987 and 1992 and the second between 1993 and 1998 (overallP = .001).
Probability of developing proven or probable IA among patients alive at day 40 in 2 cohorts.
The first cohort underwent HSC transplantation between 1987 and 1992 and the second between 1993 and 1998 (overallP = .001).
Risk factors for aspergillosis
Risks for IA were identified among 1682 patients who received first allogeneic HSCTs at FHCRC between January 1, 1993, and December 31, 1998 (Table 2). Host variables that increased the risk for IA included age at transplantation and underlying disease. Type of transplant affected overall risk, with recipients of cord blood, HLA-mismatched or unrelated donor PBSCs, and T cell–depleted or CD34-selected stem cells having increased risk. Late complications associated with increased risk included neutropenia, acute and chronic GVHD, and viral infections. To further understand the impact of each variable, we evaluated risks according to infection that occurred early (≤ 40 days) and late (41-180 days) after transplantation.
Risk factors for proven or probable IA among case (n = 187) and control (n = 1495) patients who received allogeneic HSCTs at FHCRC, 1993-1998
| . | Controls, no. (%) . | Cases, no. (%) . | HR . | 95% CI . |
|---|---|---|---|---|
| Recipient-related factors | ||||
| Age, y | ||||
| Younger than 19 | 239 (16.0) | 23 (12.3) | 1.0 | — |
| 19-40 | 634 (42.4) | 67 (35.8) | 1.5 | NS |
| Older than 40 | 622 (41.6) | 97 (51.9) | 2.4 | 1.5-3.82-153 |
| Underlying disease | ||||
| CML, chronic phase | 367 (24.6) | 37 (19.8) | 1.0 | — |
| Hematologic malignancy, first remission | 151 (10.1) | 15 (8.0) | 1.1 | NS |
| Hematologic malignancy, other | 650 (43.5) | 79 (42.3) | 1.6 | 1.1-2.42-155 |
| Other* | 327 (21.9) | 56 (30.0) | 2.1 | 1.4-3.22-153 |
| Transplant-related factors (donor and stem cell source) | ||||
| MR BM | 509 (34.1) | 57 (30.5) | 1.0 | — |
| MR PBSCs | 175 (11.7) | 17 (9.1) | 0.7 | NS |
| MM/UR BM | 779 (52.1) | 103 (55.1) | 1.1 | NS |
| MM/UR PBSCs | 22 (1.5) | 7 (3.7) | 2.8 | 1.1-7.02-155 |
| Cord blood | 10 (0.7) | 3 (1.6) | 5.1 | 1.5-17.22-155 |
| T cell–depleted/CD34-selected | 54 (3.6) | 16 (8.6) | 2.2 | 1.2-4.12-155 |
| Transplant complications | ||||
| Neutropenia† | — | — | 3.0 | 2.0-4.62-153 |
| GVHD, acute†,‡ | ||||
| Grades 0-1 | — | — | 1.0 | |
| Grades 2-4 | 2.2 | 1.4-3.42-153 | ||
| Missing | 2.1 | NS | ||
| GVHD, chronic (clinically extensive)†,‡ | — | — | 2.2 | 1.3-3.72-155 |
| CMV disease† | — | — | 7.0 | 4.5-10.82-153 |
| Respiratory virus infection† | — | — | 2.1 | 1.4-3.12-153 |
| . | Controls, no. (%) . | Cases, no. (%) . | HR . | 95% CI . |
|---|---|---|---|---|
| Recipient-related factors | ||||
| Age, y | ||||
| Younger than 19 | 239 (16.0) | 23 (12.3) | 1.0 | — |
| 19-40 | 634 (42.4) | 67 (35.8) | 1.5 | NS |
| Older than 40 | 622 (41.6) | 97 (51.9) | 2.4 | 1.5-3.82-153 |
| Underlying disease | ||||
| CML, chronic phase | 367 (24.6) | 37 (19.8) | 1.0 | — |
| Hematologic malignancy, first remission | 151 (10.1) | 15 (8.0) | 1.1 | NS |
| Hematologic malignancy, other | 650 (43.5) | 79 (42.3) | 1.6 | 1.1-2.42-155 |
| Other* | 327 (21.9) | 56 (30.0) | 2.1 | 1.4-3.22-153 |
| Transplant-related factors (donor and stem cell source) | ||||
| MR BM | 509 (34.1) | 57 (30.5) | 1.0 | — |
| MR PBSCs | 175 (11.7) | 17 (9.1) | 0.7 | NS |
| MM/UR BM | 779 (52.1) | 103 (55.1) | 1.1 | NS |
| MM/UR PBSCs | 22 (1.5) | 7 (3.7) | 2.8 | 1.1-7.02-155 |
| Cord blood | 10 (0.7) | 3 (1.6) | 5.1 | 1.5-17.22-155 |
| T cell–depleted/CD34-selected | 54 (3.6) | 16 (8.6) | 2.2 | 1.2-4.12-155 |
| Transplant complications | ||||
| Neutropenia† | — | — | 3.0 | 2.0-4.62-153 |
| GVHD, acute†,‡ | ||||
| Grades 0-1 | — | — | 1.0 | |
| Grades 2-4 | 2.2 | 1.4-3.42-153 | ||
| Missing | 2.1 | NS | ||
| GVHD, chronic (clinically extensive)†,‡ | — | — | 2.2 | 1.3-3.72-155 |
| CMV disease† | — | — | 7.0 | 4.5-10.82-153 |
| Respiratory virus infection† | — | — | 2.1 | 1.4-3.12-153 |
Hazard ratios (HRs) and 95% confidence intervals (CIs) are shown for all significant variables.
—indicates data not applicable; NS, not significant in the multivariable model.
The most common “other” diagnoses are aplastic anemia, myelodysplastic syndrome, and multiple myeloma.
Factors entered into the model as time-dependent covariates.
The GVHD variable “missing” signifies patients who did not have data entered into the computerized system (n = 118). Acute and chronic GVHD were independently graded, as previously described.17 18
P ≤ .001.
P ≤ .05.
Risk factors for early IA (up to 40 days after transplantation)
Results of multivariable risk factor models for IA during each time period are shown in Table 3. Because risks for IA in the overall model were highest in people with “other” diagnoses, models for early and late IA included separate disease categories for the most frequent “other” diagnoses—myelodysplastic syndrome (n = 209), multiple myeloma (n = 64), and aplastic anemia (n = 50). In the multivariable model, aplastic anemia and myelodysplastic syndrome were associated with increased risks for early IA (hazard ratio [HR] = 8.3; 95% CI, 1.4-50.6; P = .02; and HR = 6.0; 95% CI, 1.6-22.4; P = .008, respectively). Multiple myeloma was associated with a trend toward increased risk for early IA (HR = 4.3; 95% CI, 0.7-26.7; P = .12).
Risk factors for early IA (up to 40 days after transplantation) and late IA (days 41-180 after transplantation)
| . | Early IA (n = 57) . | Late IA (n = 99) . | ||||
|---|---|---|---|---|---|---|
| Cases, no. (%) . | HR . | 95% CI . | Cases, no. (%) . | HR . | 95% CI . | |
| Recipient-related factors | ||||||
| Age, y | ||||||
| Younger than 19 | 5 (8.8) | 1.0 | — | 12 (12.1) | — | — |
| 19-40 | 21 (36.8) | 3.8 | 1.3-11.23-155 | 34 (34.3) | NS | NS |
| Older than 40 | 31 (54.4) | 5.9 | 2.0-17.43-154 | 53 (53.5) | — | — |
| Underlying disease3-150 | ||||||
| CML, chronic phase | 3 (5.3) | 1.0 | — | 24 (24.2) | 1.0 | — |
| Hematologic malignancy, first remission | 5 (8.8) | 4.4 | 1.0-18.83-155 | 6 (6.1) | — | NS |
| Hematologic malignancy, other | 31 (54.4) | 6.9 | 2.1-23.13-155 | 37 (37.4) | — | NS |
| Aplastic anemia | 2 (3.5) | 8.3 | 1.4-50.63-155 | 2 (2.0) | — | NS |
| Myelodysplastic syndrome | 9 (15.8) | 6.0 | 1.6-22.43-155 | 13 (13.1) | — | NS |
| Multiple myeloma | 2 (3.5) | — | NS | 13 (13.1) | 4.5 | 2.3-9.13-154 |
| CMV serostatus3-151 | ||||||
| D−/R− | 14 (24.6) | — | — | 20 (20.2) | 1.0 | — |
| D+/R− | 5 (8.8) | NS | NS | 17 (17.2) | 2.0 | 1.0-3.73-155 |
| D−/R+ | 17 (29.8) | — | — | 30 (30.3) | 2.0 | 1.1-3.73-155 |
| D+/R+ | 21 (36.8) | — | — | 32 (32.3) | — | NS |
| Transplant-related factors (donor and stem cell source) | ||||||
| MR BM | 17 (29.8) | 1.0 | — | 31 (31.3) | — | — |
| MR PBSCs | 2 (3.5) | 0.2 | 0.05-0.93-155 | 12 (12.1) | — | — |
| MM/UR BM | 32 (56.1) | — | NS | 53 (53.5) | NS | NS |
| MM/UR PBSCs | 3 (5.3) | — | NS | 3 (3.0) | — | — |
| Cord blood | 3 (5.3) | 13.5 | 3.3-55.53-154 | 0 | — | — |
| T cell–depleted/CD34-selected | 6 (10.5) | — | NS | 9 (9.1) | 3.4 | 1.7-7.03-154 |
| Transplant complications | ||||||
| Neutropenia3-152 | — | — | — | — | 2.6 | 1.4-4.83-155 |
| Lymphopenia3-152 | — | — | — | — | 2.0 | 1.1-3.83-155 |
| GVHD, acute3-152,3-153 | ||||||
| Grades 0-1 | — | — | — | — | 1.0 | — |
| Grades 2-4 | — | — | — | — | 10.6 | 2.6-43.43-154 |
| Missing | — | — | — | — | 10.6 | 2.2-52.13-155 |
| GVHD, chronic (clinically extensive)3-152,3-153 | — | — | — | — | — | NS |
| CMV disease3-152 | — | 26.3 | 9.6-72.03-154 | — | 10.2 | 5.4-19.53-154 |
| Respiratory virus infection3-152 | — | — | NS | — | 2.1 | 1.1-3.83-155 |
| . | Early IA (n = 57) . | Late IA (n = 99) . | ||||
|---|---|---|---|---|---|---|
| Cases, no. (%) . | HR . | 95% CI . | Cases, no. (%) . | HR . | 95% CI . | |
| Recipient-related factors | ||||||
| Age, y | ||||||
| Younger than 19 | 5 (8.8) | 1.0 | — | 12 (12.1) | — | — |
| 19-40 | 21 (36.8) | 3.8 | 1.3-11.23-155 | 34 (34.3) | NS | NS |
| Older than 40 | 31 (54.4) | 5.9 | 2.0-17.43-154 | 53 (53.5) | — | — |
| Underlying disease3-150 | ||||||
| CML, chronic phase | 3 (5.3) | 1.0 | — | 24 (24.2) | 1.0 | — |
| Hematologic malignancy, first remission | 5 (8.8) | 4.4 | 1.0-18.83-155 | 6 (6.1) | — | NS |
| Hematologic malignancy, other | 31 (54.4) | 6.9 | 2.1-23.13-155 | 37 (37.4) | — | NS |
| Aplastic anemia | 2 (3.5) | 8.3 | 1.4-50.63-155 | 2 (2.0) | — | NS |
| Myelodysplastic syndrome | 9 (15.8) | 6.0 | 1.6-22.43-155 | 13 (13.1) | — | NS |
| Multiple myeloma | 2 (3.5) | — | NS | 13 (13.1) | 4.5 | 2.3-9.13-154 |
| CMV serostatus3-151 | ||||||
| D−/R− | 14 (24.6) | — | — | 20 (20.2) | 1.0 | — |
| D+/R− | 5 (8.8) | NS | NS | 17 (17.2) | 2.0 | 1.0-3.73-155 |
| D−/R+ | 17 (29.8) | — | — | 30 (30.3) | 2.0 | 1.1-3.73-155 |
| D+/R+ | 21 (36.8) | — | — | 32 (32.3) | — | NS |
| Transplant-related factors (donor and stem cell source) | ||||||
| MR BM | 17 (29.8) | 1.0 | — | 31 (31.3) | — | — |
| MR PBSCs | 2 (3.5) | 0.2 | 0.05-0.93-155 | 12 (12.1) | — | — |
| MM/UR BM | 32 (56.1) | — | NS | 53 (53.5) | NS | NS |
| MM/UR PBSCs | 3 (5.3) | — | NS | 3 (3.0) | — | — |
| Cord blood | 3 (5.3) | 13.5 | 3.3-55.53-154 | 0 | — | — |
| T cell–depleted/CD34-selected | 6 (10.5) | — | NS | 9 (9.1) | 3.4 | 1.7-7.03-154 |
| Transplant complications | ||||||
| Neutropenia3-152 | — | — | — | — | 2.6 | 1.4-4.83-155 |
| Lymphopenia3-152 | — | — | — | — | 2.0 | 1.1-3.83-155 |
| GVHD, acute3-152,3-153 | ||||||
| Grades 0-1 | — | — | — | — | 1.0 | — |
| Grades 2-4 | — | — | — | — | 10.6 | 2.6-43.43-154 |
| Missing | — | — | — | — | 10.6 | 2.2-52.13-155 |
| GVHD, chronic (clinically extensive)3-152,3-153 | — | — | — | — | — | NS |
| CMV disease3-152 | — | 26.3 | 9.6-72.03-154 | — | 10.2 | 5.4-19.53-154 |
| Respiratory virus infection3-152 | — | — | NS | — | 2.1 | 1.1-3.83-155 |
Calculated on the basis of 1625 evaluable control patients and 57 cases during the early period and 1526 evaluable control patients and 99 cases during the late period. Hazard ratios (HRs) and 95% confidence intervals (CIs) are shown for all significant variables. —indicates data not applicable; NS indicates not significant in the multivariable model.
Only underlying diseases associated with significant risks are shown.
CMV serostatus was not available for 10 patient-donor pairs.
Factors entered into the model as time-dependent covariates.
The GVHD variable “missing” signifies patients who did not have data entered into the computerized system (n = 113). Acute and chronic GVHD were independently graded, as previously described.17 18 GVHD variables were not entered into the model for early IA.
P ≤ .05.
P ≤ .001.
Stem cell source affected the risk for IA during the early time period; compared with marrow transplantation from an HLA-matched related donor, PBSC transplantation from an HLA-matched related donor was associated with a trend toward lower risk of IA early after transplantation. Transplantation with T cell–depleted or CD34-selected stem cell products was associated with a trend toward increased risk for early IA (HR = 2.4; 95% CI, 0.9-6.8; P = .09). Three of 13 cord blood recipients developed IA early after transplantation, corresponding with a 13.5-fold increased hazard ratio in the multivariable model.
These factors were significantly associated with early IA, independent of neutropenia, which was entered into the model as a time-dependent covariate. Neutropenia was removed from the model at the last stage of the backward selection, with a P of .09. We hypothesized that the strong relationship between stem cell source and the day of neutrophil engraftment interfered with our ability to measure risks associated with engraftment alone. We therefore repeated the model without including variables for stem cell source. In this repeat analysis, delayed neutrophil engraftment was associated with an increased risk for early IA (HR = 3.3; 95% CI, 1.4-8.0;P = .009), without altering the significance of any other risks. These results indicate that the risk of early IA attributable to stem cell source is at least in part associated with time to neutrophil engraftment.
Patients who developed CMV disease during the early time period had an increased risk for subsequent early IA (n = 5; HR = 26.3). Factors entered into the multivariable models that were not associated with increased risk for early IA include patient's sex, conditioning regimen, and donor/recipient (D/R) CMV serostatus (data not shown).
Risk factors for late IA (days 41-180 after transplantation)
We next analyzed risk factors for the 99 cases of IA that were diagnosed between days 41 and 180 after transplantation. Transplantation with T cell–depleted or CD34-selected stem cell products was associated with an increased risk for late IA (HR = 3.4), independent of other postengraftment complications and engraftment parameters. The only underlying disease that was associated with an increased risk for late IA was multiple myeloma, with a hazard ratio of 4.5 (Table 3). Donor and recipient CMV serostatus affected risks for late IA (Table 3). There was an also a trend toward increased risk for late IA in D+/R+ patients (HR = 1.6; 95% CI, 0.9-2.9;P = .09). Delayed engraftment of T lymphocytes and neutropenia were both associated with increased risks for late IA (HR = 2.0; 95% CI, 1.4-3.8; P = .03; and HR = 2.6; 95% CI, 1.4-4.8; P = .003, respectively). Risks were not affected by delayed engraftment of monocytes (P > .05 in the univariate model).
Patients who developed CMV disease after day 40 had an increased risk of subsequent IA during the day 41-180 time period (n = 14; HR = 10.2). The median number of days between diagnosis of CMV and IA was 5 (range, 0-49 days). Patients with respiratory virus infections after day 40 also had a 2.1-fold increased risk of subsequent IA. These risks were estimated from a total of 13 people who developed respiratory virus infections prior to (n = 11) or on the same day as (n = 2) diagnosis of IA. The predominant respiratory virus associated with increased risk for IA was parainfluenza 3 (n = 9), followed by RSV (n = 2). One additional patient had infection with both parainfluenza 3 and RSV. The median number of days between respiratory virus infection and IA was 9 (range, 0-100 days). Repeating the analyses after removing patients who had concurrent diagnoses did not change the significance of the association (data not shown).
Impact of corticosteroids: risks between days 41 and 100 after transplantation
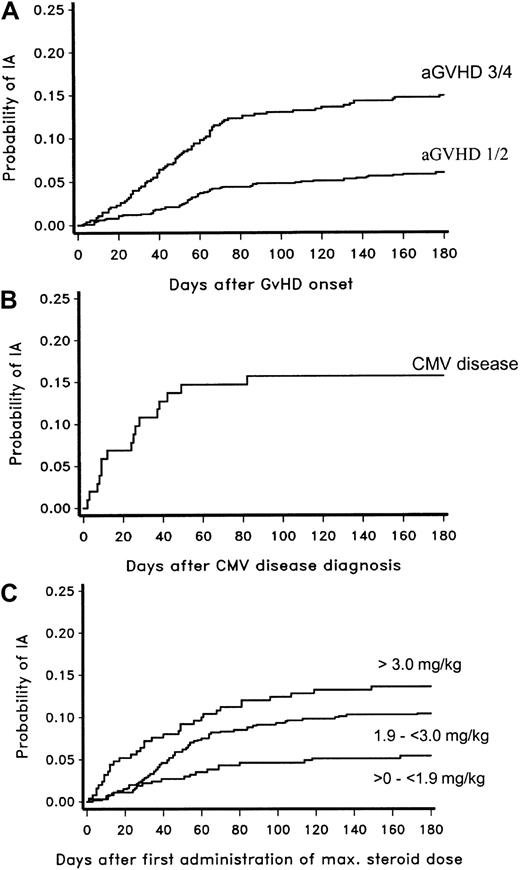
The impact of corticosteroids was assessed in a separate risk factor model that censored for follow-up at 100 days. This was done to ensure accuracy in drug administration data, which may be less reliable after discharge from Seattle. The previously noted impact of underlying disease, GVHD, and lymphopenia were negated in the model that included corticosteroids as a variable. Older age, transplantation with T cell–depleted or CD34-selected products, recipient and donor CMV serostatus, neutropenia, and viral infections remained associated with increased risk for IA, independent of receipt of corticosteroids (Table 4). Figure4 illustrates the probabilities of late IA after each of the most strongly associated risk factors—acute GVHD, CMV disease, and receipt of corticosteroids.
Risk factors for IA between days 40 and 100 after transplantation (analysis of corticosteroid therapy)
| . | Controls (n = 1552), no. (%) . | Cases (n = 73), no. (%) . | HR . | 95% CI . |
|---|---|---|---|---|
| Recipient-related factors | ||||
| Age, y | ||||
| Younger than 19 | 249 (16.0) | 8 (11.0) | 1.0 | — |
| 19-40 | 659 (42.5) | 21 (28.8) | — | NS |
| Older than 40 | 644 (41.5) | 44 (60.3) | 3.3 | 1.5-7.1‡ |
| CMV serostatus4-150 | ||||
| D−/R− | 542 (35.2) | 15 (20.6) | 1.0 | — |
| D+/R− | 234 (15.2) | 13 (17.8) | 2.2 | 1.0-4.6‡ |
| D−/R+ | 330 (21.4) | 19 (26.0) | — | NS |
| D+/R+ | 436 (28.3) | 26 (35.6) | — | NS |
| Transplant-related factors (stem cells) cell-depleted/CD34-selected | 56 (3.6) | 8 (11.0) | 2.8 | 1.2-6.1‡ |
| Transplant complications | ||||
| Neutropenia4-151 | — | — | 2.3 | 1.1-5.0‡ |
| CMV disease4-151 | — | — | 15.4 | 7.5-31.74-153 |
| Respiratory virus infection4-151 | — | — | 2.8 | 1.3-5.7‡ |
| Corticosteroids, maximum dose, mg/kg/d4-151 | ||||
| 0 | — | — | 1.0 | — |
| Less than 1.9 | — | — | — | NS |
| 2.0-3.0 | — | — | 8.0 | 2.9-22.54-153 |
| More than 3.0 | — | — | 15.4 | 5.2-45.74-153 |
| . | Controls (n = 1552), no. (%) . | Cases (n = 73), no. (%) . | HR . | 95% CI . |
|---|---|---|---|---|
| Recipient-related factors | ||||
| Age, y | ||||
| Younger than 19 | 249 (16.0) | 8 (11.0) | 1.0 | — |
| 19-40 | 659 (42.5) | 21 (28.8) | — | NS |
| Older than 40 | 644 (41.5) | 44 (60.3) | 3.3 | 1.5-7.1‡ |
| CMV serostatus4-150 | ||||
| D−/R− | 542 (35.2) | 15 (20.6) | 1.0 | — |
| D+/R− | 234 (15.2) | 13 (17.8) | 2.2 | 1.0-4.6‡ |
| D−/R+ | 330 (21.4) | 19 (26.0) | — | NS |
| D+/R+ | 436 (28.3) | 26 (35.6) | — | NS |
| Transplant-related factors (stem cells) cell-depleted/CD34-selected | 56 (3.6) | 8 (11.0) | 2.8 | 1.2-6.1‡ |
| Transplant complications | ||||
| Neutropenia4-151 | — | — | 2.3 | 1.1-5.0‡ |
| CMV disease4-151 | — | — | 15.4 | 7.5-31.74-153 |
| Respiratory virus infection4-151 | — | — | 2.8 | 1.3-5.7‡ |
| Corticosteroids, maximum dose, mg/kg/d4-151 | ||||
| 0 | — | — | 1.0 | — |
| Less than 1.9 | — | — | — | NS |
| 2.0-3.0 | — | — | 8.0 | 2.9-22.54-153 |
| More than 3.0 | — | — | 15.4 | 5.2-45.74-153 |
Calculated on the basis of 1552 evaluable control patients and 73 cases. Hazard ratios (HRs) and 95% confidence intervals (CIs) are shown for all significant variables.
—indicates data not applicable; NS, not significant in the multivariable model.
Either donor or recipient serostatus was not available for 10 patients.
Factors entered into the model as time-dependent covariates.
P ≤ .05.
P ≤ .001.
Probability of developing proven or probable IA late after onset of acute GVHD, diagnosis of CMV disease, or receipt of corticosteroids.
Panel A shows probabilities for patients with acute GVHD (aGVHD) grade 1 or 2 and those with aGVHD grade 3 or 4. Panel B shows CMV disease, and panel C shows probability according to dose of corticosteroids administered.
Probability of developing proven or probable IA late after onset of acute GVHD, diagnosis of CMV disease, or receipt of corticosteroids.
Panel A shows probabilities for patients with acute GVHD (aGVHD) grade 1 or 2 and those with aGVHD grade 3 or 4. Panel B shows CMV disease, and panel C shows probability according to dose of corticosteroids administered.
Risk factors for IA more than 6 months after transplantation
To evaluate the risks for IA in the patients who developed infection later than 6 months after transplantation (n = 31), an additional multivariable model was applied, using the same variables as the overall models. During this very late time period, neutropenia and clinically extensive chronic GVHD were associated with increased risks (HR = 6.7; 95% CI, 3.0-15.3; and HR 7.1; 95% CI, 2.1-23.8, respectively). In addition, receipt of unrelated or HLA-mismatched PBSCs was associated with increased risks compared with receipt of HLA-matched related BM (HR = 9.4; 95% CI, 1.2-75.5), and CMV disease was associated with an increased risk of subsequent IA (HR = 6.3; 95% CI, 2.1-18.9).
Outcomes
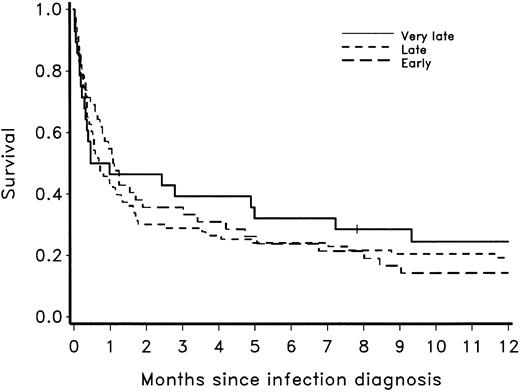
The Kaplan-Meier probability of survival one year after aspergillosis that developed during each time period is shown in Figure5. Survival in each group approximated 30% after 6 months and 20% after 1 year.
Probability of survival one year after diagnosis of proven or probable IA early, late, and very late after receipt of HSCT.
Probability of survival one year after diagnosis of proven or probable IA early, late, and very late after receipt of HSCT.
Discussion
Recent reports have indicated that the incidence of aspergillosis has increased in HSCT recipients, particularly after engraftment.2,3,21 22 The results of this study corroborate these observations and suggest that aspergillosis also occurs very late after HSC transplantation. Risk factor analysis among the largest cohort of allogeneic HSCT recipients with IA described to date indicates that the shift to late postengraftment aspergillosis is associated not only with neutropenia, GVHD, and corticosteroid therapy, but also with lymphopenia and viral infections that occur late after transplantation.
Several institutions have described a trend to late-onset IA, with reported median dates of diagnoses ranging from 48 to 136 days after transplantation.2,22-27 By comparing 2 cohorts of HSCT recipients in our institution, we have documented the trend from pre-engraftment to postengraftment infection, with a striking number of relapse-free patients developing infection more than 6 months after transplantation. Factors that influence the shift to late postengraftment IA may be multiple and may include host and transplantation variables that result in an increase in the number of patients who are alive with severe immune suppression late after transplantation as well as changes in reporting methods. The diagnostic tests and the methods used to identify cases of IA were similar in this study and our previous study2; however, it is possible that the increased number of documented cases late after transplantation in recent years may in part be influenced by the quality of long-term follow-up data. The finding that the probability of IA was higher by day 100, before patients' discharge from Seattle, suggests that the increase in postengraftment infection cannot be entirely explained by long-term follow-up reporting bias.
Host factors shown to be associated with the risk of IA include age and underlying disease. As in previous studies, our data document increased risks for infection in older patients2,21 and demonstrate a relative protection against IA in patients with CML in chronic phase.2 Our results further demonstrate additional high risks for early IA among patients with aplastic anemia, independent of day of engraftment, and high risks for late IA among patients with multiple myeloma, independent of GVHD. High transplant-related mortality among patients who receive allografts for treatment of multiple myeloma was previously described.28The specific variables underlying these risks remain unknown but may include pretransplantation immune suppression and organ dysfunction.
The shift from early to late IA also appears to have been affected by the use of different sources of stem cells. PBSC transplantation from an HLA-matched related donor was associated with protection against early IA, relative to bone marrow transplantation. This is consistent with recent studies suggesting that PBSC recipients reconstitute platelets, neutrophils, CD4+ T lymphocytes, and monocytes more rapidly than marrow recipients.29 30 In contrast, cord blood recipients were at particularly high risk for aspergillosis early after transplantation, which is most likely caused by delayed reconstitution of neutrophil and cellular immunity.
Neutrophil dysfunction in the setting of GVHD and corticosteroid administration has been largely assumed to be the primary factor increasing the risks for late infection.31 Our studies indicate that lymphopenia may also function as a risk factor during the late posttransplantation periods. Whether this factor presents an independent risk or serves as a marker for other immunologic defects associated with corticosteroid exposure is unclear. However, a protective role for T cells is supported by increased risks associated with T-cell depletion or CD34 selection and by the results of animal models. In murine models, protective immunity was associated with the activation of CD4+ TH1 cells producing interferon (IFN)–γ or with macrophage production of interleukin (IL)–12. In contrast, the production of IL-4 and IL-10 by CD4+ TH2 cells was associated with disease progression.32,33 Results of other animal studies suggest that T cells may mediate defense by up-regulating conidial killing by macrophages and hyphal killing by neutrophils.34 Further studies will be necessary to determine whether T-cell immunity toAspergillus species can be augmented in order to treat or prevent IA.
Recipients of PBSC transplants from an HLA-mismatched or unrelated donor had a higher risk of IA very late after transplantation, although the small number of patients in this group (n = 29) limits our ability to draw firm conclusions regarding the level of risk. Leukocyte engraftment occurs earlier in these patients than in those who receive BM,35-37 but the relative severity of GVHD remains to be defined. Although several reports have suggested increased rates of rapid-onset acute GVHD with UR PBSC transplantation compared with UR BM transplantation,36,37 results of one recent study suggest equivalent probabilities of acute GVHD regardless of stem cell source.35 Our data suggest that the increased risk is likely to be associated with corticosteroid therapy for GVHD.
Supportive care measures may affect the incidence and onset of IA, as the adoption of effective prevention strategies for CMV disease and candidiasis at FHCRC in the early 1990s coincided with the emergence of IA late after transplantation. An increase in the proportion of HSCT recipients alive after neutrophil engraftment could not entirely explain this increase, as the probability of late IA was higher in the most recent years when measured only among patients who survived the neutropenic period. Although we cannot measure the impact of laminar airflow isolation, which was discontinued between 1993 and 1994, it is notable that early IA did not increase in the later cohort compared with the previous cohort of HSCT recipients.
CMV disease was associated with the subsequent development of IA in all time periods examined. An association between CMV disease and fungal infections has been noted, particularly after solid-organ transplantation.38,39 In HSCT recipients, previous studies noted associations between CMV disease and candidiasis40and between patient CMV+ serostatus and non-Candida fungal infections.41 A more recent study demonstrated increased risk for IA among patients who developed CMV infection (antigenemia) or disease, but these investigators attributed the increased risk to corticosteroids.22 In this study, CMV disease was associated with particularly high risks for subsequent IA independent of corticosteroid administration, neutropenia, and T-cell engraftment.
Mechanisms to explain the associations between CMV seropositivity (and disease) and fungal infections are unknown. Neutropenia caused by treatment with ganciclovir is unlikely to be the sole explanation, since risks appear to be independent of secondary neutropenia and persist beyond the typical period of preemptive therapy (100 days). It is possible that CMV disease does not introduce an independent risk, but rather appears as a marker for a specific immunologic defect that was not adequately controlled for in the multivariable model. Other potential mechanisms include the immune-modulating effects of the virus itself: CMV can impair multiple antimicrobial effector mechanisms, including neutrophil activity and macrophage respiratory burst.42 43
Results of recent studies that emphasized poor transplant outcomes associated with donor or recipient CMV seropositivity provide compelling evidence for direct effects of the virus. In one study, higher transplant-related mortality (TRM) was observed in CMV-seropositive recipients of T cell–depleted grafts than in CMV-seronegative recipients.44 Ganciclovir-associated neutropenia could not entirely explain the association with CMV seropositivity, but CMV-seropositive patients had more severe GVHD. More recently, we reported that D+/R− recipients of non–T cell–depleted stem cell transplants had higher TRM than did D−/R− control patients.45 Mortality was associated predominantly with bacterial and fungal infections and was independent of ganciclovir-induced neutropenia in multivariable models. Results of the multiple risk factor analyses presented here are consistent with these earlier observations. Prospective studies will be necessary to define specific mechanisms underlying these associations.
To the best of our knowledge, a direct association between respiratory virus infections and aspergillosis in HSCT recipients has not been previously demonstrated. We reported that patients who developed upper or lower respiratory tract infection with parainfluenza 3 virus have increased mortality in multivariable models, but the cause was not defined.46 Mechanisms of increased risk may be related to direct effects on pulmonary phagocyte function, since at least one previous study documented that respiratory viruses can diminish microbicidal activity of murine alveolar macrophages.47
Overall outcome in patients with IA was equivalent and poor, regardless of the time during which infection developed. These findings are consistent with other reports of 30% survival at 3 months after infection in HSCT recipients.48 Identification of patient and therapeutic determinants of outcome awaits future studies.
Although we have reduced neutropenia-related aspergillosis during the past decade, the increase in late aspergillosis attests to the importance of the nonneutropenic immunosuppressed state in the pathogenesis of this disease. The results of this study suggest that changes in host, transplantation, and supportive care variables have had a combinatorial impact on the epidemiology of aspergillosis during the past decade. Further efforts are necessary to decrease the burden of late, nonnosocomial infections in allogeneic HSCT recipients. The results of the present study can assist these efforts by identifying the population of allograft recipients that might benefit most from targeted prevention strategies.
Prepublished online as Blood First Edition Paper, August 22, 2002; DOI 10.1182/blood-2002-05-1496.
Supported in part by grants from the National Institutes of Health (K08-A1571, CA-18029, CA 15704) and Merck.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Kieren A. Marr, Program in Infectious Diseases, Fred Hutchinson Cancer Research Center, 1100 Fairview Ave N, D3-100, Seattle, WA 98109; e-mail:kmarr@fhcrc.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal