Abstract
Early neutrophil entry into an inflammatory site is thought to mediate a chemokine switch, inducing subsequent monocyte recruitment through the regulation of monocyte chemoattractant protein-1 (MCP-1) release. As the murine monocyte is poorly characterized and difficult to identify, there has been little examination of either its early recruitment in inflammatory models or of the factors that influence its early migration. The phenotyping of rapidly recruited inflammatory leukocytes with 7/4 and Gr-1 monoclonal antibodies (mAbs) identifies 2 distinct populations, which we characterize as murine monocytes and neutrophils. Monocytes migrate in the first 2 hours of inflammation making use of α4β1 but not of Mac-1 or lymphocyte function-associated antigen-1 (LFA-1) integrins. Early migration is dependent on MCP-1, but neither MCP-1 release nor monocyte recruitment is affected by the reduced neutrophil migration seen in LFA-1-/- mice. Endogenous peritoneal macrophages and mesothelial cells lining the peritoneum contain MCP-1, which is released following thioglycollate stimulation. The murine monocyte therefore responds rapidly to chemokines produced in situ by tissue cells at the site of inflammation with no requirement for prior influx of neutrophils. (Blood. 2003;102:328-335)
Introduction
Neutrophils are recruited rapidly into sites of acute infection and dominate the initial influx of leukocytes.1 Later in inflammation, leukocytes of the monocyte/macrophage lineage replace the neutrophil as the predominant leukocyte, suggesting a bimodal recruitment pattern involving a switch from neutrophils to monocytes. Recruited neutrophils are thought to mediate this switch by releasing soluble factors into the early inflammatory site that initiate monocyte recruitment.2,3 The macrophage plays a central role in the inflammatory response, releasing cytokines that control key events in the initiation, resolution, and repair processes of inflammation (reviewed in Adams and Hamilton4 ). In chronic inflammation, the sustained recruitment of both monocyte/macrophages and neutrophils has been associated with disease, emphasizing the importance of understanding the mechanisms involved in regulating the recruitment of these cells.
To enter inflammatory sites, murine neutrophils use the 2 main β2 integrins, lymphocyte function-associated antigen-1 (LFA-1) (CD11a/CD18) and Mac-1 (CD11b/CD18) together with α4β1 integrin.5 In studies using antibodies to block mononuclear phagocyte migration in vivo, the same integrins (LFA-1, Mac-1, and α4) have been implicated in the rabbit,6 rat,7 and mouse.8,9 Thus there appears to be substantial overlap in the integrins mediating myeloid cell migration.
Neutrophils and monocytes migrate from the circulation across the endothelium into tissues in response to endothelial cell–bound factors, such as chemokines, that deliver activating and chemoattracting signals.10 This critical role of chemokines in the recruitment of myeloid cells is now well established in in vivo murine models.11,12 Murine neutrophils express CXC chemokine receptor 2 and are recruited in response to the CXC ELR+ chemokines, KC and macrophage inflammatory protein 2 (MIP-2),13 whereas monocytes express chemokine receptor 2 that plays a critical role in their response to monocyte chemoattractant protein-1 (MCP-1) (CCR ligand 2, JE).14 The switch from neutrophil to monocyte recruitment in acute peritonitis has been explained by differential release of their respective chemoattractants. According to this model, monocyte migration is dependent on neutrophil-derived factors inducing MCP-1 at the inflammatory site.15-17 Indeed, soluble interleukin-6 (IL-6) receptor, which may be released from infiltrating neutrophils, binds to IL-6 resulting in a complex that promotes local endothelial cells, fibroblasts, or mesothelial cells to both release MCP-1 and down-regulate CXC ELR+ chemokines.15,18,19 However, the limited characterization of the murine monocyte20 has made it difficult to identify recruited monocytes in inflammatory sites and may have led to an underestimation of their early migration.
Here we have characterized circulating murine monocytes and have discovered that, in contrast to previous perceptions, they are recruited rapidly into sites of inflammation, simultaneously with neutrophils. We have analyzed the integrins involved in in vivo monocyte recruitment and found that LFA-1-/- monocytes migrate comparably with LFA-1+/+ monocytes, making use of α4 integrin. We have also examined whether neutrophils have an essential role in inducing monocyte chemotactic signals, thereby initiating monocyte migration in vivo. We conclude that murine monocytes respond to signals derived from endogenous cells at the inflammatory site itself, independently of recruited neutrophils.
Materials and methods
Mice
LFA-1-/-,5 MCP-1-/-,14 and all wild-type mice were bred on the C57BL/6 background. Op/op heterozygote mice were purchased from Jackson Laboratories (Bar Harbor, ME); wild-type and op/op littermates21 were compared in relevant experiments. Sex-matched 8- to 12-week-old mice were used in the experiments. All animal work was performed according to United Kingdom Government Home Office Regulations.
Monoclonal antibodies (mAbs) and the preparation of Fab fragments
The following rat mAbs were used in the in vivo experiments: PS2/3 (α4 integrin, CD49d; immunoglobulin G2b [IgG2b]),22 5C6 (Mac-1, CD11b; IgG2b),9 PyLT-1 (control, antipolyoma large T antigen; IgG2b), and YB238 (control, anti-Ras; IgG2a). All mAbs were prepared under endotoxin-free conditions by Research Monoclonal Antibody Service, Cancer Research United Kingdom. Fab fragments were generated using the ImmunoPure Fab kit as specified by the manufacturer and purified using Protein A Sepharose columns (Perbio Science United Kingdom, Tattenhall, United Kingdom). Contaminating Fc fragments in the Fab preparations were removed by anti–rat IgG2a Fc (TIB173) and anti–rat IgG2b Fc (TIB174) (American Tissue Culture Collection, Rockville, MD) antibody affinity columns, which were generated using the Aminolink Plus Immobilisation kit (Perbio Science United Kingdom) according to manufacturer's instructions. All mAbs and Fabs were assessed by sodium dodecyl sulfate–polyacrylamide gel electrophoresis for purity and ultracentrifuged to remove any aggregated protein.
Flow cytometric analysis
Mouse blood was diluted 1:5 in phosphate-buffered saline (PBS)/1.5% dextran T500 (Amersham Biosciences United Kingdom, Chalfont St Giles, United Kingdom) followed by sedimentation for 30 minutes and further fractionated on Histopaque 1119 (Sigma-Aldrich, Poole, United Kingdom) according to manufacturer's instructions. Bone marrow was prepared by flushing out the femurs and tibias with PBS. Isolated spleens were injected with RPMI 1640 (Life Technologies, Paisley, United Kingdom), liberase purified enzyme blend (1.67 Wunsch U/mL), and DNase (0.2mg/mL) (Roche, Lewes, United Kingdom) and digested for 30 minutes at 37°C. The digested suspension was filtered through a 70-μM nylon filter (BD Biosciences, Oxford, United Kingdom). Red blood cells were then lysed in fluorescence-activated cell-sorter (FACS) Lysing Solution (BD Biosciences).
Peritoneal lavage, blood, bone marrow, and spleen cell preparations were centrifuged and resuspended in FACSwash (PBS, 0.2% bovine serum albumin). Cells (0.5-1 × 106) were treated with mAb 2.4G2 (10 μg/mL; BD Biosciences) for 20 minutes to block Fcγ II/III receptors and stained with conjugated mAbs at an optimal concentration (2-10 μg/mL) for 20 minutes at 4°C, followed by 3 washes in FACSwash. The conjugated antibodies used were as follows (from BD Biosciences unless stated): RB6–8C5–fluorescein isothiocyanate (FITC) or RB6-8C5-biotin (Gr-1), 7/4-phycoerythrin (PE; Caltag, Towcester, United Kingdom), RA3-6B2-biotin (B220), 53.67-biotin (CD8a), PK136-biotin (NK1.1), L3T4-biotin (CD4), M1/70-biotin (CD11b), 9C10-biotin (CD49d), KH74-biotin (I-Ab), ER-MP-20-biotin (Ly-6C, BMA), F4/80-biotin (Serotec, Oxford, United Kingdom), R35-95-biotin (IgG2a isotype), and A95-1-biotin (IgG2bisotype). MAb NIMP-R1423 was obtained from Dr Geoff Butcher (Imperial College, London).
Biotinylated mAb binding to cells was detected by a further incubation with streptavidin tricolor (1:200; Caltag). To detect cytosolic Moma-2, cells were first labeled with mAbs 7/4-PE and Gr-1-biotin followed by streptavidin tricolor (Caltag) then fixed in 4% formaldehyde, permeabilized with 0.5% saponin (Sigma-Aldrich), and labeled with Moma-2–FITC (Serotec) or isotype-FITC control. Following staining, all samples were washed 3 times and resuspended in PBS containing 2% formaldehyde. Cell fluorescence was measured on a FACS Calibur (BD Biosciences). Cells were counted on FACS Calibur by adding a known quantity of calibration beads (CaliBRITE; BD Biosciences) to a known sample volume.
MAb 7/4+ populations were sorted on a Mo-Flo cell sorter (DAKO, Ely, United Kingdom), cytospun onto microscopic slides, and stained with Diffquick according to manufactuer's instructions (Dade Behring, Milton Keynes, United Kingdom).
Peritoneal inflammation
Peritonitis was induced by intraperitoneal injection of sterile thioglycollate (TG) (3% wt/vol in 0.5 mL of sterile saline; Sigma-Aldrich). At various time points, the mice were humanely killed by carbon dioxide exposure and, peritoneal cavities were washed with 5 mL of PBS containing 3 mM EDTA (ethylenediaminetetraacetic acid) and 25 U/mL monoparin (CP Pharmaceuticals, Wrexham, United Kingdom). In some experiments 100 to 400 μg of Fab diluted in 200 μL of PBS was injected intravenously into the tail vein 15 minutes before the TG injection.
Myeloid cell assays
Superoxide production24 and phagocytosis25 were measured as described. Briefly, bone marrow leukocytes (1-2 × 106/mL in Dulbecco modified Eagle medium [DMEM]/10% fetal calf serum [FCS]/10% WEHI 3B conditioned media) were matured by incubation at 37°C, 5% CO2 overnight in Tuf-tainers (Perbio Science United Kingdom).26 For superoxide analysis, matured bone marrow leukocytes (2 × 106/mL in Hanks balanced salt solution) were labeled with 0.1 μM dihydrorhodamine 123 (Cambridge Bioscience, Cambridge, United Kingdom) for 5 minutes at 37°C prior to stimulation with phorbol-12,13 dibutyrate (PDBu; Merck, Nottingham, United Kingdom) at 50 to 200 nM for 30 minutes.24 The superoxide production was analyzed by flow cytometry.
Constitutive phagocytic activity was assayed by incubating matured bone marrow leukocytes (6 × 105 in 150 μL of DMEM 10% FCS) with 150 μL of resuspended fluorescein-conjugated Escherichia coli K-12 particles (Molecular Probes, Cambridge, United Kingdom) at 37°C.25 At 0- to 8-hour time points fluorescence of extracellular bacteria was quenched with trypan blue and extent of phagocytosis was assayed by flow cytometry.
Chemokine analysis
Levels of chemokine MCP-1 were analyzed by enzyme-linked immunosorbent assay according to manufacturer's instructions (R&D Systems, Abingdon, United Kingdom).
Immunohistochemistry
Peritoneal lavage cell samples were cytospun, air dried, and fixed with 2% paraformaldehyde prior to antibody staining. Sagittal sections of the anterior abdominal wall were paraffin embedded; 5 μm sections were microwaved in 0.01 M citrate buffer (pH 6.0) for 10 minutes. Cytospins and peritoneal wall sections were stained with 5 μg/mL rat anti-JE mAb (MCP-1; R&D Systems), control IgG2b mAb (A95-1; BD Biosciences), 5C6 (Mac-1), and F4/80 at identical concentration. Immunohistochemical staining was performed as previously described.27 Positive mAb labeling was revealed with 3,3′-diaminobenzidine staining, and the sections were counterstained with Harris hematoxylin.
Statistics
Data groups were compared using the unpaired Student t test.
Results
Rapid recruitment of 2 distinct 7/4+Gr-1+ populations in murine peritonitis
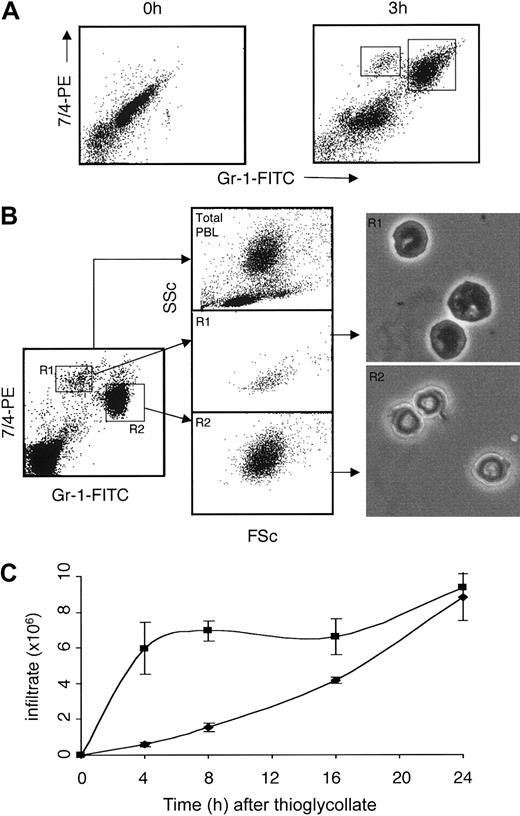
Within 3 hours following the initiation of inflammation, 2 distinct populations of recruited leukocytes are found in the peritoneal cavity (Figure 1A). Peripheral blood neutrophils are characterized by their high flow cytometric side scatter properties (SSc) and can also be distinguished from monocytes and macrophages by higher expression of Gr-1.28 Gating on the 7/4+Gr-1hi population in peripheral blood (R2) confirmed their high SSc, and cytospins of sorted bone marrow populations displayed the characteristic ring-shaped nuclei of the murine neutrophilic granulocytes (Figure 1B).29 The Gr-1int population (R1) had much lower SSc, but were larger than standard polymorphonuclear cells and had ovoid or kidney-shaped nuclei (Figure 1B).
Early recruitment of 2 distinct 7/4+ (Gr-1hi and Gr-1int) populations in murine peritonitis induced with TG. (A) Flow cytometric analysis of 7/4, Gr-1 staining prior to and 3 hours after TG injection. (B) Forward and side scatter properties of total peripheral blood leukocytes, 7/4+Gr-1int (R1), and 7/4+Gr-1hi (R2) populations together with cell morphology of sorted bone marrow populations. Original magnification, × 40. (C) Time course of 7/4+Gr-1hi (▪) and 7/4+Gr-1int (♦) recruitment. Data shown are representative of 3 or more experiments (mean of 5 mice/group, ± SEM).
Early recruitment of 2 distinct 7/4+ (Gr-1hi and Gr-1int) populations in murine peritonitis induced with TG. (A) Flow cytometric analysis of 7/4, Gr-1 staining prior to and 3 hours after TG injection. (B) Forward and side scatter properties of total peripheral blood leukocytes, 7/4+Gr-1int (R1), and 7/4+Gr-1hi (R2) populations together with cell morphology of sorted bone marrow populations. Original magnification, × 40. (C) Time course of 7/4+Gr-1hi (▪) and 7/4+Gr-1int (♦) recruitment. Data shown are representative of 3 or more experiments (mean of 5 mice/group, ± SEM).
The recruitment of these 2 populations into the inflammatory site was rapid. Initially neutrophils (Gr-1hi) were recruited in greater numbers, but the Gr-1int cells steadily increased, with similar numbers of both cell populations present by 24 hours following TG injection (Figure 1C).
Further phenotypic analysis suggests the 7/4+Gr-1int cells are monocytes
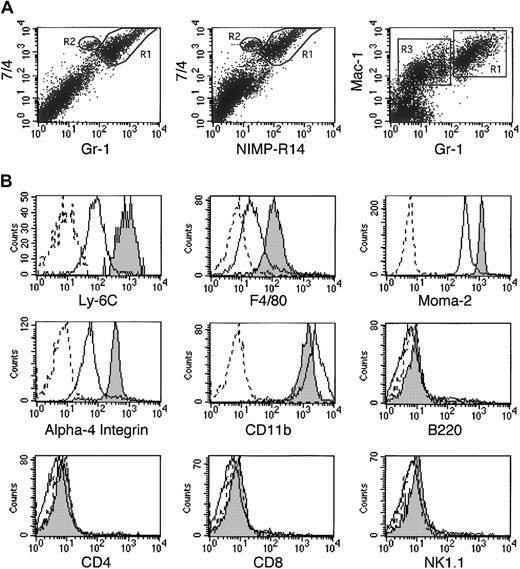
The combination of mAbs 7/4 and Gr-1 identified 2 populations of myeloid cells. The mAb NIMP-R14,23 which has been described as a neutrophil-specific mAb, showed a similar pattern when used in combination with 7/4 (Figure 2A). Furthermore NIMP-R14 blocked the binding of FITC-conjugated Gr-1 to bone marrow cells, indicating that it recognized an identical or overlapping epitope to mAb Gr-1 (data not shown). The 7/4/Gr-1 combination of mAbs allowed easier distinction by flow cytometry of the 2 myeloid populations than the traditional means of using Gr-1 and Mac-1 mAbs to identify monocytes (Gr-1lo, Mac-1hi) and neutrophils (Gr-1hi, Mac-1hi).28
Flow cytometric analysis of 7/4+Gr-1hi and 7/4+Gr-1int bone marrow populations. (A) Flow cytometric analysis of 7/4/Gr-1, 7/4/NIMP-R14 and Mac-1/Gr-1 staining of peritoneal lavage cells 4 hours after TG injection. Gr-1hi neutrophils, R1; 7/4+Gr-1int or NIMP-R14int cells, R2; Mac-1+Gr-1lo monocyte/macrophages, R3. (B) Histograms of 7/4+Gr-1hi (solid line), 7/4+Gr-1int (gray fill), and isotype control (dotted line) are shown. The 7/4+Gr-1int profiles were similar in cells from blood, spleen, and peritoneal lavage (4 hours after TG).
Flow cytometric analysis of 7/4+Gr-1hi and 7/4+Gr-1int bone marrow populations. (A) Flow cytometric analysis of 7/4/Gr-1, 7/4/NIMP-R14 and Mac-1/Gr-1 staining of peritoneal lavage cells 4 hours after TG injection. Gr-1hi neutrophils, R1; 7/4+Gr-1int or NIMP-R14int cells, R2; Mac-1+Gr-1lo monocyte/macrophages, R3. (B) Histograms of 7/4+Gr-1hi (solid line), 7/4+Gr-1int (gray fill), and isotype control (dotted line) are shown. The 7/4+Gr-1int profiles were similar in cells from blood, spleen, and peritoneal lavage (4 hours after TG).
Using the 7/4/Gr-1 mAbs to highlight the Gr-1int population, we examined other phenotypic markers. These cells expressed higher levels of the monocyte/macrophage marker Ly-6C30,31 than neutrophils. MAb F4/80, which stains mature macrophages but is expressed at low levels on circulating monocytes, and Moma-2, a murine macrophage marker expressed by circulating monocytes,31,32 were also higher on the Gr-1int population (Figure 2B). High α4 integrin on the Gr-1int cells again supports the idea that these cells are murine monocytes rather than a subset of neutrophils.
Neither population of recruited cells expressed B220, CD4, CD8, or NK1.1, eliminating B, T, and natural killer (NK) as candidate cell types (Figure 2B). In addition, the Gr-1int population expressed low levels of CD11c, DEC205, major histocompatibility complex (MHC) class II, CD40, B7-1, and B7-2 (data not shown) and expressed high levels of CD11b, making it unlikely that these cells represent a subset of dendritic cells or plasmacytoid dendritic cells, the latter of which are CD11b-. The proportions of the two 7/4+ populations were assessed in the bone marrow, blood, and spleen, confirming that both the Gr-1int and Gr-1hi cells represented significant and distinct populations in all these tissues (Table 1). Furthermore, the degree of mAb staining of the Gr-1int population was similar in these tissues and in the 4-hour lavage, indicating that epitope expression levels were comparable in these sites (data not shown).
Distribution of 7/4+ populations in C57BL/6 mice
Tissue . | % 7/4+Gr-1int . | % 7/4+Gr-1hi . |
|---|---|---|
| Peripheral blood lymphocytes | 3.3 (± 0.5) | 7.3 (± 1.4) |
| Spleen | 0.8 (± 0.2) | 1.3 (± 0.2) |
| Bone marrow | 8.0 (± 1.0) | 27.3 (± 3.5) |
Tissue . | % 7/4+Gr-1int . | % 7/4+Gr-1hi . |
|---|---|---|
| Peripheral blood lymphocytes | 3.3 (± 0.5) | 7.3 (± 1.4) |
| Spleen | 0.8 (± 0.2) | 1.3 (± 0.2) |
| Bone marrow | 8.0 (± 1.0) | 27.3 (± 3.5) |
Average percent ± SD of total leukocyte populations is shown; n = 5.
Functional characterization of the early inflammatory cells
We next examined both the capacity of the 7/4+Gr-1int cells to mature into “elicited” macrophages in vivo and their ability to perform classical macrophage functions after maturation in vitro. Comparison of the Gr-1int cells at 4 hours (R1) and 24 hours (R2) after initiation of inflammation revealed that expression of the 7/4 epitope was reduced as the inflammation progressed (Figure 3A). Furthermore, the size (forward scatter [FSc]) and granularity (SSc) of recruited 7/4+Gr-1int cells increased over the time course of inflammation, indicating that early arriving monocytes were maturing into macrophages (Figure 3A). In addition, after 24 hours of inflammatory stimulus, 7/4+Gr-1int cells increased expression of the macrophage maturation marker F4/80 and the activation markers MHC II, B7-1, and B7-2, providing phenotypic evidence for the transition of these cells into activated macrophages31,32 (Figure 3B). To further establish that the Gr-1int cells (R1) mature into the R2 macrophage population in vivo, sorted Gr-1int cells labeled with Cell Tracker dye were reinjected into mice 4 hours after TG injection. Subsequent analysis of the 24-hour lavage from these mice confirmed that the labeled cells and the R2 population were phenotypically the same (results not shown). Finally following in vitro maturation overnight in IL-3, the 7/4+Gr-1int cells were capable of phagocytosis (Figure 3C) and superoxide burst (Figure 3D), 2 vital macrophage functions. Hence, the 7/4+Gr-1int cells act as precursors of elicited macrophages in vivo, and, when matured, can carry out macrophage functions such as phagocytosis and superoxide burst.
Functional characterization of 7/4+ populations. (A-B) Phenotypic changes of the 7/4+Gr-1int population during inflammation. (A) Down-regulation of 7/4 and increase in scatter properties, 4 hours (R1) and 24 hours (R2) after TG. (B) Up-regulation of activated Mφ markers, 4 hours (R1, solid line), 24 hours (R2, gray fill), and isotype control at 24 hours (dotted line) after TG. (C) Phagocytosis of FITC E coli by matured bone marrow 7/4+Gr-1hi (black) and 7/4+Gr-1int (gray) cells (percent of 7/4+ gate in each quadrant is indicated). (D) Superoxide burst in response to PDBu. Geomean FL-1 values prior to and after stimulation were, respectively, 5.5 (solid line) and 56.7 (gray fill) for Gr-1hi and 8.7 (solid line) and 28.1 (gray fill) for Gr-1int cells.
Functional characterization of 7/4+ populations. (A-B) Phenotypic changes of the 7/4+Gr-1int population during inflammation. (A) Down-regulation of 7/4 and increase in scatter properties, 4 hours (R1) and 24 hours (R2) after TG. (B) Up-regulation of activated Mφ markers, 4 hours (R1, solid line), 24 hours (R2, gray fill), and isotype control at 24 hours (dotted line) after TG. (C) Phagocytosis of FITC E coli by matured bone marrow 7/4+Gr-1hi (black) and 7/4+Gr-1int (gray) cells (percent of 7/4+ gate in each quadrant is indicated). (D) Superoxide burst in response to PDBu. Geomean FL-1 values prior to and after stimulation were, respectively, 5.5 (solid line) and 56.7 (gray fill) for Gr-1hi and 8.7 (solid line) and 28.1 (gray fill) for Gr-1int cells.
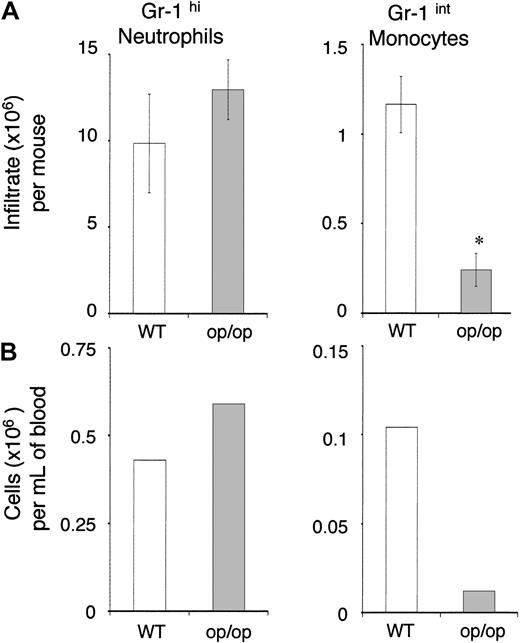
The role of macrophage colony-stimulating factor (M-CSF) as a survival factor in monocyte/macrophage development has been well established. To conclusively confirm that the 7/4+Gr-1int cells were murine monocytes, we examined op/op mice, which have a point mutation in the M-CSF gene and consequently have greatly reduced mononuclear phagocyte numbers.33 Gr-1int cell numbers in these mice were reduced by 79% in the peritoneum (Figure 4A) 6 hours after TG stimulus and by 88% in the blood (Figure 4B), whereas neutrophil numbers remained unchanged. These data confirm the hypothesis that the 7/4+Gr-1int cells are murine monocytes.
Reduction of 7/4+Gr-1int cells in M-CSF–deficientop/opmice. 7/4+Gr-1hi neutrophils and 7/4+Gr-1int monocytes (A) in 6 hours peritoneal inflammation and (B) in pooled peripheral blood. Data shown are representative of 2 experiments (*P ≤ .01; mean of 3 mice per group, ± SEM).
Reduction of 7/4+Gr-1int cells in M-CSF–deficientop/opmice. 7/4+Gr-1hi neutrophils and 7/4+Gr-1int monocytes (A) in 6 hours peritoneal inflammation and (B) in pooled peripheral blood. Data shown are representative of 2 experiments (*P ≤ .01; mean of 3 mice per group, ± SEM).
Integrins involved in monocyte recruitment
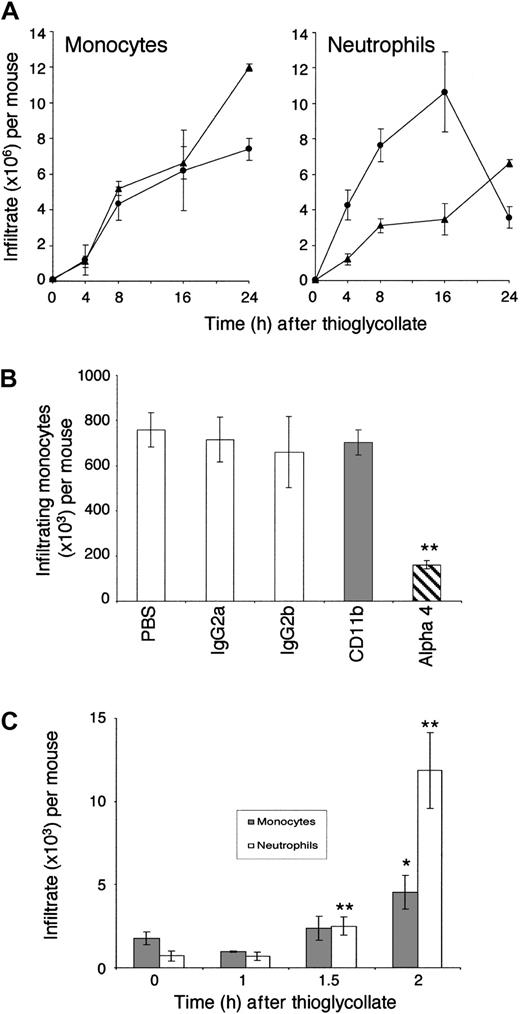
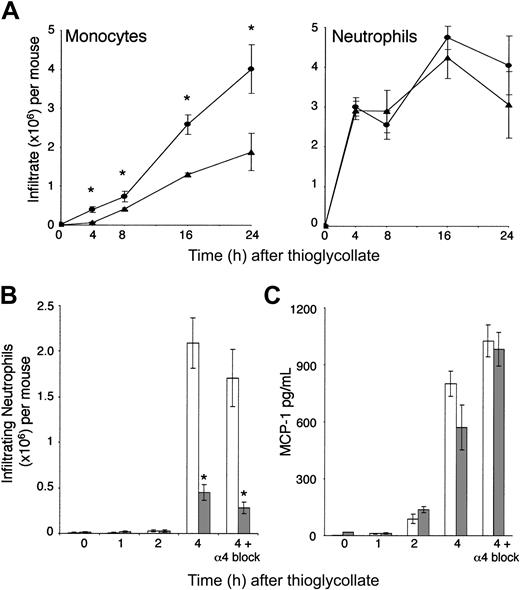
Monocyte recruitment has not previously been analyzed in LFA-1-/- mice in vivo. Although the lack of LFA-1 had a substantial negative effect on neutrophil migration, the early migration of LFA-1-/- monocytes was unaffected when compared with LFA-1+/+ monocytes (Figure 5A). There was a 1.6 (± 0.2)–fold increase in monocyte recruitment at 24 hours in LFA-1-/- compared with LFA-1+/+ mice (n = 3). The reasons for this increase were not explored but could be due to a difference in the chemokines expressed at this later stage of inflammation or to the increased availability of peritoneal tissue space in the absence of neutrophils.
Monocyte recruitment in LFA-1-/- mice. (A) Time course of TG-induced cell recruitment in LFA-1+/+ (•) and LFA-1-/- (▴) mice. (B) The effect on LFA-1-/- monocyte recruitment by purified Fab fragments in vivo. Significant inhibition of monocyte recruitment at 4 hours occurred with mAb PS2/3 (α4) but not with mAb 5C6 (Mac-1, CD11b) when compared with the PBS control. (C) Early monocyte ( ) and neutrophil (□) recruitment in LFA-1-/- mice. Significant recruitment was determined by comparing with the 0-hour control. Data shown are representative of 3 or more experiments (**P ≤ .01; *P ≤ .05; means of 4-6 mice per group, ± SEM).
) and neutrophil (□) recruitment in LFA-1-/- mice. Significant recruitment was determined by comparing with the 0-hour control. Data shown are representative of 3 or more experiments (**P ≤ .01; *P ≤ .05; means of 4-6 mice per group, ± SEM).
Monocyte recruitment in LFA-1-/- mice. (A) Time course of TG-induced cell recruitment in LFA-1+/+ (•) and LFA-1-/- (▴) mice. (B) The effect on LFA-1-/- monocyte recruitment by purified Fab fragments in vivo. Significant inhibition of monocyte recruitment at 4 hours occurred with mAb PS2/3 (α4) but not with mAb 5C6 (Mac-1, CD11b) when compared with the PBS control. (C) Early monocyte ( ) and neutrophil (□) recruitment in LFA-1-/- mice. Significant recruitment was determined by comparing with the 0-hour control. Data shown are representative of 3 or more experiments (**P ≤ .01; *P ≤ .05; means of 4-6 mice per group, ± SEM).
) and neutrophil (□) recruitment in LFA-1-/- mice. Significant recruitment was determined by comparing with the 0-hour control. Data shown are representative of 3 or more experiments (**P ≤ .01; *P ≤ .05; means of 4-6 mice per group, ± SEM).
The surprising lack of a role for LFA-1 in vivo led us to question which integrins are important for monocyte trafficking into an inflammatory site. Mac-1, α4 integrin, and L-selectin expression levels were all similar on LFA-1-/- and LFA-1+/+ monocytes, discounting any obvious compensation in expression due to the lack of LFA-1 (data not shown). Recruitment of LFA-1-/- monocytes at 4 hours after inflammatory stimulus was blocked with the anti-α4 PS2/3 Fab fragment, but surprisingly not with the anti–Mac-1 5C6 Fab fragment (Figure 5B). Effective blocking of Mac-1 sites by saturating amounts of mAb 5C6 on migrated monocytes was confirmed by probing for available Mac-1 using Alexa-conjugated mAb 5C6 (data not shown). In a previous study using the same peritonitis model, mAb 5C6 contributed to the blocking of neutrophil recruitment,5 demonstrating that this Mac-1 mAb is a functional blocker within the context of this model.
Reduced neutrophil recruitment in LFA-1-/- mice does not alter monocyte migration
The observation that monocytes migrated into the inflammatory site at an early stage was unexpected, as it had previously been thought that monocyte recruitment depended on the initial recruitment of neutrophils. It also appeared that the reduced recruitment of neutrophils in LFA-1-/- mice had no overall impact on the levels of monocytes entering the inflammatory site (Figure 5A). We next determined the speed of monocyte and neutrophil recruitment by testing the peritoneal lavage in the LFA-1-/- model at various times. At an early time point between 1.5 to 2 hours, entry of both monocytes and neutrophils is evident (Figure 5C). This observation strongly suggested that monocytes respond to an inflammatory stimulus using a mechanism independent of neutrophil recruitment and that both cell types are simultaneously recruited into the inflammatory site at an early stage.
Chemokine MCP-1 is produced in situ by cells at the inflammatory site
As the importance of MCP-1 in mononuclear phagocyte migration has been established in murine peritonitis using MCP-1-/- mice,14 we used this model to assess the role of MCP-1 in early monocyte recruitment. At 4 hours after the onset of inflammation, monocyte numbers in MCP-1-/- mice were reduced to 16% of wild-type levels, clearly showing that MCP-1 plays a critical role in recruitment during the initial stages of inflammation (Figure 6A). As expected, lack of MCP-1 caused no reduction in neutrophil numbers.
MCP-1 is critical for early monocyte recruitment and is unaffected by deficient neutrophil recruitment. (A) Time course of cell migration in MCP-1+/+ (•) and MCP-1-/- (▴) mice; MCP-1+/+ and MCP-1-/- infiltrating cells were compared at each time point (*P ≤ .05). (B) Reduced neutrophil infiltration in LFA-1-/- ( ) compared with LFA-1+/+ (□) mice, and further reduction with anti-α4 mAb PS2/3, LFA-1+/+, and LFA-1-/- infiltrating cells were compared at each time point (*P ≤ .001). (C) MCP-1 levels in peritoneal lavage of mice (panel B) with blocked neutrophil migration; LFA-1+/+ and LFA-1-/- lavages were compared at each time point (P ≥ .05 for all time points). Data shown are representative of 2 or more experiments (means of 4-5 mice per group ±, SEM).
) compared with LFA-1+/+ (□) mice, and further reduction with anti-α4 mAb PS2/3, LFA-1+/+, and LFA-1-/- infiltrating cells were compared at each time point (*P ≤ .001). (C) MCP-1 levels in peritoneal lavage of mice (panel B) with blocked neutrophil migration; LFA-1+/+ and LFA-1-/- lavages were compared at each time point (P ≥ .05 for all time points). Data shown are representative of 2 or more experiments (means of 4-5 mice per group ±, SEM).
MCP-1 is critical for early monocyte recruitment and is unaffected by deficient neutrophil recruitment. (A) Time course of cell migration in MCP-1+/+ (•) and MCP-1-/- (▴) mice; MCP-1+/+ and MCP-1-/- infiltrating cells were compared at each time point (*P ≤ .05). (B) Reduced neutrophil infiltration in LFA-1-/- ( ) compared with LFA-1+/+ (□) mice, and further reduction with anti-α4 mAb PS2/3, LFA-1+/+, and LFA-1-/- infiltrating cells were compared at each time point (*P ≤ .001). (C) MCP-1 levels in peritoneal lavage of mice (panel B) with blocked neutrophil migration; LFA-1+/+ and LFA-1-/- lavages were compared at each time point (P ≥ .05 for all time points). Data shown are representative of 2 or more experiments (means of 4-5 mice per group ±, SEM).
) compared with LFA-1+/+ (□) mice, and further reduction with anti-α4 mAb PS2/3, LFA-1+/+, and LFA-1-/- infiltrating cells were compared at each time point (*P ≤ .001). (C) MCP-1 levels in peritoneal lavage of mice (panel B) with blocked neutrophil migration; LFA-1+/+ and LFA-1-/- lavages were compared at each time point (P ≥ .05 for all time points). Data shown are representative of 2 or more experiments (means of 4-5 mice per group ±, SEM).
If neutrophils are responsible for inducing the MCP-1 necessary for early monocyte recruitment, we reasoned that preventing neutrophil entry into the inflamed site should diminish MCP-1 expression. To test this hypothesis we analyzed the induction of MCP-1 in vivo in the LFA-1-/- mouse where neutrophil recruitment is reduced by 78% at 4 hours (Figure 6B). As some neutrophils are still recruited in the LFA-1-/- mouse, we further inhibited their numbers using a blocking mAb against α4 integrin, which limited neutrophil recruitment by 87% of that seen in the untreated LFA-1+/+ mouse (Figure 6B). Surprisingly there was no significant difference in MCP-1 levels despite the reduced neutrophil recruitment (Figure 6C), suggesting that endogenous peritoneal cells are directly capable of producing MCP-1 in response to inflammatory stimuli with no requirement for prior neutrophil migration.
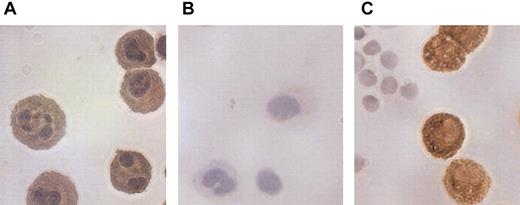
Expression of MCP-1 by peritoneal cells
To identify the cellular source of MCP-1 in the peritoneum, we analyzed resident peritoneal cells and tissues by immunohistochemistry. Peritoneal lavage cells were cytospun and tissue sections were prepared from peritoneal wall tissue. Large cells present in the lavage strongly expressed MCP-1 compared with isotype control (Figure 7A-B) and also expressed F4/80 (Figure 7C) and Mac-1 (data not shown), indicating that they were resident peritoneal macrophages. In agreement with this conclusion, cytospins from macrophage-deficient op/op mice showed minimal staining with either MCP-1 or F4/80 (data not shown). MCP-1 was also expressed, but less strongly, by the mesothelial cells lining the peritoneum (data not shown).
Chemokine MCP-1 expression in peritoneal macrophages. Immunohistochemical analysis of (A) MCP-1 expression in untreated endogenous peritoneal macrophages using anti–MCP-1 mAb. (B) IgG2b control mAb. (C) F4/80 mAb selective for murine macrophages. Original magnification, × 40.
Chemokine MCP-1 expression in peritoneal macrophages. Immunohistochemical analysis of (A) MCP-1 expression in untreated endogenous peritoneal macrophages using anti–MCP-1 mAb. (B) IgG2b control mAb. (C) F4/80 mAb selective for murine macrophages. Original magnification, × 40.
Discussion
Here we have defined the murine monocyte by both flow cytometry and functional analysis. Identification of the monocyte as a rapidly recruited cell at sites of inflammation has been lacking because of the difficulty in distinguishing murine monocytes from other cells types, particularly elicited neutrophils and resident macrophages. Previously the Gr-1 epitope together with Mac-1 have been used to distinguish neutrophils and monocyte/macrophages.28 As macrophages, monocytes, and a subset of B cells all express Mac-1, it is not possible to distinguish between these cell types using this combination of markers. In this study we use 7/4 and Gr-1 mAbs to distinguish monocytes from macrophages, B cells, and neutrophils in bone marrow, spleen, blood, and inflammatory infiltrates.
In humans, several subsets of monocytes have been characterized.34 As staining murine samples with a panel of antibodies failed to subdivide the monocyte population, this study suggests that all murine monocytes are recognized using the combination of 7/4 and Gr-1 epitope markers and that they are a homogeneous group of cells in terms of phenotype. The possibility remains, however, that further phenotyping will reveal the monocytes identified here to be heterogeneous with distinct subsets.
MAbs 7/4, NIMP-R14, and Gr-1 have all been used to define or deplete the neutrophil lineage in mice, with assessment of consequences on the function of not only macrophages but also lymphocytes.35-39 As all 3 mAbs recognize monocytes, their removal as well as the expected removal of the neutrophils could influence the outcome of any such experiment. Of interest is the observation that the Ly-6G–specific mAb 1A8 reacts with neutrophils but not with the Gr-1int cells.40 This mAb is therefore a more useful marker of the neutrophil lineage than either 7/4, Gr-1, or NIMP-R14 (supplemental figure on the Blood website; see the Supplemental Figure link at the top of the online article).
To evaluate the characteristics of monocyte recruitment to an in vivo inflammatory site, we first investigated the role of integrins LFA-1, Mac-1, and α4 integrin, all of which have been implicated in this process. Using an LFA-1-/- model, we had previously demonstrated the dependence of migrating murine neutrophils on LFA-1.5 Unlike neutrophils, however, recruitment of monocytes was not reduced in LFA-1-/- mice when compared with wild-type mice. In support of these findings, murine macrophage migration was unaltered in LFA-1-/- compared with wild-type mice in in vitro migration assays.8 In the absence of LFA-1, monocytes were able to use α4 integrin for migration. A prominent role for α4 integrin, but not β2 integrins, has also been revealed in intravital experiments examining adhesion of green fluorescent protein–expressing monocytes directly to the atherosclerotic vasculature.41 We found no essential role for the β2 integrin Mac-1 in contrast to studies in rats7 and mice8,9 that have established a role for Mac-1 in monocyte migration. It cannot be discounted that monocytes in different species and models of inflammation may have a requirement for LFA-1 and or Mac-1, which is not evident in murine peritonitis.
Other issues may also be relevant in evaluating the participation of individual integrins in particular monocyte functions. A number of previous studies have relied on blocking antibodies, which are often used as intact IgGs. In our experiments monocyte, unlike neutrophil, migration was strongly inhibited by several intact rat IgG2b mAbs, but not by the corresponding Fab fragments. In order to ensure that the effect of intact rat IgG2b was eliminated, it was found essential to use an anti-IgG2b affinity column in order to remove traces of all Fc fragments from the generated Fab fragments. Circulating mouse monocytes express low levels of FcγRI (data not shown), and rat IgG2b antibodies have been shown to bind through FcγRI to human monocytes.42 Furthermore, in our experiments 2 rat IgG2b mAbs, 5C6 and 2.4G2 (anti-CD16/32), inhibited binding of murine monomeric IgG2a to the mouse FcγRI receptor on murine monocytes (results not shown). These results suggest that there is a significant inhibitory effect of intact rat IgG2b mAbs on monocyte migration, probably mediated through Fc receptors. It is therefore essential to use Fab fragments, particularly of rat IgG2b mAbs, in monocyte functional assays.
The first easily recognizable mononuclear phagocyte in the peritoneum has been the more mature, elicited macrophage, which, as this study shows, develops phenotypically over the initial 24-hour period following the inflammatory stimulus. It was unexpected that significant numbers of monocytes were rapidly recruited simultaneously with neutrophils into the inflamed site within the first 2 hours of inflammation. One reason for the previous failure to appreciate this early monocyte recruitment is undoubtedly because of the past difficulty in distinguishing murine monocytes from neutrophils. Such experiments have given rise to the conclusion that neutrophils play a causal role in the recruitment of macrophages to an inflammatory site. Where mAbs such as 7/4 or NIMP-R14 are used as cell depletion reagents, monocytes as well as neutrophils would be affected by the treatment, with the negative effect on macrophage numbers most likely accounted for by the lack of elicited monocytes, not neutrophils
In general, the major chemokine responsible for recruiting monocytes to inflammatory sites is the CC chemokine MCP-1, and we show that MCP-1 is the critical chemokine mediating early monocyte recruitment in murine peritonitis. This raises the issue as to which cells are responsible for promoting the synthesis of this chemokine. Although not previously directly analyzed in vivo, the perception has been that neutrophils are instrumental in mediating a chemokine switch promoting monocyte chemoattraction (reviewed in Kaplanski et al17 ). In this model, neutrophils down-regulate their own migration and up-regulate subsequent monocyte recruitment by switching chemokine production from CXC ELR+ chemokines (IL-8 and Gro α in humans; KC and MIP-2 in mice) to monocyte-recruiting CC chemokines such as MCP-1.15,16 If recruited neutrophils are responsible for inducing the production of MCP-1, then a lack of neutrophil recruitment should result in failure to activate the chemokine switch leading to decreased MCP-1 expression. However, blocking neutrophil entry into the inflammatory site had no impact on the production of MCP-1 or the recruitment of monocytes.
These results have demonstrated that elicited neutrophils are not responsible for stimulating the MCP-1 synthesis or release, which causes monocyte chemoattraction. We show, however, that the endogenous peritoneal macrophages and to a lesser extent mesothelial lining cells express preformed MCP-1 protein. This finding suggests that resident macrophages and also mesothelial cells contribute to the MCP-1 levels providing an immediate source of MCP-1 for recruitment of monocytes from the circulation at 1.5 to 2 hours following TG stimulus. Previous studies using the air pouch or peritonitis models of inflammation show that MCP-1 induction may be indirect and that tumor necrosis factor α43 or MIP-1α37 can give rise to MCP-1. It therefore seems likely that a mediator is produced as a result of TG stimulus, which secondarily causes MCP-1 release by MCP-1–containing peritoneal cells. Alternatively the TG uptake by these cells, particularly the macrophage itself, might directly cause release of MCP-1.
In summary, evidence is provided that monocytes respond directly and rapidly to the chemoattractant MCP-1 following an inflammatory stimulus. The MCP-1 is produced in situ predominately by tissue macrophages independently of infiltrating neutrophils at a site of inflammation. Monocytes and macrophages participate in both the innate and adaptive immune responses and are sustaining components of chronic inflammatory disease. These advances in identifying the murine monocyte and understanding the mechanism of monocyte recruitment will aid further attempts to control these cells in the inflammatory conditions in which they have a central role.
Prepublished online as Blood First Edition Paper, March 6, 2003; DOI 10.1182/blood-2002-10-3228.
Supported by Cancer Research United Kingdom.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Barrett Rollins for his permission to use the MCP-1 null mice and Geoff Butcher for the NIMP-R14 mAb. We are grateful to Gill Hutchison for careful animal husbandry and George Elia for the immunohistochemistry. We thank our Cancer Research United Kingdom colleague Caetano Reis e Sousa and our Leukocyte Adhesion Laboratory colleagues for their helpful comments on the manuscript.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal