We demonstrated that Flk-1+ cells derived from mouse embryonic stem (ES) cells can differentiate into both endothelial cells (ECs) and mural cells (MCs) to suffice as vascular progenitor cells (VPCs). In the present study, we investigated the importance of the stage of ES cell differentiation on effective participation in adult neovascularization. We obtained Flk-1+LacZ-expressing undifferentiated VPCs. Additional culture of these VPCs with vascular endothelial growth factor (VEGF) resulted in a mixture of ECs and MCs (differentiated VPCs). We injected VPCs subcutaneously into tumor-bearing mice. Five days after the injection, whereas undifferentiated VPCs were often detected as nonvascular cells, differentiated VPCs were more specifically incorporated into developing vasculature mainly as ECs. VPC-derived MCs were also detected in vascular walls. Furthermore, transplantation of differentiated VPCs augmented tumor blood flow in nude mice. These results indicate that a specific vascular contribution in adult neovascularization can be achieved by selective transplantation of ES cell–derived VPCs in appropriate differentiation stages, which should be the basis for vascular regeneration schemes.
Introduction
Embryonic stem (ES) cells with totipotency and self-renewal are now highlighted as promising sources for regeneration medicine. Recently we demonstrated that ES cell-derived Flk-1+ cells can differentiate into both endothelial cells (ECs) and mural cells (MCs; pericytes and vascular smooth muscle cells) and reproduce the vascular organization process.1 Vascular endothelial growth factor (VEGF) promotes EC differentiation from vascular progenitor cells (VPCs). Vascular cells derived from Flk-1+ cells can organize vessel-like structures in 3-dimensional culture. ES cell-derived Flk-1+ cells can thus serve as VPCs.
To date, substantial trials on vascular regeneration using endothelial precursor/progenitor cells derived from somatic cells have been reported.2-4 However, precise characterization of the transplanted cells or comparison of the effectiveness of cell differentiation stages to generate blood vessels has been scarce. We have established an in vitro vascular differentiation system using VPCs that can obtain ES cell–derived vascular cells at different stages of differentiation with homogeneity and in large quantities. Thus, in the present study, we examined the impact of differentiation stage differences of donor Flk-1+ ES cells in transplantation on adult neoangiogenesis, to explore the potential of Flk-1+VPCs for vascular generation therapy.
Study design
Cell culture and sorting
Maintenance of CCE5 ES cells (gift from M. J. Evans, Cambridge, United Kingdom) was as described previously.6 To induce Flk-1+ cells, ES cells were cultured on type IV collagen–coated dishes as reported previously.6 Flk-1+VE-cadherin−E-cadherin− cells were sorted by fluorescence-activated cell sorting (FACSVantage; Becton Dickinson, Bedford, MA) as described.6,7 After 3 days of incubation on type IV collagen-coated dishes with 50 ng/mL VEGF (human VEGF165; R & D Systems, Minneapolis, MN) in 10% fetal calf serum (FCS), cultured cells were harvested and further resorted by FACS. For serum-free culture, Flk-1+ cells were incubated in SFO3 (Sanko Junyaku, Chiba, Japan) with 10 ng/mL platelet-derived growth factor-BB (PDGF-BB; Gibco BRL, Grand Island, NY) as described.1 For detection of circulating LacZ+ cells in peripheral blood by flow cytometry, we used FluoReporter LacZ flow cytometry kits (Molecular Probes, Eugene, OR).
Tumor transplantation and ES cell injection
Six- to 8-week-old nude (nu/nu) mice (SLC, Shizuoka, Japan) underwent subcutaneous transplantation of 1 × 106 C6 rat glioblastoma cells, which secrete large amounts of VEGF, in 0.1 mL phosphate-buffered saline (PBS) on right and left flanks as reported previously.8 ES cells expressing LacZ gene (CCE/nLacZ) were generated as previously reported.1 Seven days after tumor transplantation, C6 cells produced small tumors in both sides of the flank. We injected ES cell–derived VPCs in 0.1 mL PBS subcutaneously at 5 sites around the left tumor. Control (PBS only, right) and VPC-transplanted (left) tumors were excised 5 days after injection and sectioned into 50 blocks for whole-mount LacZ staining.
LDPI analysis of the tumor blood flow
We measured the ratios of VPCs transplanted (left) to control (right) tumor blood flow using a laser Doppler perfusion image (LDPI) analyzer (Moor Instruments, Devon, United Kingdom) 5 days after VPC transplantation.
Results and discussion
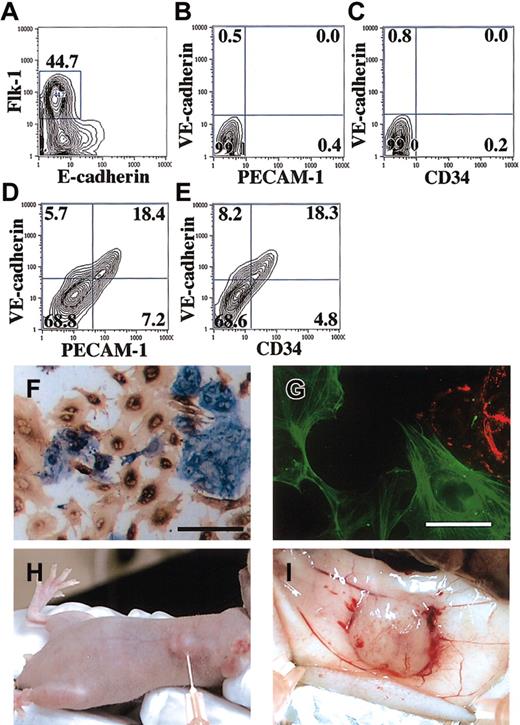
Characterization of implanted ES cell–derived VPCs
Sorted Flk-1+E-cadherin− cells did not express other EC (VE-cadherin, platelet-endothelial cell adhesion molecule 1 [PECAM-1], or CD34; Figure 1A-C) or MC (smooth muscle actin [SMA] or platelet-derived growth factor β [PDGF-β] receptor) markers (data not shown). We termed these cells “undifferentiated VPCs.” After an additional 3 days of culture with 10% FCS and 50 ng/mL VEGF165, Flk-1+ cells differentiated into mixtures of ECs and MCs. The cells that retained Flk-1 expression (about 30%) became also positive for VE-cadherin, PECAM-1, and CD34, indicating the differentiation into ECs (Figure 1D-E). The cells that lost Flk-1 expression (about 70%) were negative for EC markers, but positive for SMA (Figure 1F-G) and other markers of differentiated vascular smooth muscle cells (smooth muscle myosin heavy chain, calponin, and SM22α; data not shown). These cell mixtures were designated “differentiated VPCs.” We also sorted out a VE-cadherin+ fraction of differentiated VPCs by FACS. Three-day treatment of undifferentiated VPCs with PDGF-BB resulted in selective induction of SMA+ MCs, which were negative for Flk-1, VE-cadherin, and PECAM-1 (data not shown) in serum-free conditions (PDGF-BB–treated VPCs). Undifferentiated VPCs, differentiated VPCs (1 × 106 cells), VE-cadherin+ fraction of differentiated VPCs (0.3 × 106 cells), or PDGF-BB–treated VPCs (0.7 × 106 cells) were implanted (Figure 1H-I) into nude mice. We also injected 0.5 to 1.0 × 106 undifferentiated and differentiated VPCs in PBS into the tail vein.
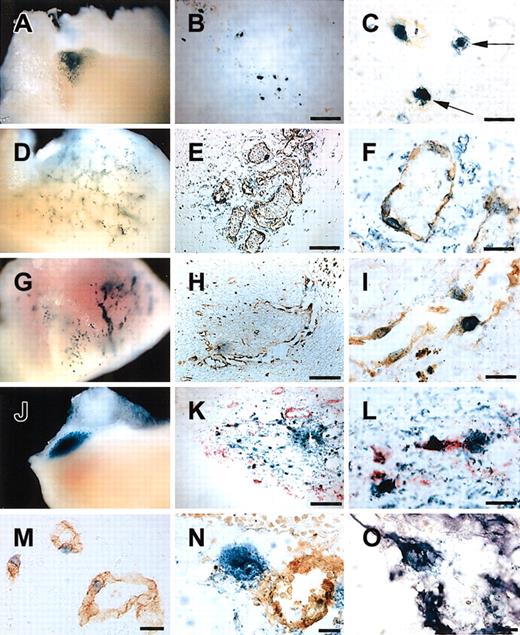
Contribution of VPCs to the vascular component in tumor neoangiogenesis
Five days after subcutaneous injection, differentiated VPCs were demonstrated to form tubelike structures (Figure2D), whereas undifferentiated VPCs mainly formed cell aggregates with little vascular stretch (Figure 2A). In undifferentiated VPC-injected tumors, many LacZ+ cells were negative for PECAM-1 (Figure 2B-C), SMA, and CD45 (data not shown), suggesting that undifferentiated VPCs gave rise to cell types other than vascular cells. Lee et al9 reported that unregulated VEGF expression in myocardium led to the formation of hemangioma.10 As shown panels E and F of Figure 2, within the newly formed blood vessels with LacZ+ VPC-derived cells, circulating LacZ− blood cells were clearly detected, indicating integration with the systemic circulation. We could not detect LacZ+CD45+ blood cells within the vessel lumen (data not shown). Circulating LacZ+ blood cells were not detected by FACS analysis (data not shown). Implantation of VE-cadherin+ endothelial fraction of differentiated VPCs also generated similar tube structures (Figure 2G) and contributed to the developing capillary network (Figure 2H-I). To investigate the impact of differentiation stages of ES cells for transplantation efficiency, we counted LacZ+PECAM-1+ cells that contributed to vascular structures (Figure 2M). Percentages of LacZ+PECAM-1+ cells to all LacZ+cells were 39.5% ± 14.1% (mean ± SEM; n = 3) in the undifferentiated VPC injection group, 86.9% ± 4.9% in the differentiated VPC group (P < .05 versus undifferentiated VPCs), and 95.3% ± 3.3% in the VE-cadherin+ fraction injection group (P < .05 versus undifferentiated VPCs). In contrast, we did not detect LacZ+ cells within the tumor after the intravenous administration of VPCs.
Characterization of injected ES cell-derived VPCs and transplantation of VPCs in tumor angiogenesis model.
(A-C) Flow cytometric sorting and analysis of Flk-1+undifferentiated VPCs. CCE/nLacZ ES cells were cultured on type IV collagen-coated dishes in the absence of leukemia inhibitory factor (LIF). (A) After 4 days of differentiation, Flk-1+VPCs were sorted by flow cytometry (undifferentiated VPCs). (B-C) Flk-1+ undifferentiated VPCs did not express other EC markers (VE-cadherin, PECAM-1, and CD34). (D-G) After a 3-day incubation of Flk-1+ undifferentiated VPCs, differentiated VPCs were induced. Flow cytometric analysis revealed that about 30% were Flk-1+VE-cadherin+PECAM-1+CD34+ECs and 70% were Flk-1−VE-cadherin−PECAM-1−CD34−(D-E). (F-G) Double staining of differentiated VPCs was performed as previously reported.1 About 70% of cells that lost Flk-1 expression were positive for SMA (brown) and surrounded PECAM-1+ EC sheets (blue). (F) The expressions of PECAM-1 and SMA were exclusive for differentiated VPCs (scale bar, 100 μm). (G) Fluorescent immunostaining of Flk-1 (red) and SMA (green) revealed that they were expressed exclusively (scale bar 20 μm). (H-I) Tumor angiogenesis model of nude mice. Subcutaneous transplantation of VPCs to the growing tumor 7 days after C6 glioblastoma cell implantation was performed (H). Vascularized tumor was obtained 5 days after VPC implantation (I). Monoclonal antibody (MoAb) for murine E-cadherin (epithelial cadherin; ECCD2), Flk-1 (AVAS12), and vascular endothelial (VE)-cadherin (VECD1) have been described previously.6 7Fluorescein isothiocyanate (FITC)-conjugated MoAb for murine PECAM-1 (Mec13.3) and FITC-conjugated MoAb for CD34 (RAM34) were purchased from Pharmingen (San Diego, CA). MoAbs for SMA 1A4, CCA7 were obtained from Neo Markers (Fremont, CA) and ENZO Diagnostics (Farmingdale, NY).
Characterization of injected ES cell-derived VPCs and transplantation of VPCs in tumor angiogenesis model.
(A-C) Flow cytometric sorting and analysis of Flk-1+undifferentiated VPCs. CCE/nLacZ ES cells were cultured on type IV collagen-coated dishes in the absence of leukemia inhibitory factor (LIF). (A) After 4 days of differentiation, Flk-1+VPCs were sorted by flow cytometry (undifferentiated VPCs). (B-C) Flk-1+ undifferentiated VPCs did not express other EC markers (VE-cadherin, PECAM-1, and CD34). (D-G) After a 3-day incubation of Flk-1+ undifferentiated VPCs, differentiated VPCs were induced. Flow cytometric analysis revealed that about 30% were Flk-1+VE-cadherin+PECAM-1+CD34+ECs and 70% were Flk-1−VE-cadherin−PECAM-1−CD34−(D-E). (F-G) Double staining of differentiated VPCs was performed as previously reported.1 About 70% of cells that lost Flk-1 expression were positive for SMA (brown) and surrounded PECAM-1+ EC sheets (blue). (F) The expressions of PECAM-1 and SMA were exclusive for differentiated VPCs (scale bar, 100 μm). (G) Fluorescent immunostaining of Flk-1 (red) and SMA (green) revealed that they were expressed exclusively (scale bar 20 μm). (H-I) Tumor angiogenesis model of nude mice. Subcutaneous transplantation of VPCs to the growing tumor 7 days after C6 glioblastoma cell implantation was performed (H). Vascularized tumor was obtained 5 days after VPC implantation (I). Monoclonal antibody (MoAb) for murine E-cadherin (epithelial cadherin; ECCD2), Flk-1 (AVAS12), and vascular endothelial (VE)-cadherin (VECD1) have been described previously.6 7Fluorescein isothiocyanate (FITC)-conjugated MoAb for murine PECAM-1 (Mec13.3) and FITC-conjugated MoAb for CD34 (RAM34) were purchased from Pharmingen (San Diego, CA). MoAbs for SMA 1A4, CCA7 were obtained from Neo Markers (Fremont, CA) and ENZO Diagnostics (Farmingdale, NY).
Contribution of ES cell-derived VPCs to tumor angiogenesis.
(A,D,G,J) Whole-mount X-gal staining of the tumor. An X-gal analog, blue gal (Nacalai), was used as a substrate for staining 5 days after the injection of undifferentiated VPCs (A), differentiated VPCs (D), VE-cadherin+ fraction of differentiated VPCs (G), and PDGF-BB–treated VPC (J). Undifferentiated VPCs and PDGF-BB–treated VPCs formed cell aggregates with few vascular structures (A,J). Differentiated VPCs and VE-cadherin+fraction of differentiated VPCs generated rich vascular-like networks (D,G). (B,C,E,F,H,I,K-O) Immunohistochemical staining of tumor sections. Differentiated VPCs were specifically incorporated as LacZ (blue)/PECAM-1 (brown) double-positive cells into developing vasculatures (E-F). Undifferentiated VPCs were often detected as LacZ+/PECAM-1− cells (arrows; B-C). Implantation of VE-cadherin+Flk-1+ fraction of differentiated VPCs similarly generated specific vascular contribution as LacZ/PECAM-1 double-positive cells (H-I). Typical LacZ+PECAM-1+ cells (M) were observed in the differentiated VPC-injected tumor. LacZ (blue)/SMA (purple) double-positive and PECAM-1 (brown)-negative cells were also detected in the continuous sections (N-O). In the PDGF-BB–treated VPC transplantation group, some LacZ (blue)/SMA (red) double-positive cells were detected (K-L). Scale bars: panels B, E, H, K, 250 μm; panels C, F, I, L, 50 μm; panel M, 100 μm; panels N-O, 25μm.
Contribution of ES cell-derived VPCs to tumor angiogenesis.
(A,D,G,J) Whole-mount X-gal staining of the tumor. An X-gal analog, blue gal (Nacalai), was used as a substrate for staining 5 days after the injection of undifferentiated VPCs (A), differentiated VPCs (D), VE-cadherin+ fraction of differentiated VPCs (G), and PDGF-BB–treated VPC (J). Undifferentiated VPCs and PDGF-BB–treated VPCs formed cell aggregates with few vascular structures (A,J). Differentiated VPCs and VE-cadherin+fraction of differentiated VPCs generated rich vascular-like networks (D,G). (B,C,E,F,H,I,K-O) Immunohistochemical staining of tumor sections. Differentiated VPCs were specifically incorporated as LacZ (blue)/PECAM-1 (brown) double-positive cells into developing vasculatures (E-F). Undifferentiated VPCs were often detected as LacZ+/PECAM-1− cells (arrows; B-C). Implantation of VE-cadherin+Flk-1+ fraction of differentiated VPCs similarly generated specific vascular contribution as LacZ/PECAM-1 double-positive cells (H-I). Typical LacZ+PECAM-1+ cells (M) were observed in the differentiated VPC-injected tumor. LacZ (blue)/SMA (purple) double-positive and PECAM-1 (brown)-negative cells were also detected in the continuous sections (N-O). In the PDGF-BB–treated VPC transplantation group, some LacZ (blue)/SMA (red) double-positive cells were detected (K-L). Scale bars: panels B, E, H, K, 250 μm; panels C, F, I, L, 50 μm; panel M, 100 μm; panels N-O, 25μm.
Interaction between ECs and MCs is essential for vascular development and maintenance of vascular integrity.11 12 Because differentiated VPCs contained substantial numbers of SMA+Flk-1− MCs, we examined the participation of the MC component to pericyte recruitment during tumor neoangiogenesis. LacZ+SMA+PECAM-1− cells were detected in differentiated VPC-injected tumors (Figure 2N-O). In differentiated VPC transplantation, however, the ratio of LacZ+SMA+ cells to total LacZ+cells was much lower than that of LacZ+PECAM-1+cells. To analyze the in vivo survival/proliferation potential of MCs, we performed selective induction of Flk-1−SMA+cells from Flk-1+ cells with PDGF-BB and transplanted them into the tumor. Whole-mount LacZ staining of the tumor revealed that transplanted PDGF-BB–treated VPCs remained less than differentiated VPCs and formed cell aggregates (Figure 2J) similar to undifferentiated VPCs (Figure 2A). We detected some LacZ+SMA+ cells (Figure 2K-L) and only a few LacZ+PECAM-1+ cells. Most LacZ+cells were negative for either. This result indicated that although VPC-derived MCs can contribute to the MC component in tumor neoangiogenesis, the in vivo survival/proliferation potential of MCs is not high.
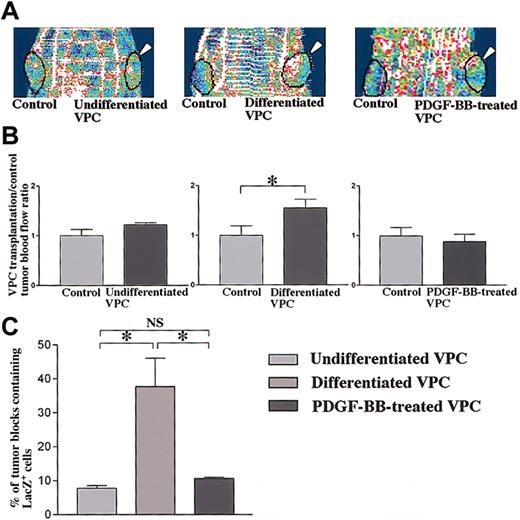
Transplantation of VPCs quantitatively augmented tumor blood flow in nude mice
We further investigated whether transplantation of VPCs might augment blood flow of the tumors. LDPI analyses revealed the significantly augmented ratio of differentiated VPC transplantation to control tumor blood flow (Figure 3A-B), whereas the blood flow ratios of other VPC transplantation groups were not altered. Quantification of the number of tumor blocks containing LacZ+ cells demonstrated an increase of the extent of vascular expansion (Figure 3C). About 40% of tumor blocks contained LacZ+ cells in the differentiated VPC transplantation group, whereas about 10% of them were seen in other VPC transplantation groups. In our protocol, no significant differences in the tumor weight were observed between control and VPC transplantation tumors among the 3 groups (data not shown).
Augmented blood flow in tumors by subcutaneous transplantation of VPCs and expansion of transplanted VPCs within the tumor
. (A) LDPI analyses of blood flow in 3 VPC transplantation groups. Bilateral generation of C6-derived tumor (black circles) and unilateral transplantation of VPCs (arrowheads) in nude mice is shown. Differentiated VPC transplantation augmented blood flow of tumor (red to white colors) compared with control, whereas undifferentiated and PDGF-BB–treated VPCs did not (blue to green colors). (B) Quantitative analyses demonstrated the significant enhancement of differentiated VPC transplantation/control tumor blood flow ratios in nude mice. Data shown (mean ± SEM) are representative of 3 experiments. *P < .05. (C) Percents of the number of sectioned tumor blocks containing LacZ+ cells. About 40% of tumor blocks contained LacZ+ cells in differentiated VPC transplantation groups, whereas about 10% of them did in other VPC transplantation groups. The number of tumor blocks containing LacZ+ cells in differentiated VPC transplantation groups was significantly increased. Data shown (mean ± SEM) are representative of 3 experiments. *P < .01; NS,P > .05.
Augmented blood flow in tumors by subcutaneous transplantation of VPCs and expansion of transplanted VPCs within the tumor
. (A) LDPI analyses of blood flow in 3 VPC transplantation groups. Bilateral generation of C6-derived tumor (black circles) and unilateral transplantation of VPCs (arrowheads) in nude mice is shown. Differentiated VPC transplantation augmented blood flow of tumor (red to white colors) compared with control, whereas undifferentiated and PDGF-BB–treated VPCs did not (blue to green colors). (B) Quantitative analyses demonstrated the significant enhancement of differentiated VPC transplantation/control tumor blood flow ratios in nude mice. Data shown (mean ± SEM) are representative of 3 experiments. *P < .05. (C) Percents of the number of sectioned tumor blocks containing LacZ+ cells. About 40% of tumor blocks contained LacZ+ cells in differentiated VPC transplantation groups, whereas about 10% of them did in other VPC transplantation groups. The number of tumor blocks containing LacZ+ cells in differentiated VPC transplantation groups was significantly increased. Data shown (mean ± SEM) are representative of 3 experiments. *P < .01; NS,P > .05.
Asahara et al13 first demonstrated the existence of endothelial progenitor cells (EPCs) in the circulation, which are at least in part derived from bone marrow,2 and showed that they can participate in postnatal angiogenesis after intravenous administration.13 In our present study, intravenously administrated ES cell–derived VPCs did not contribute to tumor neoangiogenesis, suggesting that ES cell-derived VPCs might be different from somatic circulating endothelial progenitors especially in recruitment and adhesion property. EPCs were characterized as CD34+Flk-1+AC133+cells.13-15 These precursors differentiated into Flk-1+AC133− acetyl low-density lipoprotein (LDL) incorporated-positive ECs.3,14-16 Our ES cell-derived VPCs are Flk-1+CD34− and can differentiate into both MCs and ECs.1 Thus, VPCs are supposed to be more premature precursors. Our results demonstrate that these undifferentiated VPCs cannot be specifically differentiated into ECs and MCs in vivo. However, differentiated VPCs, that is, VPC-derived vascular cells (ECs and MCs) at defined differentiation stages can contribute to tumor-associated vasculoangiogenesis.
The results of the present study clearly demonstrate that differentiated vascular cells derived from VPCs can contribute to generation of vascular structures in adult neoangiogenesis. Optimization of the differentiation stage of ES cells at transplantation is thus critically required to meet the challenge for cell therapy in regeneration medicine.
Prepublished online as Blood First Edition Paper, December 12, 2002; DOI 10.1182/blood-2002-06-1877.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Hiroshi Itoh, Department of Medicine and Clinical Science, Kyoto University Graduate School of Medicine, 54 Shogoin Kawahara-cho, Sakyo-ku, Kyoto 606-8507 Japan; e-mail:hiito@kuhp.kyoto-u.ac.jp.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal