The recent report by Tobin et al1 that chronic lymphocytic leukemia (CLL) patients using the VH3-21 gene segment have a poor prognosis despite mostly having more than 2% VH mutation has generated a considerable amount of interest.2-4 This is partly because such cases constitute an exception to the rule that “mutated” CLL necessarily has a good prognosis, and partly because their poor outcome remains unexplained.
We have previously reported that p53 dysfunction can arise in CLL through inactivating mutation of the genes encoding either p53 or ATM (a kinase that regulates p53) and have devised a simple screening test for these defects.5 The test measures the accumulation of p53 and one of its transcriptional targets (p21) in response to ionizing radiation (IR). Both defects are associated with impaired p21 accumulation. In the type A defect due to p53 mutation, baseline levels of p53 are increased, whereas in the type B defect, due to ATM mutation, baseline p53 is not increased, but IR-induced accumulation is impaired. We have further shown that both defects are, like CD38 expression, largely confined to patients with less than 5% VH mutation and associated with a short survival.6 On the basis of these findings we proposed a prognostic model of CLL in which a 5% VH mutation cut-off separates a homogeneous group of good-risk “mutated” patients from a heterogeneous “unmutated” group. The latter can then be risk-stratified according to the presence or absence of other adverse prognostic factors (eg, p53 dysfunction, CD38 expression) that are confined to this group.
It was of obvious interest to ascertain how CLL patients using VH3-21 fitted into this prognostic model and whether the poor outcome of such patients could be explained by an association with p53 dysfunction or CD38 expression. To do this, we have examined the relationship between VH3-21 usage and VH mutation, p53 dysfunction, and CD38 expression in an updated series of 83 patients with CLL attending the Royal Liverpool University Hospital. The median age at diagnosis was 64 years and the male-to-female ratio was 1.48. The median interval between diagnosis and blood sampling was 26 months. The overall median follow-up was 60 months, and survival data were obtained on all but one patient.
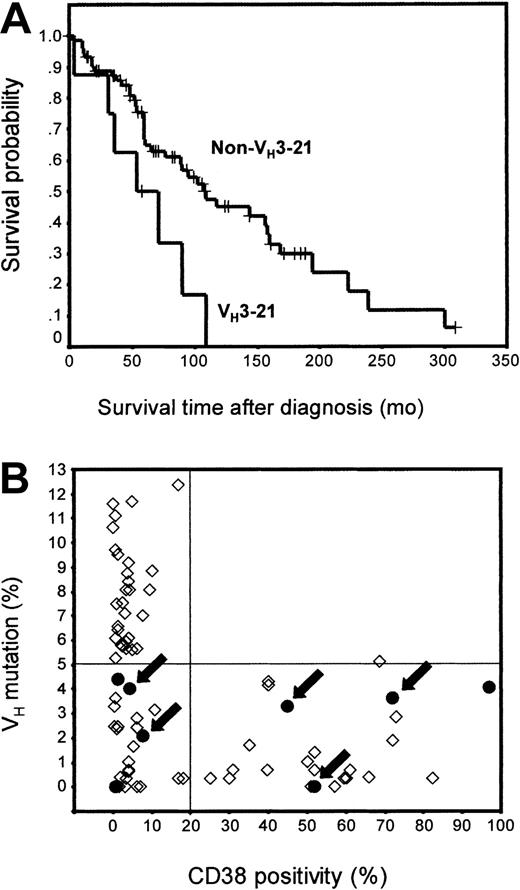
VH3-21 was used in 8 patients (9.6%). In keeping with the findings of Tobin et al,1 the survival of such patients was significantly shorter than that of patients using other VH gene segments (Figure 1A). Two (25%) of the 8 patients using VH3-21 had less than 2% VH mutation, 6 (75%) had 2% to 5% mutation, and none had more than 5% mutation (Figure 1B). In contrast, among the 75 patients with VH segments other than VH3-21, 33 (44%) had less than 2% VH mutation, 12 (16%) had 2% to 5% mutation, and 30 (40%) had more than 5% mutation (Figure 1B). The association between VH3-21 usage and less than 5% VH mutation was found to be statistically significant (P < .05; Fisher exact test). Furthermore, among cases with 5% VH mutation or less, there was a significant association between VH3-21 use and 2% to 5% VH mutation (P < .05). These findings are very much in accordance with the point made by Nollet et al2 that, despite being “mutated” by conventional criteria, most CLL patients using VH3-21 would fall into the “unmutated” category if a higher VH mutation threshold were employed.
Prognostic effect of VH3-21 usage and its association with other prognostic factors. (A) Kaplan-Meier curves showing the overall survival from diagnosis of CLL patients using VH3-21 versus other VH gene segments. The median survival values were 54 and 109 months, respectively (P = .012; log-rank test). The sex ratio and age at diagnosis were not significantly different between the 2 groups (P > .99 and P = .96, respectively; Mann-Whitney U test). (B) Dot-plot showing relationship between VH mutation (y-axis) and CD38 expression (x-axis) among patients using VH3-21 (•) or other gene segments (⋄). VH3-21–using cases with p53 dysfunction are highlighted with arrows.
Prognostic effect of VH3-21 usage and its association with other prognostic factors. (A) Kaplan-Meier curves showing the overall survival from diagnosis of CLL patients using VH3-21 versus other VH gene segments. The median survival values were 54 and 109 months, respectively (P = .012; log-rank test). The sex ratio and age at diagnosis were not significantly different between the 2 groups (P > .99 and P = .96, respectively; Mann-Whitney U test). (B) Dot-plot showing relationship between VH mutation (y-axis) and CD38 expression (x-axis) among patients using VH3-21 (•) or other gene segments (⋄). VH3-21–using cases with p53 dysfunction are highlighted with arrows.
In addition to confirming that VH3-21 usage is associated with short survival and a relatively low level of VH mutation, we also observed a strong association between VH3-21 usage and p53 dysfunction (P < .05; Fisher exact test). Specifically, among the 8 patients using VH3-21, 5 (62%) had a functional defect of the pathway (2 type A, 3 type B) compared with 20 (27%) of the 75 patients using other VH gene segments (10 type A, 10 type B). The higher frequency of p53 dysfunction observed among patients using VH3-21 was not associated with delayed blood sampling relative to patients using other VH gene segments (P = .64; Mann-Whitney U test).
A statistically significant association was not observed between VH3-21 usage and CD38 expression (defined as positivity on more than 20% of CLL cells using the HB7 monoclonal antibody). Thus, among the 8 patients using VH3-21, 4 (50%) expressed CD38, compared with 20 (26.7%) of the 75 patients using other VH gene segments (P = .22; Fisher exact test). However, the high odds ratio (2.75) meant that a β error due to small sample size could not be excluded.
We conclude that CLL patients using VH3-21 fit into our prognostic model extremely well and that their adverse clinical outcome might, at least in part, be due to associated p53 dysfunction.
This work was supported by the Leukaemia Research Fund (United Kingdom).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal