Abstract
P230 Bcr/Abl has been associated with indolent myeloproliferative disease (MPD). We generated transgenic mice expressing P230Bcr/Abl driven by the promoter of the long terminal repeat of the murine stem cell virus of the MSCV neo P230 BCR/ABL vector. Two founder mice exhibited mild granulocytosis and marked thrombocytosis and developed MPD. The disease of one founder mouse, no. 13, progressed to extramedullary myeloblastic crisis in the liver at 12 months old. The other founder mouse, no. 22, was found to have chronic-phase MPD with large populations of megakaryocytes and granulocytes in an enlarged spleen. The transgenic progeny of no. 22 clearly exhibited MPD at 15 months old. These results showed that P230Bcr/Abl had leukemogenic properties and induced MPD. The phenotype of the MPD caused by P230Bcr/Abl was characterized by mild granulocytosis, a high platelet count, infiltration of megakaryocytes in some organs, and a longer disease latency compared with the MPD caused by P210Bcr/Abl. (Blood. 2003;102:320-323)
Introduction
The Bcr/Abl oncogene is formed by reciprocal translocation between chromosomes 9 and 22 and is associated with diverse human leukemias.1 Three different forms of Bcr/Abl are associated with distinct forms of leukemia.2,3 Recently, a subset of patients was described who had Ph-positive myeloproliferative diseases (MPDs) resembling chronic myeloid leukemia (CML) but with very mild clinical symptoms, including a lower peripheral white blood cell (WBC) count consisting principally of neutrophilia, more severe thrombocytosis, less severe anemia, and delayed or absent transformation to blast crisis.4 These patients have a unique chimeric Bcr/Abl protein, P230 Bcr/Abl, that is formed with a breakpoint (μ breakpoint) located 3′ to the common breakpoints.5 It was proposed that patients with P230 Bcr/Abl comprise a distinct clinical entity having a much more benign clinical course than that associated with the traditional P210 Bcr/Abl protein.6 P230Bcr/Abl protein contains additional Bcr coding sequences that are not found in P210 Bcr/Abl protein. These observations raise the question of whether different forms of the Bcr/Abl protein have intrinsically different leukemogenic activities in hematopoietic cells. Recently, there were 2 reports of mouse models created using in vitro retroviral-mediated gene transfer into hematopoietic cell lines and a primary bone marrow transplantation system.7,8
To gain more insight into the molecular pathological function of P230 Bcr/Abl and its in vivo leukemogenic activity, we generated transgenic mice expressing P230 Bcr/Abl and investigated its leukemogenic activity and the disease phenotype.
Study design
Construction of the transgene and generation of MSCVneoP230 BCR/ABL transgenic mice
The MSCVneoP230 BCR/ABL vector, which was kindly provided by Dr R. Van Etten, Harvard Medical School, was cut at the PvuI and SspI sites (Figure 1A).7,9 The DNA fragment containing the long terminal repeats (LTRs) of murine stem cell virus (MSCV) (denoted as PCMV) and P230 BCR/ABL was microinjected into the pronuclei of eggs from C57BL/6N Crj mice. The methods of microinjection and embryonal transfer were essentially described earlier.10 Transgenic mice were identified by polymerase chain reaction (PCR). Genomic DNA from tail-cut biopsy was subjected to PCR reaction. A 1020-base PCR product was identified as positive. Transgenic mice were also identified by Southern blotting of the DNA from tail-cut or spleen biopsy.11
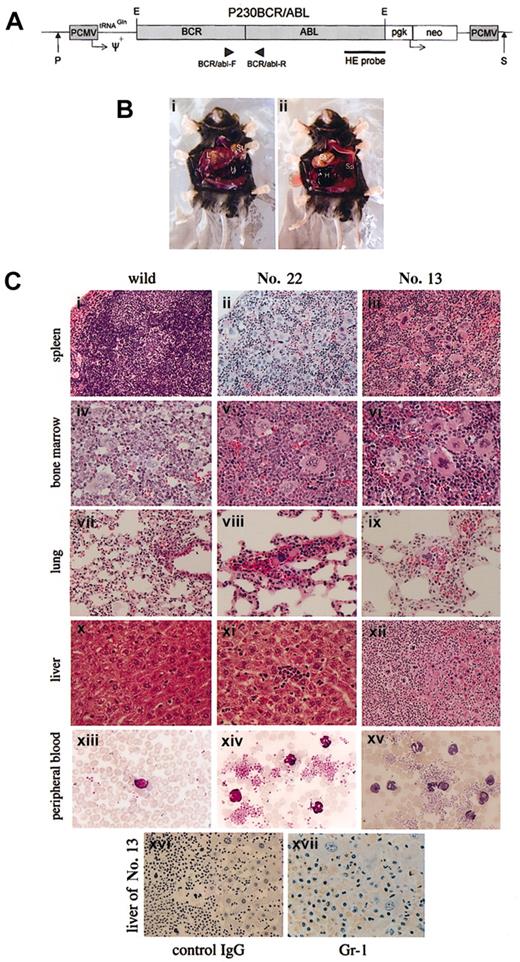
Schematic representation of the MSCVneo P230 BCR/ABL vector and macroscopic and histopathologic findings of founder mice no. 13 and no. 22. (A) The injection fragment for generating transgenic mice was made by cutting at PvuI and SspI sites of the bacterial plasmid, pUC19. Two vertical arrows indicate the cutting sites. P indicates PvuI; S, SspI. The nucleotide sequences of the primers for PCR were as follows: BCR/abl-F: 5′-TGACCAACTCGTGTGTGAAACTCCAG-3′; and BCR/abl-R: 5′-CAGCAGATAC TCAGCGGCATTG-3′. (B) Macroscopic appearance of founder mouse no. 13 in the extramedullary blastic phase of MPD. (i) A markedly enlarged liver and a large volume of hemorrhage in the peritoneal cavity are seen. (ii) After removal of the liver, the enlarged spleen is visible. (C) Histopathologic findings of founder mice no. 13 and no. 22. Photomicrographs of hematoxylin and eosin-stained spleen (i-iii), bone marrow (iv-vi), lung (vii-ix), and liver (x-xii); Wright-Giemsa-stained peripheral blood (xiii-xv); from no. 22 (ii,v,viii,xi,xiv), no. 13 (iii,vi,ix,xii,xv-xvii), and a nontransgenic littermate mouse killed at 12 months of age (i,iv,vii,x,xiii). Panels xvi and xvii show the immunohistochemical findings of the liver stained with Gr-1 (xvii) and control IgG (xvi). Blasts were positive for Gr-1. Original magnifications: × 200 (i-iii); × 1000 (panels xiii-xv); × 400 (iv-xii, xvi); and × 800 (xvii).
Schematic representation of the MSCVneo P230 BCR/ABL vector and macroscopic and histopathologic findings of founder mice no. 13 and no. 22. (A) The injection fragment for generating transgenic mice was made by cutting at PvuI and SspI sites of the bacterial plasmid, pUC19. Two vertical arrows indicate the cutting sites. P indicates PvuI; S, SspI. The nucleotide sequences of the primers for PCR were as follows: BCR/abl-F: 5′-TGACCAACTCGTGTGTGAAACTCCAG-3′; and BCR/abl-R: 5′-CAGCAGATAC TCAGCGGCATTG-3′. (B) Macroscopic appearance of founder mouse no. 13 in the extramedullary blastic phase of MPD. (i) A markedly enlarged liver and a large volume of hemorrhage in the peritoneal cavity are seen. (ii) After removal of the liver, the enlarged spleen is visible. (C) Histopathologic findings of founder mice no. 13 and no. 22. Photomicrographs of hematoxylin and eosin-stained spleen (i-iii), bone marrow (iv-vi), lung (vii-ix), and liver (x-xii); Wright-Giemsa-stained peripheral blood (xiii-xv); from no. 22 (ii,v,viii,xi,xiv), no. 13 (iii,vi,ix,xii,xv-xvii), and a nontransgenic littermate mouse killed at 12 months of age (i,iv,vii,x,xiii). Panels xvi and xvii show the immunohistochemical findings of the liver stained with Gr-1 (xvii) and control IgG (xvi). Blasts were positive for Gr-1. Original magnifications: × 200 (i-iii); × 1000 (panels xiii-xv); × 400 (iv-xii, xvi); and × 800 (xvii).
Flow cytometric analysis
The method of fluorescence-activated cell sorter (FACS) analysis was as described earlier.12 Mononuclear blastic cells that had infiltrated in the liver of no. 13 were obtained by twice Ficoll-Hypaque centrifugation (Lymphoprep, Neegard, Norway) and incubated with a phycoerythrin (PE)- or fluorescein isothiocyanate (FITC)-conjugated monoclonal antibody (MoAb) and analyzed with a FACScan (Becton Dickinson, San Jose, CA). FITC- or PE-conjugated antibodies specific for CD45R/B220, Ly-6G (Gr-1), CD11b (Mac-1), CD34, CD3-ϵ, CD61, and TER119 (BD Pharmingen, San Diego, CA) were used.
Southern and Northern blot analyses
Western blotting and in vitro kinase assays
The methods were as described previously.14 Briefly, tissues were homogenized in RIPA lysis buffer with 1 mM phenylmethylsulfonyl fluoride (PMSF), 50 μg/mL antipain, 5 μg/mL aprotinin, and 2 μg/mL leupeptin.12 For detecting the p230bcr/abl transgene product, proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), transferred to nitrocellulose membranes, and probed with an anti-c-Abl MoAb, AB3 (Oncogene Science, Manhasset, NY). For in vitro kinase assay, 1 mg aliquots of total proteins were incubated with 1:200-diluted AB3 and antimouse rat immunoglobulin G (IgG) (Sigma, St Louis, MO) coupled with protein A (Sigma). The immunoprecipitated proteins were washed and then incubated with 10 μCi (0.37 MBq) γ32P-adenosine triphosphate (γ32P-ATP) (Amersham, Arlington Heights, IL). The phosphorylated proteins were separated by SDS-PAGE, dried, and autoradiographed.
Results and discussion
Two founder mice developed MPD
We generated 2 founder mice, no. 13 and no. 22, that developed MPD. The WBC, platelet (Plt), and hemoglobin (Hb) were within their normal ranges until 7 months after birth. However, thereafter the Plt counts gradually increased. At 11 months after birth, WBC, Hb, and Plts of no. 13 were 6.5 × 109/L(65 × 102/μL), 99 g/L(9.9 g/dL), and 1867 × 109/L (186.7 × 104/μL), and at 12 months those of no. 22 were 9.1 × 109/L (91 × 102/μL), 92 g/L (9.2 g/dL), and 2437 × 109/L (243.7 × 104/μL), respectively. At 12 months after birth, no. 13 suddenly became moribund and subsequently died, and no. 22 was killed. At autopsy, no. 13 showed marked hepatomegaly with liver bleeding, splenomegaly, and ascites (Figure 1B). No. 22 was found to have marked splenomegaly and an enlarged liver.
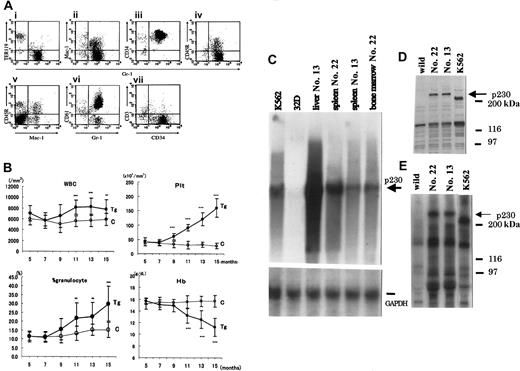
Pathological examination revealed extramedullary expansion of the blastic cells in the liver of no. 13 (Figure 1Cxii). Many immature and mature granulocytes and many megakaryocytes were detected in the bone marrow, spleen, liver, and lung of both mice (Figure 1C). Blast cells were separated from the enlarged liver of no. 13, stained with MoAbs, and analyzed by the FACScan and immunohistopathological methods. The blasts were positive for CD34, Gr-1, and CD61 and partially positive for CD11b and CD45R (Figures 1Cxvii and 2A).
FACS analysis of leukemic mononuclear cells infiltrating the liver of founder mouse no. 13, comparison of hematologic parameters of transgenic progeny of no. 22, and molecular certification of p230 Bcr/Abl expression. (A) Surface marker analysis of leukemic cells infiltrating the liver of founder no. 13. (B) Comparison of hematologic parameters in the transgenic mice (n = 20; Tg, •) and nontransgenic controls (n = 10; C, ○) from 5 months to 15 months. The data are shown as the mean values and standard deviations for each group. Time course of WBC count, platelet (Plt) count, the percentage (%) of granulocytes, and hemoglobin (Hb) are shown. **P < .01; ***P < .001. (C) Northern blot analysis of p230 Bcr/Abl mRNA in tissues from no. 13 and no. 22 offspring. Lane K562: K562 cells as positive control; lane 32D: mouse 32D cells as negative control; lane liver no. 13: liver cells of no. 13; lane spleen no. 22: spleen cells of no. 22; lane spleen no. 13: spleen cells of no. 13; lane bone marrow no. 22: bone marrow cells of no. 22. The bottom bar shows the bands of glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mRNA as an internal control. (D) P230 Bcr/Abl transgene product and (E) kinase activity of the p230 Bcr/Abl transgene product of the splenic cells. The expressed and phosphorylated P230 Bcr/Abl transgene products are indicated by arrows, and the positions of protein markers are shown on the right. The splenic cells of a 3-month-old F1 transgenic mouse were subjected to Western blot and immunoprecipitation analyses.
FACS analysis of leukemic mononuclear cells infiltrating the liver of founder mouse no. 13, comparison of hematologic parameters of transgenic progeny of no. 22, and molecular certification of p230 Bcr/Abl expression. (A) Surface marker analysis of leukemic cells infiltrating the liver of founder no. 13. (B) Comparison of hematologic parameters in the transgenic mice (n = 20; Tg, •) and nontransgenic controls (n = 10; C, ○) from 5 months to 15 months. The data are shown as the mean values and standard deviations for each group. Time course of WBC count, platelet (Plt) count, the percentage (%) of granulocytes, and hemoglobin (Hb) are shown. **P < .01; ***P < .001. (C) Northern blot analysis of p230 Bcr/Abl mRNA in tissues from no. 13 and no. 22 offspring. Lane K562: K562 cells as positive control; lane 32D: mouse 32D cells as negative control; lane liver no. 13: liver cells of no. 13; lane spleen no. 22: spleen cells of no. 22; lane spleen no. 13: spleen cells of no. 13; lane bone marrow no. 22: bone marrow cells of no. 22. The bottom bar shows the bands of glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mRNA as an internal control. (D) P230 Bcr/Abl transgene product and (E) kinase activity of the p230 Bcr/Abl transgene product of the splenic cells. The expressed and phosphorylated P230 Bcr/Abl transgene products are indicated by arrows, and the positions of protein markers are shown on the right. The splenic cells of a 3-month-old F1 transgenic mouse were subjected to Western blot and immunoprecipitation analyses.
The clinical course and the results of these analyses showed that the disease of no. 13 had the characteristics of MPD with extramedullary blastic proliferation in the liver and that no. 22 mimicked the cardinal features of the chronic phase of human CML.
The transgenic progeny of no. 22 were maintained under continual observation. The WBC counts mildly increased after 11 months (Figure 2B). As for the differential count of the WBC, a steadily increased percent of granulocytes became apparent after 9 months of age (Figure 2B). The mean Plt counts for the transgenic progeny (n = 20) gradually increased after 9 months of age and reached 200 × 104/μL (Figure 2B).
Expression of the p230Bcr/Abl transgene in transgenic mice
Southern blot analysis confirmed that no. 13 and no. 22 carry 10 and 5 copies of the p230Bcr/Abl transgene, respectively (data not shown). To confirm expression of the p230Bcr/Abl transgene, Northern blotting, Western blotting, and kinase assay were carried out using mRNAs or proteins extracted from the spleen, bone marrow, and liver cells. The p230Bcr/Abl mRNA and tyrosine-phosphorylated P230Bcr/Abl protein were detected in both mRNAs and proteins from no. 13 and the progeny of no. 22 (Figure 2C-E).
Many animal models of CML have proven to be invaluable for improving our understanding of the molecular pathophysiology of P210 Bcr/Abl.15 In transgenic mice, the p210 Bcr/Abl transgenic mouse using the mouse tec promoter system reproducibly developed CML-like disease.14
The present P230 Bcr/Abl transgenic mouse line using the MSCV promoter was characterized by modestly increased peripheral WBC counts (6 × 109 to 9.5 × 109/L [6 × 103 to 9.5 × 103/μL]) composed predominantly of mature neutrophils, marked thrombocytosis (Plts 1300 × 109 to 3000 × 109/L [130 × 104 to 300 × 104/μL]), and mild anemia (Hb97-127 g/L [9.7-12.7 g/dL]). All the transgenic offspring of no. 22 had an obvious phenotype of CML-like disease by around 15 months of age and showed massive infiltration of megakaryocytes and granulocytes mainly in the spleen and also in the liver and lung. The filial 3 (F3) Tg mice were confirmed to inherit a disease of MPD/CML phenotype. One of the disease phenotypic differences between the P210 and P230 Bcr/Abl transgenic mouse systems was the latency period.14 Latency until manifestation of disease in our transgenic mice was 7 months longer than that in the tec P210 Bcr/Abl system (8 months).14 Another difference was granulocytosis. Granulocytosis was milder than in the P210 Bcr/Abl transgenic mice.14,16 Peripheral thrombocytosis developed in both the P210 Bcr/Abl and the P230 Bcr/Abl transgenic mice, but infiltration of megakaryocytes in the spleen, liver, and lung was a unique characteristic of the P230 Bcr/Abl transgenic mice.14,16
These disease findings of our transgenic mice might be due to the MSCV promoter function or the structure of the p230Bcr/Abl cDNA as well as b3a2-type p210Bcr/Abl cDNA.17 Previous reports suggested a positive correlation between thrombocytosis and the b3a2 type and p230Bcr/Abl type of Bcr/Abl transcripts in human CML.17-19 With its longer disease latency, our transgenic mice develop an MPD disease type with thrombocytosis. In this respect our transgenic mice may more accurately reflect the thrombopoietic characteristics of P230 Bcr/Abl in vivo. Human neutrophilic chronic myelogenous leukemia (CML-N) is known as a CML variant with a more benign clinical course than CML.6,20 Such patients show the disease phenotype of Ph-positive essential thrombocythemia (ET)18,21 or CML with thrombocytosis.22
Another leukemic model using the identical transgene has been reported using in vitro retroviral-mediated gene transfer/transplantation (T/T) system.7 Because the gene constructs used in that study are essentially the same as ours, it is unclear why the mice in these 2 studies showed different disease latency and disease phenotype. One possibility is that, unlike our transgenic mice, the recipient mice in the T/T study were exposed to various cytokines during in vitro culture and also in vivo engraftment, which might accelerate disease onset and affect disease phenotype.
In summary, we present a novel transgenic mouse line created using the P230 Bcr/Abl transgene to develop MPD mimicking CML-N or CML with thrombocytosis. This model will be valuable not only for investigating the biologic properties of P230 Bcr/Abl in vivo but also for analyzing the mechanism involved in the progression from chronic phase to blastic crisis.
Prepublished online as Blood First Edition Paper, March 6, 2003; DOI 10.1182/blood-2002-10-3182.
Supported by a Grant-in-Aid from the Japanese Ministry of Health and Welfare.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked ”advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr R. Van Etten, Harvard Medical School, for providing the MSCVneoP230 BCR/ABL vector. We thank M. Kitoh, H. Yamaguchi, S. Inokuchi, and H. Matsuoka for their expert technical assistance.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal